Health Cluster Bulletin 11Ver2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Forecasting Tourists Arrivals at Chinhoyi Caves Recreational Park in Zimbabwe Using SARIMA Model
International Tourism and Hospitality Journal 1(2): 1-10 (2018) Print ISSN: 2616-518X Online ISSN: 2616-4701 RPA ITHJ Journals International Tourism and Hospitality Journal Journal Homepage: https://rpajournals.com/ithj Forecasting Tourists Arrivals at Chinhoyi Caves Recreational Park in Zimbabwe Using SARIMA Model Tendai Makoni*1, Delson Chikobvu2 Bongani Maphosa3 Great Zimbabwe University, Zimbabwe1,3 University of the Free State, South Africa2 Abstract Forecasting tourist arrivals and volatility for Chinhoyi Caves Recreational Parks using SARIMA-GARCH models are vital for decision and planning purposes. The monthly data from the Zimbabwe Parks and Wildlife Management Authority (ZIMPARKS) for the period January 2010 to December 2016 was used. The time series plot indicated mixed fluctuations in tourist arrivals and exhibited seasonality. The series became stationary after a logarithmic transformation and a seasonal difference. The Akaike Information Criteria (AIC) and the Bayesian Information Criterion was used in selecting the best model and a SARIMA(1,0,1)(1,1,0)12 model fitted well to the data. The residuals of the model confirmed to all tests. Accuracy measures like the mean absolute error (MAE) and the mean absolute percentage error (MAPE) supported the model and an out of sample for the next 24 months (2017 to 2018) were done. From the forecasts, an increase in tourist arrivals was noted. The results imply the need for enough accommodation facilities in and around the recreational centre. Keywords: Tourist arrivals, ARIMA models, SARIMA models, time series plot 1 *Corresponding author: Tendai Makoni ; Email: [email protected] Submission Date: 9 June 2018 Acceptance Date: 17 June 2018 Introduction Forecasting is a key tool for planning and decision-making in modern business organisations, according to Thoplan (2014). -
Integrated Testing for TB and HIV Zimbabwe
AUGUST 2019 ZIMBABWE TB AND HIV FAST FACTS 1.3 MILLION PEOPLE LIVING WITH HIV % ADULT HIV 13.3 PREVALENCE (AGES 15–49 YEARS) 37,000 PEOPLE FELL ILL WITH TUBERCULOSIS (TB)* © UNICEF/Costa/Zimbabwe INTEGRATED TESTING FOR TB AND HIV 23,000 USING GENEXPERT DEVICES EXPANDS PEOPLE LIVING WITH HIV ACCESS TO NEAR-POINT-OF-CARE TESTING FELL ILL * LESSONS LEARNED FROM ZIMBABWE WITH TB Introduction With limited funding for global health, identifying practical, cost- and time- OF TB PATIENTS % saving solutions while also ensuring quality of care is evermore important. 63ARE PEOPLE Globally, there are fleets of molecular testing platforms within laboratories WITH KNOWN HIV-POSITIVE and at the point of care (POC), the majority of which were placed to offer STATUS disease-specific services such as the diagnosis of tuberculosis (TB) or HIV in infants. Since November 2015, Clinton Health Access Initiative, Inc. (CHAI), the United Nations Children’s Fund (UNICEF) and the African Society of Laboratory Medicine (ASLM), with funding from Unitaid, have % OF HIV-EXPOSED been working closely with ministries of health across 10 countries in sub- Saharan Africa to introduce innovative POC technologies into national INFANTS 1 63 health programmes. RECEIVED AN HIV TEST WITHIN THE FIRST TWO One approach to increasing access to POC testing is integrated testing MONTHS OF LIFE (a term often used interchangeably with “multi-disease testing”), which is testing for different conditions or diseases using the same diagnostic *Annually platform.2 Leveraging excess capacity on existing devices to enable testing Sources: UNAIDS estimates 2019; World Health across multiple diseases offers the potential to optimize limited human Organization, ‘Global Tuberculosis Report 2018’ and financial resources at health facilities, while increasing access to rapid testing services. -

(Ports of Entry and Routes) (Amendment) Order, 2020
Statutory Instrument 55 ofS.I. 2020. 55 of 2020 Customs and Excise (Ports of Entry and Routes) (Amendment) [CAP. 23:02 Order, 2020 (No. 20) Customs and Excise (Ports of Entry and Routes) (Amendment) “THIRTEENTH SCHEDULE Order, 2020 (No. 20) CUSTOMS DRY PORTS IT is hereby notifi ed that the Minister of Finance and Economic (a) Masvingo; Development has, in terms of sections 14 and 236 of the Customs (b) Bulawayo; and Excise Act [Chapter 23:02], made the following notice:— (c) Makuti; and 1. This notice may be cited as the Customs and Excise (Ports (d) Mutare. of Entry and Routes) (Amendment) Order, 2020 (No. 20). 2. Part I (Ports of Entry) of the Customs and Excise (Ports of Entry and Routes) Order, 2002, published in Statutory Instrument 14 of 2002, hereinafter called the Order, is amended as follows— (a) by the insertion of a new section 9A after section 9 to read as follows: “Customs dry ports 9A. (1) Customs dry ports are appointed at the places indicated in the Thirteenth Schedule for the collection of revenue, the report and clearance of goods imported or exported and matters incidental thereto and the general administration of the provisions of the Act. (2) The customs dry ports set up in terms of subsection (1) are also appointed as places where the Commissioner may establish bonded warehouses for the housing of uncleared goods. The bonded warehouses may be operated by persons authorised by the Commissioner in terms of the Act, and may store and also sell the bonded goods to the general public subject to the purchasers of the said goods paying the duty due and payable on the goods. -

Zimbabwean Government Gazette
A I SET ZIMBABWEAN GOVERNMENT GAZETTE Published by Authority Vol. LXXI, No. 44 2nd JULY. 1993 Price $2,50 i General Notice 384 of 1993. Zimbabwe United Passenger Company. ^^0/226/93. Permit: 15723. Motor-omnibus. Passenger-capacity: ROAD MOTOR TRANSPORTATION ACT [CHAPTER 262] Route 1: As d^ned in the agreonent between the holder and Applications in Connexion with Road Service Permits the Harare Municipality, approved by the Minister in terms of section 18 of the Road Motor Transportation Act [Chapter 262]. IN terms of subsection (4) of section 7 of the Road Motor Transportation Act [Chapter 262], notice is hereby given that Route 2:' Throu^out Zimbabwe. the applications detailed in the Sdiedule, for ue issue or Route 3: Harare - Darwendale - Banket - Chinhoyi - Aladta amendment of road service permits, have been received for the Compoimd - Sheckleton Mine - lions Den. consideration of the Controller of Road Motor Transportation. Condition: Any person wishing to object to any such application must Route 2: lodge with the Controller of Road Motor Transportation, (a) For private hire and for advertised or organized P.O. Box 8332, Causeway— tours, provided no stage carriage service is operated (a) a notice, in writing, of his intention to object, so as along any route. to reach the Controller’s ofiSce not later than the 23rd (b) No private Hire or any advertised or organized tour July, 1993; shall be operated under authority of this permit, (b) his objection and the grounds therefor, on form RAl.T. during ^e times for which a scheduled stage carriage 24, together with two copies tiiereof, so as to tetaxHa. -

Bulawayo City Mpilo Central Hospital
Province District Name of Site Bulawayo Bulawayo City E. F. Watson Clinic Bulawayo Bulawayo City Mpilo Central Hospital Bulawayo Bulawayo City Nkulumane Clinic Bulawayo Bulawayo City United Bulawayo Hospital Manicaland Buhera Birchenough Bridge Hospital Manicaland Buhera Murambinda Mission Hospital Manicaland Chipinge Chipinge District Hospital Manicaland Makoni Rusape District Hospital Manicaland Mutare Mutare Provincial Hospital Manicaland Mutasa Bonda Mission Hospital Manicaland Mutasa Hauna District Hospital Harare Chitungwiza Chitungwiza Central Hospital Harare Chitungwiza CITIMED Clinic Masvingo Chiredzi Chikombedzi Mission Hospital Masvingo Chiredzi Chiredzi District Hospital Masvingo Chivi Chivi District Hospital Masvingo Gutu Chimombe Rural Hospital Masvingo Gutu Chinyika Rural Hospital Masvingo Gutu Chitando Rural Health Centre Masvingo Gutu Gutu Mission Hospital Masvingo Gutu Gutu Rural Hospital Masvingo Gutu Mukaro Mission Hospital Masvingo Masvingo Masvingo Provincial Hospital Masvingo Masvingo Morgenster Mission Hospital Masvingo Mwenezi Matibi Mission Hospital Masvingo Mwenezi Neshuro District Hospital Masvingo Zaka Musiso Mission Hospital Masvingo Zaka Ndanga District Hospital Matabeleland South Beitbridge Beitbridge District Hospital Matabeleland South Gwanda Gwanda Provincial Hospital Matabeleland South Insiza Filabusi District Hospital Matabeleland South Mangwe Plumtree District Hospital Matabeleland South Mangwe St Annes Mission Hospital (Brunapeg) Matabeleland South Matobo Maphisa District Hospital Matabeleland South Umzingwane Esigodini District Hospital Midlands Gokwe South Gokwe South District Hospital Midlands Gweru Gweru Provincial Hospital Midlands Kwekwe Kwekwe General Hospital Midlands Kwekwe Silobela District Hospital Midlands Mberengwa Mberengwa District Hospital . -

African Development Bank African Development Fund
AFRICAN DEVELOPMENT BANK AFRICAN DEVELOPMENT FUND Public Disclosure Authorized Disclosure Public BULAWAYO WATER AND SEWERAGE SERVICES IMPROVEMENT PROJECT COUNTRY: ZIMBABWE APPRAISAL REPORT Public Disclosure Authorized Disclosure Public OWAS DEPARTMENT November 2015 TABLE OF CONTENTS SUMMARY ................................................................................................................................................ iii RESULTS- BASED LOGICAL FRAMEWORK ................................................................................... iv I – STRATEGIC THRUST & RATIONALE .............................................................................................. 1 1.1 Project Linkages with Country Strategy and Objectives ............................................................ 1 1.2 Rationale for Bank’s Involvement .............................................................................................. 2 1.3 Donor Coordination .................................................................................................................... 3 II. PROJECT DESCRIPTION ...................................................................................................................... 4 2.1 Detailed Project Components ...................................................................................................... 4 2.2 Technical Solution Retained and Other Alternatives Explored .................................................. 5 2.3 Project Type ............................................................................................................................... -

Conference Paper Series
POLITICAL ECONOMY RESEARCH INSTITUTE University of Massachusetts Amherst Community Rights, Costs, and Benefits: The Question of Natural Resource Stewardship and Community Benefits in Zimbabwe’s CAMPFIRE Program James C. Murombedzi January 2003 CONFERENCE PAPER SERIES No. 16 Committees, Rights, Costs and Benefits: The Question of Natural Resource Stewardship and Community Benefits in Zimbabwe’s CAMPFIRE Program James C. Murombedzi The Ford Foundation Johannesburg, South Africa 1 In the CAMPFIRE formulation, the resource management problems obtaining in the communal areas of Zimbabwe are the result of the absence of both the institutional capacity as well as the incentives to manage the resources in question. The CAMPFIRE solution, therefore, was to introduce new systems of group ownership and territorial rights to natural resources to communities, and provide the appropriate institutions for legitimate resource management for the benefit of these communities (Martin 1986). The implementation of this solution was attained through the enactment of an amendment to the Parks and Wild Life Act of 1975, which enables the government to delegate appropriate authority over the wildlife to the ‘communal representatives’. The CAMPFIRE program in fact constitutes a transfer of the notion of ownership, successfully implemented with regard to individual landowners, to communal landowners (Farquharson 1993). This chapter tests the extent to which CAMPFIRE has in fact been able to devolve ownership over wildlife to communities in the communal areas, and thereby promoted stewardship of wildlife through the production of benefits for the participating communities. To achieve this, I will proceed by first evaluating the extent to which CAMPFIRE has succeeded in eliciting stewardship of the wildlife resource by participating communities through the devolution of clear and unambiguous rights to wildlife to these communities. -

PLAAS RR46 Smeadzim 1.Pdf
Chrispen Sukume, Blasio Mavedzenge, Felix Murimbarima and Ian Scoones Faculty of Economic and Management Sciences Research Report 46 Space, Markets and Employment in Agricultural Development: Zimbabwe Country Report Chrispen Sukume, Blasio Mavedzenge, Felix Murimbarima and Ian Scoones Published by the Institute for Poverty, Land and Agrarian Studies, Faculty of Economic and Management Sciences, University of the Western Cape, Private Bag X17, Bellville 7535, Cape Town, South Africa Tel: +27 21 959 3733 Fax: +27 21 959 3732 Email: [email protected] Institute for Poverty, Land and Agrarian Studies Research Report no. 46 June 2015 All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means without prior permission from the publisher or the authors. Copy Editor: Vaun Cornell Series Editor: Rebecca Pointer Photographs: Pamela Ngwenya Typeset in Frutiger Thanks to the UK’s Department for International Development (DfID) and the Economic and Social Research Council’s (ESRC) Growth Research Programme Contents List of tables ................................................................................................................ ii List of figures .............................................................................................................. iii Acronyms and abbreviations ...................................................................................... v 1 Introduction ........................................................................................................ -

Promotion of Climate-Resilient Lifestyles Among Rural Families in Gutu
Promotion of climate-resilient lifestyles among rural families in Gutu (Masvingo Province), Mutasa (Manicaland Province) and Shamva (Mashonaland Central Province) Districts | Zimbabwe Sahara and Sahel Observatory 26 November 2019 Promotion of climate-resilient lifestyles among rural families in Gutu Project/Programme title: (Masvingo Province), Mutasa (Manicaland Province) and Shamva (Mashonaland Central Province) Districts Country(ies): Zimbabwe National Designated Climate Change Management Department, Ministry of Authority(ies) (NDA): Environment, Water and Climate Development Aid from People to People in Zimbabwe (DAPP Executing Entities: Zimbabwe) Accredited Entity(ies) (AE): Sahara and Sahel Observatory Date of first submission/ 7/19/2019 V.1 version number: Date of current submission/ 11/26/2019 V.2 version number A. Project / Programme Information (max. 1 page) ☒ Project ☒ Public sector A.2. Public or A.1. Project or programme A.3 RFP Not applicable private sector ☐ Programme ☐ Private sector Mitigation: Reduced emissions from: ☐ Energy access and power generation: 0% ☐ Low emission transport: 0% ☐ Buildings, cities and industries and appliances: 0% A.4. Indicate the result ☒ Forestry and land use: 25% areas for the project/programme Adaptation: Increased resilience of: ☒ Most vulnerable people and communities: 25% ☒ Health and well-being, and food and water security: 25% ☐ Infrastructure and built environment: 0% ☒ Ecosystem and ecosystem services: 25% A.5.1. Estimated mitigation impact 399,223 tCO2eq (tCO2eq over project lifespan) A.5.2. Estimated adaptation impact 12,000 direct beneficiaries (number of direct beneficiaries) A.5. Impact potential A.5.3. Estimated adaptation impact 40,000 indirect beneficiaries (number of indirect beneficiaries) A.5.4. Estimated adaptation impact 0.28% of the country’s total population (% of total population) A.6. -

Crop Area, Condition and Stage
Foreword The Government of Zimbabwe has continued to exhibit its commitment for reducing food and nutrition insecurity in Zimbabwe. Evidence include the culmination of ZimASSET’s Food and Nutrition Security Cluster and the multi-sector Food and Nutrition Security Policy (FNSP). Recognising the vagaries of climate variabilities and the unforeseeable potential livelihood challenges, Government put in place structures whose mandates are, among other things to provide early warning information for early actioning. The Food and Nutrition Council, through the ZimVAC, is one of such structures which strives to fulfil the aspirations of the FNSP’s commitment number 6 of providing food and nutrition early warning information. In response to the advent of the El Nino phenomena which has resulted in the country experiencing long dry spells, the ZimVAC undertook a rapid assessment focussing on updating the ZimVAC May 2015 results. The lean season monitoring focused on the relevant food and nutrition security parameters. The process followed a 3 pronged approach which were, a review of existing food and nutrition secondary data, qualitative district Focus Group Discussions (FGDs) and for other variables a quantitative household survey which in most cases are representative at provincial and national level. This report provides a summation of the results for the 3 processes undertaken and focuses on the following thematic areas: the rainfall season quality, 2015/16 agricultural assistance, crop and livestock condition, food and livestock markets, gender based violence, household income sources and livelihoods strategies, domestic and production water situation, health and nutrition, food assistance and a review of the rural food security projections. -
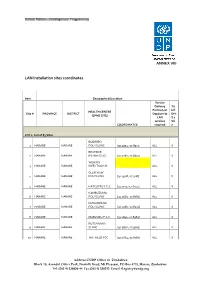
LAN Installation Sites Coordinates
ANNEX VIII LAN Installation sites coordinates Item Geographical/Location Service Delivery Tic Points (List k if HEALTH CENTRE Site # PROVINCE DISTRICT Dept/umits DHI (EPMS SITE) LAN S 2 services Sit COORDINATES required e LOT 1: List of 83 Sites BUDIRIRO 1 HARARE HARARE POLYCLINIC [30.9354,-17.8912] ALL X BEATRICE 2 HARARE HARARE RD.INFECTIO [31.0282,-17.8601] ALL X WILKINS 3 HARARE HARARE INFECTIOUS H ALL X GLEN VIEW 4 HARARE HARARE POLYCLINIC [30.9508,-17.908] ALL X 5 HARARE HARARE HATCLIFFE P.C.C. [31.1075,-17.6974] ALL X KAMBUZUMA 6 HARARE HARARE POLYCLINIC [30.9683,-17.8581] ALL X KUWADZANA 7 HARARE HARARE POLYCLINIC [30.9285,-17.8323] ALL X 8 HARARE HARARE MABVUKU P.C.C. [31.1841,-17.8389] ALL X RUTSANANA 9 HARARE HARARE CLINIC [30.9861,-17.9065] ALL X 10 HARARE HARARE HATFIELD PCC [31.0864,-17.8787] ALL X Address UNDP Office in Zimbabwe Block 10, Arundel Office Park, Norfolk Road, Mt Pleasant, PO Box 4775, Harare, Zimbabwe Tel: (263 4) 338836-44 Fax:(263 4) 338292 Email: [email protected] NEWLANDS 11 HARARE HARARE CLINIC ALL X SEKE SOUTH 12 HARARE CHITUNGWIZA CLINIC [31.0763,-18.0314] ALL X SEKE NORTH 13 HARARE CHITUNGWIZA CLINIC [31.0943,-18.0152] ALL X 14 HARARE CHITUNGWIZA ST.MARYS CLINIC [31.0427,-17.9947] ALL X 15 HARARE CHITUNGWIZA ZENGEZA CLINIC [31.0582,-18.0066] ALL X CHITUNGWIZA CENTRAL 16 HARARE CHITUNGWIZA HOSPITAL [31.0628,-18.0176] ALL X HARARE CENTRAL 17 HARARE HARARE HOSPITAL [31.0128,-17.8609] ALL X PARIRENYATWA CENTRAL 18 HARARE HARARE HOSPITAL [30.0433,-17.8122] ALL X MURAMBINDA [31.65555953980,- 19 MANICALAND -

THE HISTORY of the TONGA and FISHING COOPERATIVES in BINGA DISTRICT 1950S-2015
FACULTY OF ARTS DEPARTMENT OF HISTORY EMPOWERMENT OR CONTROL? : THE HISTORY OF THE TONGA AND FISHING COOPERATIVES IN BINGA DISTRICT 1950s-2015 BY HONOUR M.M. SINAMPANDE R131722P DISSERTATION SUBMITTED TO THE FACULTY OF ARTS IN PARTIAL FULLFILMENT OF THE REQUIREMENTS OF THE HONOURS DEGREE IN HISTORY AT MIDLANDS STATE UNIVERSITY. NOVEMBER 2016 ZVISHAVANE: ZIMBABWE SUPERVISOR DR. T.M. MASHINGAIDZE APPROVAL FORM The undersigned certify that they have supervised the student Honour M.M Sinampande (R131722P) dissertation entitled Empowerment or Control? : The history of the Tonga and fishing cooperatives in Binga District 1950-210 submitted in partial fulfillment of the requirements of the Bachelor of Arts in History Honours Degree offered by Midlands State University. Dr. T.M Mashingaidze ……………………… SUPERVISOR DATE …….……………………………………… …………………………….. CHAIRPERSON DATE ….………………………………………… …………………………….. EXTERNAL EXAMINER DATE DECLARATION I, Honour M.M Sinampande declare that, Empowerment or Control? : The history of the Tonga and fishing cooperatives in Binga District 1950s-2015 is my own work and it has never been submitted before any degree or examination in any other university. I declare that all sources which have been used have been acknowledged. I authorize the Midlands State University to lend this to other institution or individuals for purposes of academic research only. Honour M.M Sinampande …………………………………………… 2016 DEDICATION This work is dedicated to my father Mr. H.M Sinampande and my mother Ms. J. Muleya for their inspiration, love and financial support throughout my four year degree programme. ABSTRACT The history of the Tonga have it that, the introduction of the fishing villages initially and then later the cooperative system in Binga District from the 1950s-2015 saw the Zambezi Tonga lose their fishing rights.