Expression of Placenta Growth Factor Is Associated with Unfavorable Prognosis of Advanced-Stage Serous Ovarian Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ARTICLES Fibroblast Growth Factors 1, 2, 17, and 19 Are The
0031-3998/07/6103-0267 PEDIATRIC RESEARCH Vol. 61, No. 3, 2007 Copyright © 2007 International Pediatric Research Foundation, Inc. Printed in U.S.A. ARTICLES Fibroblast Growth Factors 1, 2, 17, and 19 Are the Predominant FGF Ligands Expressed in Human Fetal Growth Plate Cartilage PAVEL KREJCI, DEBORAH KRAKOW, PERTCHOUI B. MEKIKIAN, AND WILLIAM R. WILCOX Medical Genetics Institute [P.K., D.K., P.B.M., W.R.W.], Cedars-Sinai Medical Center, Los Angeles, California 90048; Department of Obstetrics and Gynecology [D.K.] and Department of Pediatrics [W.R.W.], UCLA School of Medicine, Los Angeles, California 90095 ABSTRACT: Fibroblast growth factors (FGF) regulate bone growth, (G380R) or TD (K650E) mutations (4–6). When expressed at but their expression in human cartilage is unclear. Here, we deter- physiologic levels, FGFR3-G380R required, like its wild-type mined the expression of entire FGF family in human fetal growth counterpart, ligand for activation (7). Similarly, in vitro cul- plate cartilage. Using reverse transcriptase PCR, the transcripts for tivated human TD chondrocytes as well as chondrocytes FGF1, 2, 5, 8–14, 16–19, and 21 were found. However, only FGF1, isolated from Fgfr3-K644M mice had an identical time course 2, 17, and 19 were detectable at the protein level. By immunohisto- of Fgfr3 activation compared with wild-type chondrocytes and chemistry, FGF17 and 19 were uniformly expressed within the showed no receptor activation in the absence of ligand (8,9). growth plate. In contrast, FGF1 was found only in proliferating and hypertrophic chondrocytes whereas FGF2 localized predominantly to Despite the importance of the FGF ligand for activation of the resting and proliferating cartilage. -

Pathophysiological Roles of FGF Signaling in the Heart
MINI REVIEW ARTICLE published: 06 September 2013 doi: 10.3389/fphys.2013.00247 Pathophysiological roles of FGF signaling in the heart Nobuyuki Itoh* and Hiroya Ohta Department of Genetic Biochemistry, Kyoto University Graduate School of Pharmaceutical Sciences, Kyoto, Japan Edited by: Cardiac remodeling progresses to heart failure, which represents a major cause of Marcel van der Heyden, University morbidity and mortality. Cardiomyokines, cardiac secreted proteins, may play roles Medical Center, Netherlands in cardiac remodeling. Fibroblast growth factors (FGFs) are secreted proteins with Reviewed by: diverse functions, mainly in development and metabolism. However, some FGFs play Marcel van der Heyden, University Medical Center, Netherlands pathophysiological roles in cardiac remodeling as cardiomyokines. FGF2 promotes cardiac Christian Faul, University of Miami hypertrophy and fibrosis by activating MAPK signaling through the activation of FGF Miller School of Medicine, USA receptor (FGFR) 1c. In contrast, FGF16 may prevent these by competing with FGF2 for the *Correspondence: binding site of FGFR1c. FGF21 prevents cardiac hypertrophy by activating MAPK signaling Nobuyuki Itoh, Department of through the activation of FGFR1c with β-Klotho as a co-receptor. In contrast, FGF23 Genetic Biochemistry, Kyoto α University Graduate School of induces cardiac hypertrophy by activating calcineurin/NFAT signaling without Klotho. Pharmaceutical Sciences, These FGFs play crucial roles in cardiac remodeling via distinct action mechanisms. These Yoshida-Shimoadachi, Sakyo, findings provide new insights into the pathophysiological roles of FGFs in the heart and Kyoto 606-8501, Japan may provide potential therapeutic strategies for heart failure. e-mail: itohnobu@ pharm.kyoto-u.ac.jp Keywords: FGF, heart, hypertrophy, fibrosis, heart failure, cardiomyokine INTRODUCTION mice and humans, respectively. -

Instability Restricts Signaling of Multiple Fibroblast Growth Factors
Cell. Mol. Life Sci. DOI 10.1007/s00018-015-1856-8 Cellular and Molecular Life Sciences RESEARCH ARTICLE Instability restricts signaling of multiple fibroblast growth factors Marcela Buchtova • Radka Chaloupkova • Malgorzata Zakrzewska • Iva Vesela • Petra Cela • Jana Barathova • Iva Gudernova • Renata Zajickova • Lukas Trantirek • Jorge Martin • Michal Kostas • Jacek Otlewski • Jiri Damborsky • Alois Kozubik • Antoni Wiedlocha • Pavel Krejci Received: 18 June 2014 / Revised: 7 February 2015 / Accepted: 9 February 2015 Ó Springer Basel 2015 Abstract Fibroblast growth factors (FGFs) deliver ex- failure to activate FGF receptor signal transduction over tracellular signals that govern many developmental and long periods of time, and influence specific cell behavior regenerative processes, but the mechanisms regulating FGF in vitro and in vivo. Stabilization via exogenous heparin signaling remain incompletely understood. Here, we ex- binding, introduction of stabilizing mutations or lowering plored the relationship between intrinsic stability of FGF the cell cultivation temperature rescues signaling of un- proteins and their biological activity for all 18 members of stable FGFs. Thus, the intrinsic ligand instability is an the FGF family. We report that FGF1, FGF3, FGF4, FGF6, important elementary level of regulation in the FGF sig- FGF8, FGF9, FGF10, FGF16, FGF17, FGF18, FGF20, and naling system. FGF22 exist as unstable proteins, which are rapidly de- graded in cell cultivation media. Biological activity of Keywords Fibroblast growth factor Á FGF Á Unstable Á FGF1, FGF3, FGF4, FGF6, FGF8, FGF10, FGF16, FGF17, Proteoglycan Á Regulation and FGF20 is limited by their instability, manifesting as Electronic supplementary material The online version of this article (doi:10.1007/s00018-015-1856-8) contains supplementary material, which is available to authorized users. -

FGF Signaling Network in the Gastrointestinal Tract (Review)
163-168 1/6/06 16:12 Page 163 INTERNATIONAL JOURNAL OF ONCOLOGY 29: 163-168, 2006 163 FGF signaling network in the gastrointestinal tract (Review) MASUKO KATOH1 and MASARU KATOH2 1M&M Medical BioInformatics, Hongo 113-0033; 2Genetics and Cell Biology Section, National Cancer Center Research Institute, Tokyo 104-0045, Japan Received March 29, 2006; Accepted May 2, 2006 Abstract. Fibroblast growth factor (FGF) signals are trans- Contents duced through FGF receptors (FGFRs) and FRS2/FRS3- SHP2 (PTPN11)-GRB2 docking protein complex to SOS- 1. Introduction RAS-RAF-MAPKK-MAPK signaling cascade and GAB1/ 2. FGF family GAB2-PI3K-PDK-AKT/aPKC signaling cascade. The RAS~ 3. Regulation of FGF signaling by WNT MAPK signaling cascade is implicated in cell growth and 4. FGF signaling network in the stomach differentiation, the PI3K~AKT signaling cascade in cell 5. FGF signaling network in the colon survival and cell fate determination, and the PI3K~aPKC 6. Clinical application of FGF signaling cascade in cell polarity control. FGF18, FGF20 and 7. Clinical application of FGF signaling inhibitors SPRY4 are potent targets of the canonical WNT signaling 8. Perspectives pathway in the gastrointestinal tract. SPRY4 is the FGF signaling inhibitor functioning as negative feedback apparatus for the WNT/FGF-dependent epithelial proliferation. 1. Introduction Recombinant FGF7 and FGF20 proteins are applicable for treatment of chemotherapy/radiation-induced mucosal injury, Fibroblast growth factor (FGF) family proteins play key roles while recombinant FGF2 protein and FGF4 expression vector in growth and survival of stem cells during embryogenesis, are applicable for therapeutic angiogenesis. Helicobacter tissues regeneration, and carcinogenesis (1-4). -

Supplementary Information
Supplementary information Supplemental Figure 1. No tissue contamination is confirmed by immunostaining of anti-MHC antibodies in the human-mouse heterogeneous recombination. A: The mesenchymally exclusive expression of human MHC in recombinant of mouse dental epithelium and human dental mesenchyme after subrenal culture for 4 weeks. B: The mesenchymally exclusive expression of mouse MHC in the recombinant of human dental epithelium and mouse dental mesenchyme after subrenal culture for 7 days. C: The epithelially exclusive expression of human MHC in the recombinant of human dental epithelium and mouse dental mesenchyme after subrenal culture for 7 days. hdm, human bell-stage dental mesenchyme; mam, mouse ameloblasts; mdm, E13.5 mouse dental mesenchyme; hde, human bell-stage dental epithelium. Scale bar = 50 μm. Supplemental Figure 2. Expression pattern of FGF1, FGF2, FGF15/19, and FGF18 in human tooth germs at the cap and bell stages. In situ hybridization shows the expression of FGF1 (A, B), FGF2 (C, D), FGF15/19 (E, F), and FGF18 (G, H) in human molar germs at the cap (A, C, E, G) and bell (B, D, F, H) stages. de, dental epithelium; dm, dental mesenchyme; ek, enamel knot; sr, stellate reticulum; iee, inner enamel epithelium. Scale bar = 50 μm. Supplemental Figure 3. Fgf8 is ectopically expressed in E13.5 molar germs of Wnt1-Cre;R26RFgf8 mice. Immunostaining of FGF8 in E13.5 wild-type (A) and mutant (B) molar germs. de, dental epithelium; dm, dental mesenchyme. Scale bar: 50 μm. Supplemental Table 1. Comparison of the expression pattern of FGF ligands between human and mouse tooth germ at the cap and bell stages. -

DNA Hypermethylation of Fgf16 and Tbx22 Associated with Cleft Palate During Palatal Fusion
Original Article http://dx.doi.org/10.1590/1678-7757-2018-0649 DNA hypermethylation of Fgf16 and Tbx22 associated with cleft palate during palatal fusion Abstract Xuan SHU1 Objective: Cleft palate (CP) is a congenital birth defect caused by the failure of palatal fusion. Little is known about the potential role of DNA methylation Zejun DONG1 in the pathogenesis of CP. This study aimed to explore the potential role of Liuhanghang CHENG1 DNA methylation in the mechanism of CP. Methodology: We established an Shenyou SHU1 all-trans retinoic acid (ATRA)-induced CP model in C57BL/6J mice and used methylation-dependent restriction enzymes (MethylRAD, FspEI) combined with high-throughput sequencing (HiSeq X Ten) to compare genome-wide DNA methylation profiles of embryonic mouse palatal tissues, between embryos from ATRA-treated vs. untreated mice, at embryonic gestation day 14.5 (E14.5) (n=3 per group). To confirm differentially methylated levels of susceptible genes, real-time quantitative PCR (qPCR) was used to correlate expression of differentially methylated genes related to CP. Results: We identified 196 differentially methylated genes, including 17,298 differentially methylated CCGG sites between ATRA-treated vs. untreated embryonic mouse palatal tissues (P<0.05, log2FC>1). The CP-related genes Fgf16 (P=0.008, log2FC=1.13) and Tbx22 (P=0.011, log2FC=1.64,) were hypermethylated. Analysis of Fgf16 and Tbx22, using Gene Ontology (GO) and the Kyoto Encyclopedia of Genes and Genomes (KEGG), identified 3 GO terms and 1 KEGG pathway functionally related to palatal fusion. The qPCR showed that changes in expression level negatively correlated with methylation levels. -

Expression of Fgfs During Early Mouse Tongue Development
Gene Expression Patterns 20 (2016) 81e87 Contents lists available at ScienceDirect Gene Expression Patterns journal homepage: http://www.elsevier.com/locate/gep Expression of FGFs during early mouse tongue development * Wen Du a, b, Jan Prochazka b, c, Michaela Prochazkova b, c, Ophir D. Klein b, d, a State Key Laboratory of Oral Diseases, West China Hospital of Stomatology, Sichuan University, Chengdu, Sichuan, 610041, China b Department of Orofacial Sciences and Program in Craniofacial Biology, University of California San Francisco, San Francisco, CA 94143, USA c Laboratory of Transgenic Models of Diseases, Institute of Molecular Genetics of the ASCR, v.v.i., Prague, Czech Republic d Department of Pediatrics and Institute for Human Genetics, University of California San Francisco, San Francisco, CA 94143, USA article info abstract Article history: The fibroblast growth factors (FGFs) constitute one of the largest growth factor families, and several Received 29 September 2015 ligands and receptors in this family are known to play critical roles during tongue development. In order Received in revised form to provide a comprehensive foundation for research into the role of FGFs during the process of tongue 13 December 2015 formation, we measured the transcript levels by quantitative PCR and mapped the expression patterns by Accepted 29 December 2015 in situ hybridization of all 22 Fgfs during mouse tongue development between embryonic days (E) 11.5 Available online 31 December 2015 and E14.5. During this period, Fgf5, Fgf6, Fgf7, Fgf9, Fgf10, Fgf13, Fgf15, Fgf16 and Fgf18 could all be detected with various intensities in the mesenchyme, whereas Fgf1 and Fgf2 were expressed in both the Keywords: Tongue epithelium and the mesenchyme. -

FGF/FGFR Signaling in Health and Disease
Signal Transduction and Targeted Therapy www.nature.com/sigtrans REVIEW ARTICLE OPEN FGF/FGFR signaling in health and disease Yangli Xie1, Nan Su1, Jing Yang1, Qiaoyan Tan1, Shuo Huang 1, Min Jin1, Zhenhong Ni1, Bin Zhang1, Dali Zhang1, Fengtao Luo1, Hangang Chen1, Xianding Sun1, Jian Q. Feng2, Huabing Qi1 and Lin Chen 1 Growing evidences suggest that the fibroblast growth factor/FGF receptor (FGF/FGFR) signaling has crucial roles in a multitude of processes during embryonic development and adult homeostasis by regulating cellular lineage commitment, differentiation, proliferation, and apoptosis of various types of cells. In this review, we provide a comprehensive overview of the current understanding of FGF signaling and its roles in organ development, injury repair, and the pathophysiology of spectrum of diseases, which is a consequence of FGF signaling dysregulation, including cancers and chronic kidney disease (CKD). In this context, the agonists and antagonists for FGF-FGFRs might have therapeutic benefits in multiple systems. Signal Transduction and Targeted Therapy (2020) 5:181; https://doi.org/10.1038/s41392-020-00222-7 INTRODUCTION OF THE FGF/FGFR SIGNALING The binding of FGFs to the inactive monomeric FGFRs will Fibroblast growth factors (FGFs) are broad-spectrum mitogens and trigger the conformational changes of FGFRs, resulting in 1234567890();,: regulate a wide range of cellular functions, including migration, dimerization and activation of the cytosolic tyrosine kinases by proliferation, differentiation, and survival. It is well documented phosphorylating the tyrosine residues within the cytosolic tail of that FGF signaling plays essential roles in development, metabo- FGFRs.4 Then, the phosphorylated tyrosine residues serve as the lism, and tissue homeostasis. -

Halotag Is an Effective Expression and Solubilisation Fusion Partner for a Range of Fibroblast Growth Factors
HaloTag is an eVective expression and solubilisation fusion partner for a range of fibroblast growth factors Changye Sun1,3 , Yong Li1,3 , Sarah E. Taylor1, Xianqing Mao2, Mark C. Wilkinson1 and David G. Fernig1 1 Department of Biochemistry, Institute of Integrative Biology, University of Liverpool, Liverpool, UK 2 Department of Oncology, Laboratory of Cellular and Molecular Oncology, Luxembourg Institute of Health, Luxembourg 3 These authors contributed equally to this work. ABSTRACT The production of recombinant proteins such as the fibroblast growth factors (FGFs) is the key to establishing their function in cell communication. The production of recombinant FGFs in E. coli is limited, however, due to expression and solubility problems. HaloTag has been used as a fusion protein to introduce a genetically- encoded means for chemical conjugation of probes. We have expressed 11 FGF proteins with an N-terminal HaloTag, followed by a tobacco etch virus (TEV) protease cleavage site to allow release of the FGF protein. These were purified by heparin-aYnity chromatography, and in some instances by further ion-exchange chromatography. It was found that HaloTag did not adversely aVect the expression of FGF1 and FGF10, both of which expressed well as soluble proteins. The N-terminal HaloTag fusion was found to enhance the expression and yield of FGF2, FGF3 and FGF7. Moreover, whereas FGF6, FGF8, FGF16, FGF17, FGF20 and FGF22 were only expressed as insoluble proteins, their N-terminal HaloTag fusion counterparts (Halo-FGFs) were soluble, and could be successfully purified. However, cleavage of Halo-FGF6, -FGF8 and -FGF22 with TEV resulted in aggregation of the FGF protein. -

Dissertation LFS Corrected 08-22-16
EXPRESSION AND ROLE OF FIBROBLAST GROWTH FACTOR 9 (FGF9) IN BOVINE FOLLICULOGENESIS By LUÍS FERNANDO SCHÜTZ Doctor of Veterinary Medicine Federal University of Rio Grande do Sul Porto Alegre, Brazil 2007 Master of Science in Animal Science Santa Catarina State University Lages, Brazil Submitted to the Faculty of the Graduate College of the Oklahoma State University in partial fulfillment of the requirements for the Degree of DOCTOR OF PHILOSOPHY July, 2016 EXPRESSION AND ROLE OF FIBROBLAST GROWTH FACTOR 9 (FGF9) IN BOVINE FOLLICULOGENESIS Dissertation Approved: Dr. Leon J. Spicer Dissertation Adviser Dr. Robert Wettemann Dr. Glenn Zhang Dr. Peter Hoyt ii ACKNOWLEDGEMENTS To my beloved wife, for her love, support, encouragement, and understanding. She made all the steps of the arduous pathway to achieve this degree much easier. With her by my side, I feel much stronger. To my family in Brazil: my beloved parents, my brother, Lipe, and my sister, Ane, for their love, faith, and support. And to my beautiful niece, Sofia, my sister-in-law, Manuela, and my brother-in-law, Joni. To my advisor and mentor, Dr. Leon Spicer, for accepting me as a student, for giving me priceless lessons and advice whenever I needed, for stimulating me to develop a critical thinking, and for teaching me how to perform sound science in the field of ovarian folliculogenesis. And to his family, Michael, Melissa, Anna, and Richie, for their friendship and support. To the Franceschi family: my mother-in-law, Pierina, and my father-in-law, Adi, for their support and encouragement; to my brother-in-law, Junior, his wife, Janine, and his great boys, Bernardo and Bruno; and to my sister-in-law, Sheila, and her fiancé, Fábio. -
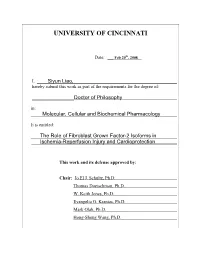
University of Cincinnati
UNIVERSITY OF CINCINNATI Date: ___ Feb 20th, 2008 I, Siyun Liao, hereby submit this work as part of the requirements for the degree of: ________________Doctor of Philosophy in: Molecular, Cellular and Biochemical Pharmacology It is entitled: ____The Role of Fibroblast Grown Factor-2 Isoforms in ___Ischemia-Reperfusion Injury and Cardioprotection This work and its defense approved by: Chair: Jo El J. Schultz, Ph.D. Thomas Doetschman, Ph.D. W. Keith Jones, Ph.D. Evangelia G. Kranias, Ph.D. Mark Olah, Ph.D. Hong-Sheng Wang, Ph.D. THE ROLE OF FIBROBLAST GROWTH FACTOR-2 ISOFORMS IN ISCHEMIA- REPERFUSION INJURY AND CARDIOPROTECTION A dissertation submitted to the Division of Graduate Studies of the University of Cincinnati In partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY In the Department of Pharmacology and Cell Biophysics 2007 by Siyun Liao B.S. China Pharmaceutical University, 2000 Committee Chair: Dr. Jo El J. Schultz ii Abstract Cardiovascular disease (CVD) remains the leading cause of death in the United States and in the developing world, with ischemic heart disease the second most common form of CVD. Experimental and clinical studies have demonstrated that a number of interventions, including brief periods of ischemia or hypoxia and certain endogenous molecules such as growth factors, opioids, adenosine or pharmacological agents are capable of protecting the heart against post- ischemic cardiac dysfunction, arrhythmias and myocardial infarction. One of these growth factors, fibroblast growth factor-2 (FGF2), has been implicated to be a cardioprotective molecule. FGF2 consists of multiple protein isoforms (low molecular weight, LMW, and high molecular weight, HMW) produced by alternative translation from the Fgf2 gene and these protein isoforms are localized to different cellular compartments indicating unique biological activity. -

Termination of Receptor Tyrosine Kinase Signal
International Journal of Molecular Sciences Review All Good Things Must End: Termination of Receptor Tyrosine Kinase Signal Azzurra Margiotta 1,2 1 Department of Biology, Faculty of Medicine, Masaryk University, 62500 Brno, Czech Republic; [email protected] 2 International Clinical Research Center, St. Anne’s University Hospital, 65691 Brno, Czech Republic Abstract: Receptor tyrosine kinases (RTKs) are membrane receptors that regulate many fundamental cellular processes. A tight regulation of RTK signaling is fundamental for development and survival, and an altered signaling by RTKs can cause cancer. RTKs are localized at the plasma membrane (PM) and the major regulatory mechanism of signaling of RTKs is their endocytosis and degradation. In fact, RTKs at the cell surface bind ligands with their extracellular domain, become active, and are rapidly internalized where the temporal extent of signaling, attenuation, and downregulation are modulated. However, other mechanisms of signal attenuation and termination are known. Indeed, inhibition of RTKs’ activity may occur through the modulation of the phosphorylation state of RTKs and the interaction with specific proteins, whereas antagonist ligands can inhibit the biological responses mediated by the receptor. Another mechanism concerns the expression of endogenous inactive receptor variants that are deficient in RTK activity and take part to inactive heterodimers or hetero-oligomers. The downregulation of RTK signals is fundamental for several cellular functions and the homeostasis of the cell. Here, we will review the mechanisms of signal attenuation and termination of RTKs, focusing on FGFRs. Keywords: RTKs; FGFRs; termination of signaling; degradation; ubiquitination; PTPs; kinases Citation: Margiotta, A. All Good Things Must End: Termination of Receptor Tyrosine Kinase Signal.