Phs 403 Accident and Emergency
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Choking Game” Awareness and Participation Among 8Th Graders — Oregon, 2008
Morbidity and Mortality Weekly Report Weekly / Vol. 59 / No. 1 January 15, 2010 “Choking Game” Awareness and Participation Among 8th Graders — Oregon, 2008 The “choking game” is an activity in which persons strangu- based on the CDC’s Youth Risk Behavior Survey (YRBS) and late themselves to achieve euphoria through brief hypoxia (1). It includes questions on physical and mental health, sexual activ- is differentiated from autoerotic asphyxiation 2,3( ). The activity ity, substance use, physical activity/nutrition, and community can cause long-term disability and death among youths (4). In characteristics. In 2008, all 647 Oregon public middle and high 2008, CDC reported 82 deaths attributed to the choking game schools were part of the sampling frame, which was stratified and other strangulation activities during the period 1995–2007; into eight regions. Schools were sampled randomly from within most victims were adolescent males aged 11–16 years (4). To each region, with a total of 114 schools being sampled. The data assess the awareness and prevalence of this behavior among were weighted to achieve a statewide representative sample. 8th graders in Oregon, the Oregon Public Health Division Weighting was based on the probability of school and student added a question to the 2008 Oregon Healthy Teens survey selection, and a post-stratification adjustment for county par- concerning familiarity with and participation in this activity. ticipation. Schools use an active notification/passive consent This report describes the results of that survey, which indicated model with parents, who may decline their child’s participation. that 36.2% of 8th-grade respondents had heard of the choking In 2008, the survey contained a total of 188 questions, which game, 30.4% had heard of someone participating, and 5.7% had were designed to be completed in the course of a class period. -

The Civilian Impact of Drone Strikes
THE CIVILIAN IMPACT OF DRONES: UNEXAMINED COSTS, UNANSWERED QUESTIONS Acknowledgements This report is the product of a collaboration between the Human Rights Clinic at Columbia Law School and the Center for Civilians in Conflict. At the Columbia Human Rights Clinic, research and authorship includes: Naureen Shah, Acting Director of the Human Rights Clinic and Associate Director of the Counterterrorism and Human Rights Project, Human Rights Institute at Columbia Law School, Rashmi Chopra, J.D. ‘13, Janine Morna, J.D. ‘12, Chantal Grut, L.L.M. ‘12, Emily Howie, L.L.M. ‘12, Daniel Mule, J.D. ‘13, Zoe Hutchinson, L.L.M. ‘12, Max Abbott, J.D. ‘12. Sarah Holewinski, Executive Director of Center for Civilians in Conflict, led staff from the Center in conceptualization of the report, and additional research and writing, including with Golzar Kheiltash, Erin Osterhaus and Lara Berlin. The report was designed by Marla Keenan of Center for Civilians in Conflict. Liz Lucas of Center for Civilians in Conflict led media outreach with Greta Moseson, pro- gram coordinator at the Human Rights Institute at Columbia Law School. The Columbia Human Rights Clinic and the Columbia Human Rights Institute are grateful to the Open Society Foundations and Bullitt Foundation for their financial support of the Institute’s Counterterrorism and Human Rights Project, and to Columbia Law School for its ongoing support. Copyright © 2012 Center for Civilians in Conflict (formerly CIVIC) and Human Rights Clinic at Columbia Law School All rights reserved Printed in the United States of America. Copies of this report are available for download at: www.civiliansinconflict.org Cover: Shakeel Khan lost his home and members of his family to a drone missile in 2010. -

The Twenty Greatest Music Concerts I've Ever Seen
THE TWENTY GREATEST MUSIC CONCERTS I'VE EVER SEEN Whew, I'm done. Let me remind everyone how this worked. I would go through my Ipod in that weird Ipod alphabetical order and when I would come upon an artist that I have seen live, I would replay that concert in my head. (BTW, since this segment started I no longer even have an ipod. All my music is on my laptop and phone now.) The number you see at the end of the concert description is the number of times I have seen that artist live. If it was multiple times, I would do my best to describe the one concert that I considered to be their best. If no number appears, it means I only saw that artist once. Mind you, I have seen many artists live that I do not have a song by on my Ipod. That artist is not represented here. So although the final number of concerts I have seen came to 828 concerts (wow, 828!), the number is actually higher. And there are "bar" bands and artists (like LeCompt and Sam Butera, for example) where I have seen them perform hundreds of sets, but I counted those as "one," although I have seen Lecompt in "concert" also. Any show you see with the four stars (****) means they came damn close to being one of the Top Twenty, but they fell just short. So here's the Twenty. Enjoy and thanks so much for all of your input. And don't sue me if I have a date wrong here and there. -

Programme & Abstracts
The 57th Annual Meeting of the International Association of Forensic Toxicologists. 2nd - 6th September 2019 BIRMINGHAM, UK The ICC Birmingham Broad Street, Birmingham B1 2EA Programme & Abstracts 1 Thank You to our Sponsors PlatinUm Gold Silver Bronze 2 3 Contents Welcome message 5 Committees 6 General information 7 iCC maps 8 exhibitors list 10 Exhibition Hall 11 Social Programme 14 opening Ceremony 15 Schedule 16 Oral Programme MONDAY 2 September 19 TUESDAY 3 September 21 THURSDAY 5 September 28 FRIDAY 6 September 35 vendor Seminars 42 Posters 46 oral abstracts 82 Poster abstracts 178 4 Welcome Message It is our great pleasure to welcome you to TIAFT Gala Dinner at the ICC on Friday evening. On the accompanying pages you will see a strong the UK for the 57th Annual Meeting of scientific agenda relevant to modern toxicology and we The International Association of Forensic thank all those who submitted an abstract and the Toxicologists Scientific Committees for making the scientific programme (TIAFT) between 2nd and 6th a success. Starting with a large Young Scientists September 2019. Symposium and Dr Yoo Memorial plenary lecture by Prof Tony Moffat on Monday, there are oral session topics in It has been decades since the Annual Meeting has taken Clinical & Post-Mortem Toxicology on Tuesday, place in the country where TIAFT was founded over 50 years Human Behaviour Toxicology & Drug-Facilitated Crime on ago. The meeting is supported by LTG (London Toxicology Thursday and Toxicology in Sport, New Innovations and Group) and the UKIAFT (UK & Ireland Association of Novel Research & Employment/Occupational Toxicology Forensic Toxicologists) and we thank all our exhibitors and on Friday. -
![Arxiv:1503.00071V1 [Cs.MA] 28 Feb 2015 Is Why Police Officers in Large Numbers Are Assigned at These Places to Ensure Safe Management of Crowd](https://docslib.b-cdn.net/cover/5433/arxiv-1503-00071v1-cs-ma-28-feb-2015-is-why-police-o-cers-in-large-numbers-are-assigned-at-these-places-to-ensure-safe-management-of-crowd-405433.webp)
Arxiv:1503.00071V1 [Cs.MA] 28 Feb 2015 Is Why Police Officers in Large Numbers Are Assigned at These Places to Ensure Safe Management of Crowd
Crowd Congestion and Stampede Management through Multi Robotic Agents Garima Ahuja and Kamalakar Karlapalem Center for Data Engineering, International Institute of Information Technology Hyderabad, India {[email protected],[email protected]} Abstract. Crowd management is a complex, challenging and crucial task. Lack of appropriate management of crowd has, in past, led to many unfortunate stampedes with significant loss of life. To increase the crowd management efficiency, we deploy automated real time detection of stampede prone areas. Then, we use robotic agents to aid the crowd management police in controlling the crowd in these stampede prone ar- eas. While doing so, we aim for minimum interference by robotic agents in our environment. Thereby not disturbing the ambience and aesthetics of the place. We evaluate the effectiveness of our model in dealing with difficult scenarios like emergency evacuation and presence of localized congestion. Lastly, we simulate a multi agent system based on our model and use it to illustrate the utility of robotic agents for detecting and reducing congestion. Keywords: Crowd Management, Stampede, Congestion, Localized Con- gestion, Emergency Evacuation 1 Introduction Managing large crowds is a difficult task. Ineffective execution of this task can potentially lead to stampedes. History suggests that crowd management police appointed to prevent such incidents have not been very successful. During a coro- nation festival in Russia, a police force of 1,800 men failed to control the crowd, leading to loss of 1,389 lives by trampling [4]. Crowd management is a team task, it requires strategic communication to figure out where to lead the crowd. -

M E M O R a N D U M
M E M O R A N D U M TO: Technical Committee on Gaseous Fire Extinguishing Systems FROM: Barry Chase, Staff Liaison DATE: March 20, 2019 SUBJECT: NFPA 12/12A/2001 First Draft Meeting Agenda (F2020) April 24-26, 2019, Memphis, TN 1. Call to Order – April 24, 2019, 8:00am ET 2. Chair’s comments 3. Previous minutes [April 25, 2017, Linthicum Heights, MD] 4. NFPA Staff Liaison Presentation a. NFPA Standards Development Process b. NFPA Resources 5. NFPA 2001 First Draft a. Public input [see attached] b. Report of the Task Group on Total Flooding Design Concentration Requirements (5.4.2) [P. Rivers] c. Presentation on Halocarbon Blend 55 (related to PI 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 58, 60) [Robert Richard – Honeywell] d. April 25, 8:00AM - Presentation on Toxicity of Halocarbon Impurities (related to PI 74) [Kurt Werner, Government and Regulatory Affairs Manager, 3M Electronics Materials Solutions Division] e. April 25, 9:00AM - Presentation on Toxicity of Halocarbon Impurities [Steve Hodges, Alion Science and Technology] f. Committee revisions g. Staff notes and editorial issues 6. NFPA 12 First Draft a. Public input [see attached] b. Report of the Task Group on Low Pressure Containers (4.6.6.1.1) [K. Adrian] c. Committee revisions d. Staff notes and editorial issues 7. NFPA 12A First Draft a. Public input [see attached] b. Committee revisions c. Staff notes and editorial issues 8. Other business 9. Next meeting location and dates 1 of 371 All NFPA Technical Committee meetings are open to the public. -

“Quiet Please, It's a Bloody Opera”!
UNIVERSITETET I OSLO “Quiet Please, it’s a bloody opera”! How is Tommy a part of the Opera History? Martin Nordahl Andersen [27.10.11] A theatre/performance/popular musicology master thesis on the rock opera Tommy by The Who ”Quiet please, it’s a bloody opera!” Martin Nordahl Andersen 2011 “Quiet please, it’s a bloody opera!” How is Tommy part of the Opera History? Print: Reprosentralen, University of Oslo All photos by Ross Halfin © All photos used with written permission. 1 ”Quiet please, it’s a bloody opera!” Aknowledgements I would like to thank my supervisors Ståle Wikshåland and Stan Hawkins for superb support and patience during the three years it took me to get my head around to finally finish this thesis. Thank you both for not giving up on me even when things were moving very slow. I am especially thankful for your support in my work in the combination of popular music/performance studies. A big thank you goes to Siren Leirvåg for guidance in the literature of theatre studies. Everybody at the Institute of Music at UiO for helping me when I came back after my student hiatus in 2007. I cannot over-exaggerate my gratitude towards Rob Lee, webmaster at www.thewho.com for helping me with finding important information on that site and his attempts at getting me an interview with one of the boys. The work being done on that site is fantastic. Also, a big thank you to my fellow Who fans. Discussing Who with you makes liking the band more fun. -

Critical Corpse Studies: Engaging with Corporeality and Mortality in Curriculum
Taboo: The Journal of Culture and Education Volume 19 Issue 3 The Affect of Waste and the Project of Article 10 Value: April 2020 Critical Corpse Studies: Engaging with Corporeality and Mortality in Curriculum Mark Helmsing George Mason University, [email protected] Cathryn van Kessel University of Alberta, [email protected] Follow this and additional works at: https://digitalscholarship.unlv.edu/taboo Recommended Citation Helmsing, M., & van Kessel, C. (2020). Critical Corpse Studies: Engaging with Corporeality and Mortality in Curriculum. Taboo: The Journal of Culture and Education, 19 (3). Retrieved from https://digitalscholarship.unlv.edu/taboo/vol19/iss3/10 This Article is protected by copyright and/or related rights. It has been brought to you by Digital Scholarship@UNLV with permission from the rights-holder(s). You are free to use this Article in any way that is permitted by the copyright and related rights legislation that applies to your use. For other uses you need to obtain permission from the rights-holder(s) directly, unless additional rights are indicated by a Creative Commons license in the record and/ or on the work itself. This Article has been accepted for inclusion in Taboo: The Journal of Culture and Education by an authorized administrator of Digital Scholarship@UNLV. For more information, please contact [email protected]. 140 CriticalTaboo, Late Corpse Spring Studies 2020 Critical Corpse Studies Engaging with Corporeality and Mortality in Curriculum Mark Helmsing & Cathryn van Kessel Abstract This article focuses on the pedagogical questions we might consider when teaching with and about corpses. Whereas much recent posthumanist writing in educational research takes up the Deleuzian question “what can a body do?,” this article investigates what a dead body can do for students’ encounters with life and death across the curriculum. -

Hijikata Tatsumi's Sabotage of Movement and the Desire to Kill The
Death and Desire in Contemporary Japan Representing, Practicing, Performing edited by Andrea De Antoni and Massimo Raveri Hijikata Tatsumi’s Sabotage of Movement and the Desire to Kill the Ideology of Death Katja Centonze (Universität Trier, Deutschland; Waseda University, Japan) Abstract Death and desire appear as essential characteristics in Hijikata Tatsumi’s butō, which brings the paradox of life and death, of stillness and movement into play. Hijikata places these con- tradictions at the roots of dance itself. This analysis points out several aspects displayed in butō’s death aesthetics and performing processes, which catch the tension between being dead and/or alive, between presence and absence. It is shown how the physical states of biological death are enacted, and demonstrated that in Hijikata’s nonhuman theatre of eroticism death stands out as an object aligned with the other objects on stage including the performer’s carnal body (nikutai). The discussion focuses on Hijikata’s radical investigation of corporeality, which puts under critique not only the nikutai, but even the corpse (shitai), revealing the cultural narratives they are subjected to. Summary 1 Deadly Erotic Labyrinth. – 2 Death Aesthetics for a Criminal and Erotic Dance. – 3 Rigor Mortis and Immobility. – 4 Shibusawa Tatsuhiko. Performance as Sacrifice and Experience. – 5 Pallor Mortis and shironuri. – 6 Shitai and suijakutai. The Dead are Dancing. – 7 The Reiteration of Death and the miira. – 8 The shitai under Critique. Death and the nikutai as Object. – 9 Against the Ideology of Death. Keywords Hijikata Tatsumi. Butō. Death. Eroticism. Corporeality. Acéphale. Anti-Dance. Body and Object. Corpse. Shibusawa Tatsuhiko. -

Autoerotic Asphyxiation: Secret Pleasure—Lethal Outcome?
Autoerotic Asphyxiation: Secret Pleasure—Lethal Outcome? WHAT’S KNOWN ON THIS SUBJECT: Centuries old, AEA first AUTHOR: Daniel D. Cowell, MD, MLS, CPHQ appeared in medical literature in 1856. Etiology is speculative, Departments of Psychiatry and Behavioral Medicine and and the majority of reports deal with fatal cases. Distortions of Graduate Medical Education, Marshall University, Joan C. normal development on the basis of psychoanalytic theories are the Edwards School of Medicine, Huntington, West Virginia most prevalent understanding of the disorder. KEY WORDS asphyxiation, “choking games,” hypoxia/anoxia, lethal, WHAT THIS STUDY ADDS: AEA is little known beyond forensic masochism/sadism, sexual stimulation, suffocation, suicide medicine and is generally regarded as a curiosity rather than a ABBREVIATION medical disorder whose onset is in childhood or adolescence. AEA—autoerotic asphyxiation This study adds understanding of causation and provides guidance to www.pediatrics.org/cgi/doi/10.1542/peds.2009-0730 pediatricians on recognition and management. doi:10.1542/peds.2009-0730 Accepted for publication Jun 4, 2009 Address correspondence to Daniel D. Cowell, MD, MLS, CPHQ, Departments of Psychiatry and Behavioral Medicine, and Graduate Medical Education, Marshall University, Joan C. abstract Edwards School of Medicine, 1600 Medical Center Dr, Suite 3414, Huntington, WV 25701. E-mail: [email protected] OBJECTIVE: Voluntary asphyxiation among children, preteens, and ad- PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275). olescents by hanging or other means of inducing hypoxia/anoxia to Copyright © 2009 by the American Academy of Pediatrics enhance sexual excitement is not uncommon and can lead to unin- FINANCIAL DISCLOSURE: The author has indicated he has no tended death. -
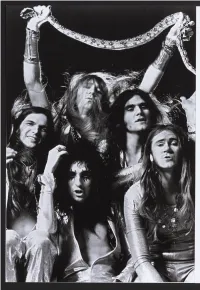
Alice Cooper 2011.Pdf
® • • • I ’ M - I N - T HE - MIDDLE-WIT HOUT ANT PLANS - I’M A BOY AND I’M-A MAN - I.’ M EIGHTEEN- - ® w Q < o ¡a 2 Ó z s * Tt > o ALICE M > z o g «< COOPER s [ BY BRAD T O L I N S K I ] y a n y standards, short years before, in 1967, Alice Cooper 1973 was an had been scorned as “the most hated exceptional year band” in Los Angeles. The group members for rock & roll. weirded out the locals by being the first Its twelve months hoys that weren’t transvestites to dress as saw the release girls, and their wildly dissonant, fuzzed- of such gems as out psychedelia sent even the most liberal Pink Floyd s The Dark Side of the Moon, hippies fleeing for the door. Any rational H H Led Zeppelin s Houses of the Holy, the human would have said they were 0 o W ho’s Quadrophenia, Stevie Wonders committing professional suicide, but z Innervisions, Elton Johns Goodbye Yellow the band members thought otherwise. Brick Road, and debuts from Lynyrd Who cared if a bunch o f Hollywood squares Skynyrd, Aerosmith, Queen, and the New thought they were gay? At least they Y ork D olls. were being noticed. But the most T H E BAND Every time they provocative and heard somebody audacious treasure G R A B B E D y e ll “faggot;” they of that banner year H EA D LIN ES AND swished more, and was Alice Coopers overnight they found £ o masterpiece, B illio n MADE WAVES fame as the group z w Dollar Babies, a it was hip to hate H m brilliant lampoon of American excess. -

Indian Country Issues
Indian Country Issues In Tbis Issue . Jurisdictional Conflicts Between Tribes and States: Disputes Over Land Set Aside Pursuant to the Indian Reorganization Act and July Reservation Boundary Disputes .............................. 1 2014 By Gina Allery and Darou T. Carreiro Volume62 Number4 Protecting the Civil Rights of American Indians and Alaska Natives: The Civil Rights Division's Indian Working Group ............. 10 Uniled,States By Verlin Deerinwater and Susana Lorenzo-Giguere Department of1\lstice l!!:xeeutive Office fur United States Altom.y. Wubington, DC Reentry Programming in Indian Country: Building the Third Leg 20530 of the Stool ............................................... 16 Monty Wilkinson By Timothy Q. Purdon Director Contributors' opinions and statements Native Children Exposed to Violence: Defending Childhood in should not be considered an Indian Country and Alaska Native Communities ............... 22 endorsoment by EOUSA fur any poJicy1 program, or service By Amanda Marshall Tbe United Statos Altomeys' Bulletin is published plll'$uant to Investigating and Prosecuting the Non-Fatal Strangulation Case .. 28 28 CFR § 0 22(b) By Leslie A. Hagen Tbe United StaleS Altornoys' Bulletin ;. publilbed bJmonthly by the Executive Office fur United States Native American Graves Protection and Repatriation Act Attorney., Offico ofLegall!dueation, 1620Pendleto.IIStreet, (NAGPRA): The Law Is Not an Authorization for Disinterment . .41 Columbia, Seulh Carolina 29201 By Sherry Hutt and David Tarler Manaatn~ Editor The Investigation