Discussion Papers on HIV/AIDS Care and Support
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Liste Représentative Du Patrimoine Culturel Immatériel De L'humanité
Liste représentative du patrimoine culturel immatériel de l’humanité Date de Date récente proclamation Intitulé officiel Pays d’inscriptio Référence ou première n inscription Al-Ayyala, un art traditionnel du Oman - Émirats spectacle dans le Sultanat d’Oman et 2014 2014 01012 arabes unis aux Émirats arabes unis Al-Zajal, poésie déclamée ou chantée Liban 2014 2014 01000 L’art et le symbolisme traditionnels du kelaghayi, fabrication et port de foulards Azerbaïdjan 2014 2014 00669 en soie pour les femmes L’art traditionnel kazakh du dombra kuï Kazakhstan 2014 2014 00011 L’askiya, l’art de la plaisanterie Ouzbékistan 2014 2014 00011 Le baile chino Chili 2014 2014 00988 Bosnie- La broderie de Zmijanje 2014 2014 00990 Herzégovine Le cante alentejano, chant polyphonique Portugal 2014 2014 01007 de l’Alentejo (sud du Portugal) Le cercle de capoeira Brésil 2014 2014 00892 Le chant traditionnel Arirang dans la République 2014 2014 00914 République populaire démocratique de populaire Date de Date récente proclamation Intitulé officiel Pays d’inscriptio Référence ou première n inscription Corée démocratique de Corée Les chants populaires ví et giặm de Viet Nam 2014 2014 01008 Nghệ Tĩnh Connaissances et savoir-faire traditionnels liés à la fabrication des Kazakhstan - 2014 2014 00998 yourtes kirghizes et kazakhes (habitat Kirghizistan nomade des peuples turciques) La danse rituelle au tambour royal Burundi 2014 2014 00989 Ebru, l’art turc du papier marbré Turquie 2014 2014 00644 La fabrication artisanale traditionnelle d’ustensiles en laiton et en -

A Feminist Critique of Knowledge Production
This volume is the result of the close collaboration between the University of Naples “L‘Orientale” and the scholars organizing and participating to the postgraduate course Feminisms in a Transnational Perspective in Dubrovnik, Croatia. It features 15 essays that envision a feminist critique of the production Università degli studi di Napoli of knowledge that contributes today, intentionally or not, to new “L’Orientale” forms of discrimination, hierarchy control, and exclusion. Opposing the skepticism towards the viability of Humanities and Social Sciences in the era of ‘banking education’, marketability, and the so-called technological rationalization, these essays inquiry into teaching practices of non- institutional education and activism. They practice methodological ‘diversions’ of feminist intervention A feminist critique into Black studies, Childhood studies, Heritage studies, Visual studies, and studies of Literature. of knowledge production They venture into different research possibilities such as queering Eurocentric archives and histories. Some authors readdress Monique production A feminist critique of knowledge Wittig’s thought on literature as the Trojan horse amidst academy’s walls, the war-machine whose ‘design and goal is to pulverize the old forms and formal conventions’. Others rely on the theoretical assumptions of minor transnationalism, deconstruction, edited by Deleuzian nomadic feminism, queer theory, women’s oral history, and Silvana Carotenuto, the theory of feminist sublime. Renata Jambrešic ´ Kirin What connects these engaged writings is the confidence in the ethics and Sandra Prlenda of art and decolonized knowledge as a powerful tool against cognitive capitalism and the increasing precarisation of human lives and working conditions that go hand in hand with the process of annihilating Humanities across Europe. -

Bulletin POLISH NATIONAL COMMISSION
biuletyn 2013 PRZEGLÑD POLSKIEGO KOMITETU DO SPRAW UNESCO PRZEGLÑD POLSKIEGO KOMITETU DO SPRAW UNESCO biuletynbiuletyn|| 2013 2013 POLISH NATIONAL COMMISSION for UNESCO Reviev bulletin | bulletin | for UNESCO Review UNESCO for POLISH NATIONAL COMMISSION COMMISSION NATIONAL POLISH bulletin 2013 covBIUL13gr.indd 1 14-11-03 14:34 POLISH NATIONAL COMMISSION for UNESCO Review bulletin| 2013 Table of Contents Andrzej Rottermund Workshop for Restorers A Few Words 53 in Nesvizh 5 About Our Activities Last Year Marek Konopka UNESCO 55 Anamnesis – Re-minding Programme Priorities 8 for the Coming Years 61 Kraków – UNESCO City of Literature What We Dealt with Sławomir Ratajski 12 in 2013 UNESCO 2005 Convention 63 A Tool of Cultural Policy Why and How to Protect Cultural 21 Heritage by Modern Means? Intercultural Education Workshops 72 for Teachers Bogusław Szmygin Protecting Our Heritage Libyan Journalists 25 – Contemporary Approach 73 on a Study Visit to Poland Leszek Kolankiewicz The Concept of Intangible Euro-Arab Dialogue Conference Cultural Heritage “Our Commonly Shared Values” 32 in the 2003 Convention 75 held in Algarve Mariusz Czuba Anna Kalinowska Wooden Orthodox Churches Contemporary Man In Dialogue (Tserkvas) of the Polish 77 With The Environment? and Ukrainian Carpathian Region 43 on the World Heritage List Magdalena Machinko-Nagrabecka How to Teach Katarzyna Piotrowska 85 on Sustainable Development? Wieliczka and Bochnia Royal Salt Mines Educating in Dialogue 46 on UNESCO World Heritage List 90 with the Environment 93 ASPnet for Global -

POSTER PRESENTATIONS All Poster Presentations Will Be Located in the Thomas Field House
POSTER PRESENTATIONS All Poster Presentations will be located in the Thomas Field House 8:30-10:00 POSTER PRESENTATIONS BIOLOGY Amy Kutay Monitoring levels of immunoglobulins using immunoprecipitation Jessie L. Burns 3 Dimensional models in biology Erika K. Bullock Heather Bechtold Lab research poster presentations The Impact of Invasive Worm Species on Soil Nutrients and the Native Flora Within an Ecosystem Mary K. Arnold Pavlovian Plants Cody M. Iannozzi Pesticides and Algae: a look at effects on GPP Benjamin A. Tripoli Carina Howell Research in Developmental Biology Effects of Aquatic Toxins on the Development of Xenopus Embryos Courtney Capper The Teratogenic Effects of Bisphenol A on Xenopus laevis Kevin Hulings Jay Lunden Antarctic Invertebrates on Acid: Effects of Changing Ocean Chemistry on Larval Sea Urchins at McMurdo Station, Antarctica Sara K. Sette Jennifer Deitloff Research in Herpetology Mating Behaviors of Eurycea Wilderae Samantha P. Wesnak Comparing Population and Sex Differences in Head Shape for Four Populations of Red-Backed Salamanders in Pennsylvania Landon S. Allen Effect of Silver Nanoparticles on Xenopus Tadpoles Mariah A. Cardoza Joseph Calabrese Preliminary Studies into the Prokaryotic Microbiome associated with Bat Guano (Myotis lucifugus) from a Maternity Colony. Samantha M. Dutton, Breanna N. Glacken Investigating the Microbiome of Myotis lucifugus Populations and Potential for Prokaryotic Isolates as Biocontrol Agents of White Nose Syndrome Max V. Cravener Ted Nuttall Genetic Counseling Naomi S. Kriner CHEMISTRY Laura Lee Chemistry Research Poster Session Analysis of Natural Sugars by High Performance Liquid Chromatography Carley A. Bennett Bomb Calorimetry of Cycloalkanes Anmarie Misterkiewicz Extraction and Identification of Compounds from Morning Glory Seeds Meagan E. -

List of the 90 Masterpieces of the Oral and Intangible Heritage
Albania • Albanian Folk Iso-Polyphony (2005) Algeria • The Ahellil of Gourara (2005) Armenia • The Duduk and its Music (2005) Azerbaijan • Azerbaijani Mugham (2003) List of the 90 Masterpieces Bangladesh • Baul Songs (2005) of the Oral and Belgium • The Carnival of Binche (2003) Intangible Belgium, France Heritage of • Processional Giants and Dragons in Belgium and Humanity France (2005) proclaimed Belize, Guatemala, by UNESCO Honduras, Nicaragua • Language, Dance and Music of the Garifuna (2001) Benin, Nigeria and Tog o • The Oral Heritage of Gelede (2001) Bhutan • The Mask Dance of the Drums from Drametse (2005) Bolivia • The Carnival Oruro (2001) • The Andean Cosmovision of the Kallawaya (2003) Brazil • Oral and Graphic Expressions of the Wajapi (2003) • The Samba de Roda of Recôncavo of Bahia (2005) Bulgaria • The Bistritsa Babi – Archaic Polyphony, Dances and Rituals from the Shoplouk Region (2003) Cambodia • The Royal Ballet of Cambodia (2003) • Sbek Thom, Khmer Shadow Theatre (2005) Central African Republic • The Polyphonic Singing of the Aka Pygmies of Central Africa (2003) China • Kun Qu Opera (2001) • The Guqin and its Music (2003) • The Uyghur Muqam of Xinjiang (2005) Colombia • The Carnival of Barranquilla (2003) • The Cultural Space of Palenque de San Basilio (2005) Costa Rica • Oxherding and Oxcart Traditions in Costa Rica (2005) Côte d’Ivoire • The Gbofe of Afounkaha - the Music of the Transverse Trumps of the Tagbana Community (2001) Cuba • La Tumba Francesa (2003) Czech Republic • Slovácko Verbunk, Recruit Dances (2005) -

State of the World's Minorities and Indigenous Peoples 2013
Focus on health minority rights group international State of the World’s Minorities and Indigenous Peoples 2013 Events of 2012 State of theWorld’s Minorities and Indigenous Peoples 20131 Events of 2012 Front cover: A Dalit woman who works as a Community Public Health Promoter in Nepal. Jane Beesley/Oxfam GB. Inside front cover: Indigenous patient and doctor at Klinik Kalvary, a community health clinic in Papua, Indonesia. Klinik Kalvary. Inside back cover: Roma child at a community centre in Slovakia. Bjoern Steinz/Panos Acknowledgements Support our work Minority Rights Group International (MRG) Donate at www.minorityrights.org/donate gratefully acknowledges the support of all organizations MRG relies on the generous support of institutions and individuals who gave financial and other assistance and individuals to help us secure the rights of to this publication, including CAFOD, the European minorities and indigenous peoples around the Union and the Finnish Ministry of Foreign Affairs. world. All donations received contribute directly to our projects with minorities and indigenous peoples. © Minority Rights Group International, September 2013. All rights reserved. Subscribe to our publications at www.minorityrights.org/publications Material from this publication may be reproduced Another valuable way to support us is to subscribe for teaching or for other non-commercial purposes. to our publications, which offer a compelling No part of it may be reproduced in any form for analysis of minority and indigenous issues and commercial purposes without the prior express original research. We also offer specialist training permission of the copyright holders. materials and guides on international human rights instruments and accessing international bodies. -

Roles of Communities and Ngos in Safeguarding ICH
Roles of communities and NGOs in safeguarding ICH Hanaholmen, Espoo, Finland 31 October 2019 Questions • Why community participation in safeguarding intangible cultural heritage? Why are communities so important? • What are the roles of NGOs? • What does the Convention for the Safeguarding of the Intangible Cultural Heritage say about the roles of communities and NGOs? © Centro de la Diversidad, 2013 • What has been the experience so far ? Hanaholmen, Espoo, Finland 31 October 2019 The Culture Conventions Protection of Cultural Property in the Event of Armed Conflict (1954) Prohibiting and Preventing the Illicit Import, Export and Transfer of Cultural Property (1970) Protection of the World Cultural and Natural Heritage (1972) Protection of the Underwater Cultural Heritage (2001) Safeguarding of the Intangible Cultural Heritage (2003) Protection and Promotion of the Diversity of Cultural Expressions (2005) Hanaholmen, Espoo, Finland 31 October 2019 The Convention today • Adopted in 2003; entered into force in 2006 • 178 States Parties to date Some other figures: o 176 accredited NGOs o 179 Periodic reports o 95 International Assistance o 488 inscriptions on the Lists 59 USL +429 RL Ramman: religious festival and ritual theatre of the Garhwal Himalayas, India o 20 Good safeguarding practices © IGNCA, Ministry of Culture, India o +100 countries benefitted from the global capacity-building programme Hanaholmen, Espoo, Finland 31 October 2019 Objectives of the Convention • To safeguard the intangible heritage of humanity • To raise awareness of the importance of ICH and ensure mutual appreciation thereof • To ensure respect for it • To provide for international cooperation and assistance Hanaholmen, Espoo, Finland 31 October 2019 The definition Article 2.1: • The ‘intangible cultural heritage’ … means the practices, representations, expressions, knowledge, skills – as well as the instruments, objects, artefacts and cultural spaces associated therewith – that communities, groups and, in some cases, individuals recognize as part of their cultural heritage. -
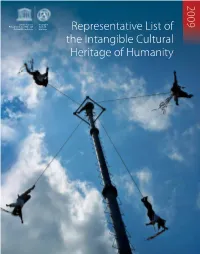
Representative List of the Intangible Cultural Heritage Of
RL cover [temp]:Layout 1 1/6/10 17:35 Page 2 2009 United Nations Intangible Educational, Scientific and Cultural Cultural Organization Heritage Representative List of the Intangible Cultural Heritage of Humanity RL cover [temp]:Layout 1 1/6/10 17:35 Page 5 Rep List 2009 2.15:Layout 1 26/5/10 09:25 Page 1 2009 Representative List of the Intangible Cultural Heritage of Humanity Rep List 2009 2.15:Layout 1 26/5/10 09:25 Page 2 © UNESCO/Michel Ravassard Foreword by Irina Bokova, Director-General of UNESCO UNESCO is proud to launch this much-awaited series of publications devoted to three key components of the 2003 Convention for the Safeguarding of the Intangible Cultural Heritage: the List of Intangible Cultural Heritage in Need of Urgent Safeguarding, the Representative List of the Intangible Cultural Heritage of Humanity, and the Register of Good Safeguarding Practices. The publication of these first three books attests to the fact that the 2003 Convention has now reached the crucial operational phase. The successful implementation of this ground-breaking legal instrument remains one of UNESCO’s priority actions, and one to which I am firmly committed. In 2008, before my election as Director-General of UNESCO, I had the privilege of chairing one of the sessions of the Intergovernmental Committee for the Safeguarding of the Intangible Cultural Heritage, in Sofia, Bulgaria. This enriching experience reinforced my personal convictions regarding the significance of intangible cultural heritage, its fragility, and the urgent need to safeguard it for future generations. Rep List 2009 2.15:Layout 1 26/5/10 09:25 Page 3 It is most encouraging to note that since the adoption of the Convention in 2003, the term ‘intangible cultural heritage’ has become more familiar thanks largely to the efforts of UNESCO and its partners worldwide. -

Representative List of the Intangible Cultural Heritage of Humanity As Heritage Fund
ElemeNts iNsCriBed iN 2012 oN the UrGeNt saFeguarding List, the represeNtatiVe List iNTANGiBLe CULtURAL HERITAGe aNd the reGister oF Best saFeguarding praCtiCes What is it? UNESCo’s ROLe iNTANGiBLe CULtURAL SECRETARIAT Intangible cultural heritage includes practices, representations, Since its adoption by the 32nd session of the General Conference in HERITAGe FUNd oF THE CoNVeNTION expressions, knowledge and know-how that communities recognize 2003, the Convention for the Safeguarding of the Intangible Cultural The Fund for the Safeguarding of the The List of elements of intangible cultural as part of their cultural heritage. Passed down from generation to Heritage has experienced an extremely rapid ratification, with over Intangible Cultural Heritage can contribute heritage is updated every year by the generation, it is constantly recreated by communities in response to 150 States Parties in the less than 10 years of its existence. In line with financially and technically to State Intangible Cultural Heritage Section. their environment, their interaction with nature and their history, the Convention’s primary objective – to safeguard intangible cultural safeguarding measures. If you would like If you would like to receive more information to participate, please send a contribution. about the 2003 Convention for the providing them with a sense of identity and continuity. heritage – the UNESCO Secretariat has devised a global capacity- Safeguarding of the Intangible Cultural building strategy that helps states worldwide, first, to create -

Signs of the Time: Kallawaya Medical Expertise and Social Reproduction in 21St Century Bolivia by Mollie Callahan a Dissertation
Signs of the Time: Kallawaya Medical Expertise and Social Reproduction in 21st Century Bolivia by Mollie Callahan A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Anthropology) in the University of Michigan 2011 Doctoral Committee: Professor Judith T. Irvine, Chair Professor Bruce Mannheim Associate Professor Barbra A. Meek Associate Professor Javier C. Sanjines Dedicada a la comunidad de Curva (en su totalidad) y mis primeros amores, Jorge y Luka. ii Acknowledgements There are many people without whom this dissertation would have never been conceived, let alone completed. I am indebted first and foremost to my mother, Lynda Lange, for bringing me into this world and imparting her passion for reading, politics, and people well before she managed to complete her bachelor’s degree and then masters late into my own graduate studies. She has for as long as I can remember wished for me to achieve all that I could imagine and more, despite the limitations she faced in pursuing her own professional aspirations early in her adult life. Out of self-less love, and perhaps the hope of also living vicariously through my own adventures, she has persistently encouraged me to follow my heart even when it has delivered me into harms way and far from her protective embrace. I am eternally grateful for the freedom she has given me to pursue my dreams far from home and without judgment. Her encouragement and excitement about my own process of scholarly discovery have sustained me throughout the research and writing of this dissertation. -

Traduccion Del Original Quechua
TRADUCCION DEL ORIGINAL QUECHUA PUEBLO QUECHUA v. MARRIOT INTERNATIONAL A) NOMBRE COMPLETO, NÚMERO DE DOCUMENTO NACIONAL DE IDENTIDAD Y DOMICILIO DE LA PERSONA NATURAL QUE PRESENTA LA INSTANCIA ESPECÍFICA. La presente Instancia Específica es presentada por indígenas del pueblo quechua, cuyos datos se consignan a continuación: --------- Torres ---------, con DNI -----------, con domicilio en ---------------, Cusco. ---------- Condori ----------, con DNI -----------, con domicilio en ---------------------, Cusco. ----------- Quispe ----------, con DNI ------------, con domicilio -----------------------------, Cusco. B) DIRECCIÓN(ES) DE CORREO(S) ELECTRÓNICO(S) EN EL/LOS QUE AUTORICE SE LE PUEDAN ENVIAR TODAS LAS NOTIFICACIONES CORRESPONDIENTES A LA INSTANCIA ESPECÍFICA. Las notificaciones en la presente Instancia Específica deberán ser enviadas a: ----------------- Con copia a: --------------------- C) EXPLICACIÓN ACERCA DEL INTERÉS CONCRETO QUE SE TIENE EN LA INSTANCIA ESPECÍFICA PLANTEADA. Los firmantes somos indígenas Quechuas, herederos de la tradición cultural de nuestros padres los inkas y practicantes de la religión andina de nuestros ancestros. Planteamos esta Instancia Específica a solicitud de miles de nuestros hermanos miembros de nuestras comunidades que no pueden apersonarse a esta Instancia Específica pues o habitan en lugares alejados de las alturas del Qosqo, o son iletrados o han sido amenazados por los constructores del Hotel “Four Points by Sheraton Cusco”. Nos apersonamos a esta Instancia Específica para evitar que continúe la destrucción de nuestro templo de Huacapuncu, se respete nuestro derecho humano a la conservación de nuestra cultura y se respete nuestra libertad religiosa. D) LA RAZÓN SOCIAL Y DOMICILIO DE NOTIFICACIÓN DE LA EMPRESA MULTINACIONAL QUE ESTÁ INCUMPLIENDO LAS DIRECTRICES, ASÍ COMO INFORMACIÓN ACERCA DE LA ESTRUCTURA ORGANIZACIONAL DE LA EMPRESA MULTINACIONAL, EN CASO RESULTE RELEVANTE PARA LA INSTANCIA ESPECÍFICA. -

The Heritage of Agriculture” Celebrate the World’S Heritage on 18 April 2010!
The International Day for Monuments and Sites Theme for 2010 – “The Heritage of Agriculture” Celebrate the world’s heritage on 18 April 2010! A contribution to the United Nations 2010 International Year of Biodiversity About the day On the proposal of ICOMOS, 18 April was endorsed as The International Day for Monuments and Sites by UNESCO in 1983. This special day offers an opportunity to raise public awareness concerning the diversity of the world’s heritage and the efforts that are required to protect and conserve it, as well as to draw attention to its vulnerability. For several years now, ICOMOS suggests a topic to be highlighted on this occasion. This has allowed our members and our committees to hold activities, conferences, colloquia or other events to raise awareness on this cultural heritage among the public, the owners or the public authorities by linking a global theme to local or national realities. We thank you in advance for all your initiatives and ask you to inform the ICOMOS Secretariat, as early as possible, of the activities you plan to undertake for 18 April, but also to share their results with us (programme, participation, publications). This will help us to disseminate information and to gather conclusions on all your activities, so as to be able to testify of the vitality of ICOMOS’ network. For further information on the Day, previous themes, support material and the calendar of activities foreseen in 2010 – consult http://www.international.icomos.org/18thapril/index.html. We will post information as it comes in. About the theme In the last two decades, the international NGO’s and public administrations in charge of heritage protection have begun to define and characterize the heritage of agriculture as well as to establish the criteria and tools that should guide the assessment of its values, protection and management.