Expert Reviewers for Orphanet in 2020 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Centronuclear Myopathies Under Attack: a Plethora of Therapeutic Targets Hichem Tasfaout, Belinda Cowling, Jocelyn Laporte
CORE Metadata, citation and similar papers at core.ac.uk Provided by Archive Ouverte en Sciences de l'Information et de la Communication Centronuclear myopathies under attack: A plethora of therapeutic targets Hichem Tasfaout, Belinda Cowling, Jocelyn Laporte To cite this version: Hichem Tasfaout, Belinda Cowling, Jocelyn Laporte. Centronuclear myopathies under attack: A plethora of therapeutic targets. Journal of Neuromuscular Diseases, IOS Press, 2018, 5, pp.387 - 406. 10.3233/JND-180309. hal-02438924 HAL Id: hal-02438924 https://hal.archives-ouvertes.fr/hal-02438924 Submitted on 14 Jan 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Journal of Neuromuscular Diseases 5 (2018) 387–406 387 DOI 10.3233/JND-180309 IOS Press Review Centronuclear myopathies under attack: A plethora of therapeutic targets Hichem Tasfaouta,b,c,d, Belinda S. Cowlinga,b,c,d,1 and Jocelyn Laportea,b,c,d,1,∗ aDepartment of Translational Medicine and Neurogenetics, Institut de G´en´etique et de Biologie Mol´eculaire et Cellulaire (IGBMC), Illkirch, France bInstitut National de la Sant´eetdelaRechercheM´edicale (INSERM), U1258, Illkirch, France cCentre National de la Recherche Scientifique (CNRS), UMR7104, Illkirch, France dUniversit´e de Strasbourg, Illkirch, France Abstract. -

Affected Female Carriers of MTM1 Mutations Display a Wide Spectrum
Acta Neuropathol DOI 10.1007/s00401-017-1748-0 ORIGINAL PAPER Afected female carriers of MTM1 mutations display a wide spectrum of clinical and pathological involvement: delineating diagnostic clues Valérie Biancalana1,2,3,4,5 · Sophie Scheidecker1 · Marguerite Miguet1 · Annie Laquerrière6 · Norma B. Romero7,8 · Tanya Stojkovic8 · Osorio Abath Neto9 · Sandra Mercier10,11,12 · Nicol Voermans13 · Laura Tanner14 · Curtis Rogers15 · Elisabeth Ollagnon‑Roman16 · Helen Roper17 · Célia Boutte18 · Shay Ben‑Shachar19 · Xavière Lornage2,3,4,5 · Nasim Vasli2,3,4,5 · Elise Schaefer20 · Pascal Laforet21 · Jean Pouget22 · Alexandre Moerman23 · Laurent Pasquier24 · Pascale Marcorelle25,26 · Armelle Magot12 · Benno Küsters27 · Nathalie Streichenberger28 · Christine Tranchant29 · Nicolas Dondaine1 · Raphael Schneider2,3,4,5,30 · Claire Gasnier1 · Nadège Calmels1 · Valérie Kremer31 · Karine Nguyen32 · Julie Perrier12 · Erik Jan Kamsteeg33 · Pierre Carlier34 · Robert‑Yves Carlier35 · Julie Thompson30 · Anne Boland36 · Jean‑François Deleuze36 · Michel Fardeau7,8 · Edmar Zanoteli9 · Bruno Eymard21 · Jocelyn Laporte2,3,4,5 Received: 9 May 2017 / Revised: 24 June 2017 / Accepted: 2 July 2017 © Springer-Verlag GmbH Germany 2017 Abstract X-linked myotubular myopathy (XLMTM), a females and to delineate diagnostic clues, we character- severe congenital myopathy, is caused by mutations in the ized 17 new unrelated afected females and performed a MTM1 gene located on the X chromosome. A majority of detailed comparison with previously reported cases at the afected males die in the early postnatal period, whereas clinical, muscle imaging, histological, ultrastructural and female carriers are believed to be usually asymptomatic. molecular levels. Taken together, the analysis of this large Nevertheless, several afected females have been reported. cohort of 43 cases highlights a wide spectrum of clini- To assess the phenotypic and pathological spectra of carrier cal severity ranging from severe neonatal and generalized weakness, similar to XLMTM male, to milder adult forms. -

Unilateral Proximal Focal Femoral Deficiency, Fibular Aplasia, Tibial
The Egyptian Journal of Medical Human Genetics (2014) 15, 299–303 Ain Shams University The Egyptian Journal of Medical Human Genetics www.ejmhg.eg.net www.sciencedirect.com CASE REPORT Unilateral proximal focal femoral deficiency, fibular aplasia, tibial campomelia and oligosyndactyly in an Egyptian child – Probable FFU syndrome Rabah M. Shawky a,*, Heba Salah Abd Elkhalek a, Shaimaa Gad a, Shaimaa Abdelsattar Mohammad b a Pediatric Department, Genetics Unit, Ain Shams University, Egypt b Radio Diagnosis Department, Ain Shams University, Egypt Received 2 March 2014; accepted 18 March 2014 Available online 30 April 2014 KEYWORDS Abstract We report a fifteen month old Egyptian male child, the third in order of birth of healthy Short femur; non consanguineous parents, who has normal mentality, normal upper limbs and left lower limb. Limb anomaly; The right lower limb has short femur, and tibia with anterior bowing, and an overlying skin dimple. FFU syndrome; The right foot has also oligosyndactyly (three toes), and the foot is in vulgus position. There is lim- Proximal focal femoral ited abduction at the hip joint, full flexion and extension at the knee, limited dorsiflexion and plan- deficiency; tar flexion at the ankle joint. The X-ray of the lower limb and pelvis shows proximal focal femoral Fibular aplasia; deficiency, absent right fibula with shortening of the right tibia and anterior bowing of its distal Tibial campomelia; third. The acetabulum is shallow. He has a family history of congenital cyanotic heart disease. Oligosyndactyly Our patient represents most probably the first case of femur fibula ulna syndrome (FFU) in Egypt with unilateral right leg affection. -
Multiple Hereditary Exostoses
Multiple Hereditary Exostoses Dror Paley MD, FRCSC Medical Director, Paley Orthopedic and spine Institute, St. Mary’s Medical Center, West palm Beach, FL David Feldman, MD Director, Spinal deformity center, Paley Orthopedic and spine Institute, St. Mary’s Medical Center, West palm Beach, FL Multiple hereditary exostoses (MHE), also known as multiple osteochondromas (MO), is an autosomal dominant skeletal disorder. Approximately 10–20% of individuals are a result of a spontaneous mutation while the rest are familial. The prevalence of MHE/MO is 1/50 000. There are two known genes found to cause MHE/MO, EXT1 located on chromosome 8q23-q24 and EXT2 located on chromosome 11p11-p12. In 10–15% of the patients, no mutation can be located by current methods of genetic testing.1–7 These mutations are scattered across both genes. EXT1/EXT2 is essential for the biosynthesis of heparan sulfate (HS). HS production in patients’ cells is reduced by 50% or more.8–19 MHE/MO is associated with characteristic progressive skeletal deformities of the extremities and shortening of one or both the sides, leading to limb length discrepancy (LLD) and short stature.20–28 Two bone segments, such as the lower leg or forearm, are at greater risk of problems due to either osteochondromas (OCs) from one or both bones impinging on or deforming the other bone or a primary issue of altered growth causing one bone to grow at a faster or slower rate. OCs can also affect joint motion due to impingement of an OC with the opposite side of the joint or subluxation/dislocation related to deformity, impingement, and incongruity.20,24,26,29,30 OCs can also cause nerve or vessel entrapment and/or compression, including the spinal cord and nerve roots. -

Psykisk Utviklingshemming Og Forsinket Utvikling
Psykisk utviklingshemming og forsinket utvikling Genpanel, versjon v03 Tabellen er sortert på gennavn (HGNC gensymbol) Navn på gen er iht. HGNC >x10 Andel av genet som har blitt lest med tilfredstillende kvalitet flere enn 10 ganger under sekvensering x10 er forventet dekning; faktisk dekning vil variere. Gen Gen (HGNC Transkript >10x Fenotype (symbol) ID) AAAS 13666 NM_015665.5 100% Achalasia-addisonianism-alacrimia syndrome OMIM AARS 20 NM_001605.2 100% Charcot-Marie-Tooth disease, axonal, type 2N OMIM Epileptic encephalopathy, early infantile, 29 OMIM AASS 17366 NM_005763.3 100% Hyperlysinemia OMIM Saccharopinuria OMIM ABCB11 42 NM_003742.2 100% Cholestasis, benign recurrent intrahepatic, 2 OMIM Cholestasis, progressive familial intrahepatic 2 OMIM ABCB7 48 NM_004299.5 100% Anemia, sideroblastic, with ataxia OMIM ABCC6 57 NM_001171.5 93% Arterial calcification, generalized, of infancy, 2 OMIM Pseudoxanthoma elasticum OMIM Pseudoxanthoma elasticum, forme fruste OMIM ABCC9 60 NM_005691.3 100% Hypertrichotic osteochondrodysplasia OMIM ABCD1 61 NM_000033.3 77% Adrenoleukodystrophy OMIM Adrenomyeloneuropathy, adult OMIM ABCD4 68 NM_005050.3 100% Methylmalonic aciduria and homocystinuria, cblJ type OMIM ABHD5 21396 NM_016006.4 100% Chanarin-Dorfman syndrome OMIM ACAD9 21497 NM_014049.4 99% Mitochondrial complex I deficiency due to ACAD9 deficiency OMIM ACADM 89 NM_000016.5 100% Acyl-CoA dehydrogenase, medium chain, deficiency of OMIM ACADS 90 NM_000017.3 100% Acyl-CoA dehydrogenase, short-chain, deficiency of OMIM ACADVL 92 NM_000018.3 100% VLCAD -

(12) Patent Application Publication (10) Pub. No.: US 2016/0281166 A1 BHATTACHARJEE Et Al
US 20160281 166A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2016/0281166 A1 BHATTACHARJEE et al. (43) Pub. Date: Sep. 29, 2016 (54) METHODS AND SYSTEMIS FOR SCREENING Publication Classification DISEASES IN SUBJECTS (51) Int. Cl. (71) Applicant: PARABASE GENOMICS, INC., CI2O I/68 (2006.01) Boston, MA (US) C40B 30/02 (2006.01) (72) Inventors: Arindam BHATTACHARJEE, G06F 9/22 (2006.01) Andover, MA (US); Tanya (52) U.S. Cl. SOKOLSKY, Cambridge, MA (US); CPC ............. CI2O 1/6883 (2013.01); G06F 19/22 Edwin NAYLOR, Mt. Pleasant, SC (2013.01); C40B 30/02 (2013.01); C12O (US); Richard B. PARAD, Newton, 2600/156 (2013.01); C12O 2600/158 MA (US); Evan MAUCELI, (2013.01) Roslindale, MA (US) (21) Appl. No.: 15/078,579 (57) ABSTRACT (22) Filed: Mar. 23, 2016 Related U.S. Application Data The present disclosure provides systems, devices, and meth (60) Provisional application No. 62/136,836, filed on Mar. ods for a fast-turnaround, minimally invasive, and/or cost 23, 2015, provisional application No. 62/137,745, effective assay for Screening diseases, such as genetic dis filed on Mar. 24, 2015. orders and/or pathogens, in Subjects. Patent Application Publication Sep. 29, 2016 Sheet 1 of 23 US 2016/0281166 A1 SSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSSS S{}}\\93? sau36 Patent Application Publication Sep. 29, 2016 Sheet 2 of 23 US 2016/0281166 A1 &**** ? ???zzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzzz??º & %&&zzzzzzzzzzzzzzzzzzzzzzz &Sssssssssssssssssssssssssssssssssssssssssssssssssssssssss & s s sS ------------------------------ Patent Application Publication Sep. 29, 2016 Sheet 3 of 23 US 2016/0281166 A1 23 25 20 FG, 2. Patent Application Publication Sep. 29, 2016 Sheet 4 of 23 US 2016/0281166 A1 : S Patent Application Publication Sep. -

Management of Fibular Hemimelia (Congenital Absence of Fibula) Using Ilizarov Method in Sulaimani
European Scientific Journal October 2015 edition vol.11, No.30 ISSN: 1857 – 7881 (Print) e - ISSN 1857- 7431 MANAGEMENT OF FIBULAR HEMIMELIA (CONGENITAL ABSENCE OF FIBULA) USING ILIZAROV METHOD IN SULAIMANI Ass. Prof. Dr. Omer Ali Rafiq Barawi, Ass. Lecturer Zmnako J. Amen School of Medicine, University of Sulaimani, Kurdistan Region, Iraq Abstract Background: Fibular hemimelia is the most common congenital deficiency of long bones. Therefore, it is characterized by a wide spectrum of manifestations ranging from mild limb length inequality to sever shortening with foot and ankle deformities and associated anomalies. Objectives: To evaluate the results of ankle and foot reconstruction and limb length equalization in patients with Fibular Hemimelia. Patients and Methods: A prospective study was carried out on 40 limbs in 32 patients with fibular hemimelia during the periods of March 2010 to January 2014. Male to female ratio was 24:8. Their age ranged at an average between 2-16 years (9 years). The reconstruction of ankle and foot was done. Also, the equalization of the limb was done also using Ilizarov frame. Results: The result of this study was assessed using the Association for the Study of Applications of Methods of Ilizarov (ASAMI) scoring system. Therefore, the final results were: Failure rate with 2 limbs 5%, Poor with 2 limbs 5%, Fair with 2 limbs 5%, Good with 8 limbs 20%, and Excellent with 26 limbs 65%. Conclusion: In conclusion, the Ilizarov method is an attractive alternative method used for the management of selected fibular hemimelic patients having three or more toes who are refusing amputation. -

A CLINICAL STUDY of 25 CASES of CONGENITAL KEY WORDS: Ectromelia, Hemimelia, Dysmelia, Axial, Inter- LIMB DEFICIENCIES Calary
PARIPEX - INDIAN JOURNAL OF RESEARCH Volume-7 | Issue-1 | January-2018 | PRINT ISSN No 2250-1991 ORIGINAL RESEARCH PAPER Medical Science A CLINICAL STUDY OF 25 CASES OF CONGENITAL KEY WORDS: Ectromelia, Hemimelia, Dysmelia, Axial, Inter- LIMB DEFICIENCIES calary M.B.B.S., D.N.B (PMR), M.N.A.M.S Medical officer, D.P.M.R., K.G Medical Dr Abhiman Singh University Lucknow (UP) An Investigation of 25 patients from congenital limb deficient patients who went to D. P. M. R. , K.G Medical University Lucknow starting with 2010 with 2017. This study represents the congenital limb deficient insufficient number of the India. Commonest deficiencies were Adactylia Also mid Ectromelia (below knee/ below elbow deficiency).Below knee might have been basic in male same time The following elbow for female Youngsters. No conclusive reason for the deformity might be isolated, however, A large number guardians accepted that possible exposure to the eclipse throughout pregnancy might have been those reason for ABSTRACT those deficiency. INTRODUCTION Previous Treatment Only 15 patients had taken some D. P. M. R., K.G Medical University Lucknow (UP) may be a greatest treatment, 5 underwent some surgical treatment and only 4 Also its identity or sort of Rehabilitation Centre in India. Thusly the patients used prosthesis. This indicates the ignorance or lack of limb deficient children attending this department can easily be facilities to deal with the limb deficient children. accepted as a representative sample of the total congenital limb deficiency population in the India. DEFICIENCIES The deficiencies are classified into three categories:- MATERIAL AND METHODS This study incorporates 25 patients congenital limb deficiency for 1) Axial Dysmelia where medial or lateral portion is missing lack who originated for medicine at D. -

Myopathies Infosheet
The University of Chicago Genetic Services Laboratories 5841 S. Maryland Ave., Rm. G701, MC 0077, Chicago, Illinois 60637 Toll Free: (888) UC GENES (888) 824 3637 Local: (773) 834 0555 FAX: (773) 702 9130 [email protected] dnatesting.uchicago.edu CLIA #: 14D0917593 CAP #: 18827-49 Gene tic Testing for Congenital Myopathies/Muscular Dystrophies Congenital Myopathies Congenital myopathies are typically characterized by the presence of specific structural and histochemical features on muscle biopsy and clinical presentation can include congenital hypotonia, muscle weakness, delayed motor milestones, feeding difficulties, and facial muscle involvement (1). Serum creatine kinase may be normal or elevated. Heterogeneity in presenting symptoms can occur even amongst affected members of the same family. Congenital myopathies can be divided into three main clinicopathological defined categories: nemaline myopathy, core myopathy and centronuclear myopathy (2). Nemaline Myopathy Nemaline Myopathy is characterized by weakness, hypotonia and depressed or absent deep tendon reflexes. Weakness is typically proximal, diffuse or selective, with or without facial weakness and the diagnostic hallmark is the presence of distinct rod-like inclusions in the sarcoplasm of skeletal muscle fibers (3). Core Myopathy Core Myopathy is characterized by areas lacking histochemical oxidative and glycolytic enzymatic activity on histopathological exam (2). Symptoms include proximal muscle weakness with onset either congenitally or in early childhood. Bulbar and facial weakness may also be present. Patients with core myopathy are typically subclassified as either having central core disease or multiminicore disease. Centronuclear Myopathy Centronuclear Myopathy (CNM) is a rare muscle disease associated with non-progressive or slowly progressive muscle weakness that can develop from infancy to adulthood (4, 5). -
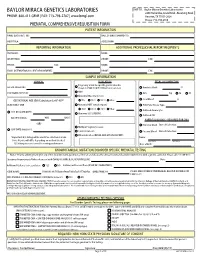
Prenatal Testing Requisition Form
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 PRENATAL COMPREHENSIVE REQUISITION FORM PATIENT INFORMATION NAME (LAST,FIRST, MI): DATE OF BIRTH (MM/DD/YY): HOSPITAL#: ACCESSION#: REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: SAMPLE INFORMATION CLINICAL INDICATION FETAL SPECIMEN TYPE Pregnancy at risk for specific genetic disorder DATE OF COLLECTION: (Complete FAMILIAL MUTATION information below) Amniotic Fluid: cc AMA PERFORMING PHYSICIAN: CVS: mg TA TC Abnormal Maternal Screen: Fetal Blood: cc GESTATIONAL AGE (GA) Calculation for AF-AFP* NTD TRI 21 TRI 18 Other: SELECT ONLY ONE: Abnormal NIPT (attach report): POC/Fetal Tissue, Type: TRI 21 TRI 13 TRI 18 Other: Cultured Amniocytes U/S DATE (MM/DD/YY): Abnormal U/S (SPECIFY): Cultured CVS GA ON U/S DATE: WKS DAYS PARENTAL BLOODS - REQUIRED FOR CMA -OR- Maternal Blood Date of Collection: Multiple Pregnancy Losses LMP DATE (MM/DD/YY): Parental Concern Paternal Blood Date of Collection: Other Indication (DETAIL AND ATTACH REPORT): *Important: U/S dating will be used if no selection is made. Name: Note: Results will differ depending on method checked. Last Name First Name U/S dating increases overall screening performance. Date of Birth: KNOWN FAMILIAL MUTATION/DISORDER SPECIFIC PRENATAL TESTING Notice: Prior to ordering testing for any of the disorders listed, you must call the lab and discuss the clinical history and sample requirements with a genetic counselor. -

Fibular Hemimelia Shawn C
Parent/Patient Education Series: Fibular Hemimelia Shawn C. Standard, M.D. What Is fIbuLar hemImeLIa? Fibular hemimelia falls under the category of congenital limb deficiency. This means that a growth abnormality occurred during the development of the lower limb bud at six to eight weeks after conception. Although most of the limb abnormalities are concentrated in the lower leg and foot, the entire lower extremity is affected by this condition. The most inclusive medical term for this condition is post-axial hypoplasia of the lower limb. This means that one side of the limb bud (post-axial side – small toe side) was altered resulting in an abnormal growth pattern. hoW Common Is fIbuLar hemImeLIa? The incidence of fibular hemimelia is 1 in 40,000 live births. To put this into perspective, the United States of America usually averages about 4,000,000 live births per year. This results in 100 live births with fibular hemimelia per year in the United States. What are the ChanCes that a seCond ChILd In the same famILy WILL have thIs CondItIon? The chances of a second child having fibular hemimelia are the same as the first, 1 in 40,000. Since this genetic mutation is spontaneous, there is no increased risk of having a second child with fibular hemimelia. What are the ChanCes that a person WIth fIbuLar hemImeLIa WILL have a ChILd WIth thIs CondItIon? A person with fibular hemimelia has a 1 in 40,000 chance of having a child with fibular hemimelia. Since this genetic mutation is spontaneous, there is no increased risk of fibular hemimelia being passed down to the next generation. -

Recurrent Pregnancy Loss Precision Panel Overview Indications Clinical
Recurrent Pregnancy Loss Precision Panel Overview Recurrent Pregnancy Loss (RPL) is one of the most common obstetric complications, affecting more than 30% of conceptions. These can occur during preimplantation, pre-embryonic, embryonic, early fetal, late fetal and stillbirth. An important number of losses are due to genetic abnormalities, nonetheless 50% of early pregnancy losses have been associated with chromosomal abnormalities. The majority are due to de novo non-disjunctional events during meiosis and balanced paternal translocations. Traditionally, the assessment of recurrent pregnancy loss was based on karyotyping techniques. However, advances in molecular genetic technology have provided an array of information regarding genetic causes and risk factors for pregnancy loss. One of the most innovative techniques with a significant role in RPL is preimplantation genetic testing in in vitro fertilization cycles. The Igenomix Recurrent Pregnancy Loss Precision Panel can be used to make a directed and accurate differential diagnosis of inability to carry out a full pregnancy ultimately leading to a better management and achieve a healthy baby at home. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Recurrent Pregnancy Loss Precision Panel is indicated for those patients the following manifestations: - Inability to conceive after 1 year of unprotected intercourse - Family history of infertility - Personal history of recurrent miscarriages - Family history of recurrent miscarriages - Previous failed IVF cycles - Other failed assisted reproductive technology (ART) treatments Clinical Utility The clinical utility of this panel is: - The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient.