Fulminant Myocarditis in a Patient with Severe Coronary Artery Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Heart Valve Disease: Mitral and Tricuspid Valves
Heart Valve Disease: Mitral and Tricuspid Valves Heart anatomy The heart has two sides, separated by an inner wall called the septum. The right side of the heart pumps blood to the lungs to pick up oxygen. The left side of the heart receives the oxygen- rich blood from the lungs and pumps it to the body. The heart has four chambers and four valves that regulate blood flow. The upper chambers are called the left and right atria, and the lower chambers are called the left and right ventricles. The mitral valve is located on the left side of the heart, between the left atrium and the left ventricle. This valve has two leaflets that allow blood to flow from the lungs to the heart. The tricuspid valve is located on the right side of the heart, between the right atrium and the right ventricle. This valve has three leaflets and its function is to Cardiac Surgery-MATRIx Program -1- prevent blood from leaking back into the right atrium. What is heart valve disease? In heart valve disease, one or more of the valves in your heart does not open or close properly. Heart valve problems may include: • Regurgitation (also called insufficiency)- In this condition, the valve leaflets don't close properly, causing blood to leak backward in your heart. • Stenosis- In valve stenosis, your valve leaflets become thick or stiff, and do not open wide enough. This reduces blood flow through the valve. Blausen.com staff-Own work, CC BY 3.0 Mitral valve disease The most common problems affecting the mitral valve are the inability for the valve to completely open (stenosis) or close (regurgitation). -

Coronary Artery Disease
Coronary Artery Disease INFORMATION GUIDE Other names: Atherosclerosis CAD Coronary heart disease (CHD) Hardening of the arteries Heart disease Ischemic (is-KE-mik) heart disease Narrowing of the arteries The purpose of this guide is to help patients and families find sources of information and support. This list is not meant to be comprehensive, but rather to provide starting points for information seeking. The resources may be obtained at the Mardigian Wellness Resource Center located off the Atrium on Floor 2 of the Cardiovascular Center. Visit our website at http://www.umcvc.org/mardigian-wellness-resource-center and online Information guides at http://infoguides.med.umich.edu/home Books, Brochures, Fact Sheets Michigan Medicine. What is Ischemic Heart Disease and Stroke. http://www.med.umich.edu/1libr/CCG/IHDshort.pdf National Heart, Lung and Blood Institute (NHLBI). In Brief: Your Guide to Living Well with Heart Disease. A four-page fact sheet. Available online at: http://www.nhlbi.nih.gov/health/public/heart/other/your_guide/living_hd_f s.pdf National Heart, Lung and Blood Institute (NHLBI). Your Guide to Living Well with Heart Disease. A 68-page booklet is a step-by-step guide to helping people with heart disease make decisions that will protect and improve their lives A printer- friendly version is available at: http://www.nhlbi.nih.gov/health/public/heart/other/your_guide/living_well. pdf Coronary Artery Disease Page 1 Mardigian Wellness Resource Center Coronary Artery Disease INFORMATION GUIDE Books Bale, Bradley. Beat the Heart Attack Gene: A Revolutionary Plan to Prevent Heart Disease, Stroke and Diabetes. New York, NY: Turner Publishing, 2014. -

Association of Cardiomegaly with Coronary Artery Histopathology and Its Relationship to Atheroma
32 Journal of Atherosclerosis and Thrombosis Vol.18, No.1 Coronary Histopathology in Cardiomegaly 33 Original Article Association of Cardiomegaly with Coronary Artery Histopathology and its Relationship to Atheroma Richard Everett Tracy Department of Pathology, Louisiana State University Health Sciences Center, New Orleans, USA Aims: Hypertrophied hearts at autopsy often display excessive coronary artery atherosclerosis, but the histopathology of coronary arteries in hearts with and without cardiomegaly has rarely been com- pared. Methods: In this study, forensic autopsies provided hearts with unexplained enlargement plus com- parison specimens. Right coronary artery was opened longitudinally and flattened for formalin fixa- tion and H&E-stained paraffin sections were cut perpendicular to the endothelial surface. The mi- croscopically observed presence or absence of a necrotic atheroma in the specimen was recorded. At multiple sites far removed from any form of atherosclerosis, measurements were taken of intimal thickness, numbers of smooth muscle cells (SMC) and their ratio, the thickness per SMC, averaged over the entire nonatheromatous arterial length. When the mean thickness per SMC exceeded a cer- tain cutoff point, the artery was declared likely to contain a necrotic atheroma. Results: The prevalence of specimens with necrotic atheromas increased stepwise with increasing heart weight, equally with fatal or with incidental cardiomegaly, and equally with hypertension- or obesity-related hypertrophy, rejecting further inclusion of appreciable age, race, or gender effects. The prevalence of specimens with thickness per SMC exceeding the cutoff point was almost always nearly identical to the prevalence of observed necrotic atheroma, showing the two variables to be tightly linked to each other with quantitative consistency across group comparisons of every form. -
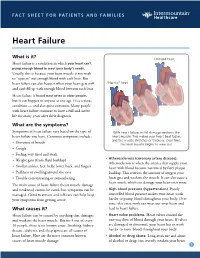
Heart Failure
FACT SHEET FOR PATIENTS AND FAMILIES Heart Failure What is it? Enlarged heart Heart failure is a condition in which your heart can’t pump enough blood to meet your body’s needs. Usually, this is because your heart muscle is too weak to “squeeze” out enough blood with each beat. But heart failure can also happen when your heart gets stiff “Normal” heart and can’t fill up with enough blood between each beat. Heart failure is found most often in older people, but it can happen to anyone at any age. It’s a serious condition — and also quite common. Many people with heart failure continue to have a full and active life for many years after their diagnosis. What are the symptoms? Symptoms of heart failure vary based on the type of With heart failure, initial damage weakens the heart failure you have. Common symptoms include: heart muscle. This makes your heart beat faster, and the muscle stretches or thickens. Over time, • Shortness of breath the heart muscle begins to wear out. • Cough • Feeling very tired and weak • Atherosclerosis (coronary artery disease). • Weight gain (from fluid buildup) Atherosclerosis is when the arteries that supply your • Swollen ankles, feet, belly, lower back, and fingers heart with blood become narrowed by fatty plaque • Puffiness or swelling around the eyes buildup. This restricts the amount of oxygen your • Trouble concentrating or remembering heart gets and weakens the muscle. It can also cause a heart attack, which can damage your heart even more. The main cause of heart failure (heart muscle damage and weakness) cannot be cured, but symptoms can be • High blood pressure (hypertension). -

KNOW the FACTS ABOUT Heart Disease
KNOW THE FACTS ABOUT Heart Disease What is heart disease? Having high cholesterol, high blood pressure, or diabetes also can increase Heart disease is the leading cause of your risk for heart disease. Ask your death in the United States. More than doctor about preventing or treating these 600,000 Americans die of heart disease medical conditions. each year. That’s one in every four deaths in this country.1 What are the signs and symptoms? The term “heart disease” refers to several The symptoms vary depending on the types of heart conditions. The most type of heart disease. For many people, common type is coronary artery disease, chest discomfort or a heart attack is the which can cause heart attack. Other first sign. kinds of heart disease may involve the Someone having a heart attack may valves in the heart, or the heart may not experience several symptoms, including: pump well and cause heart failure. Some people are born with heart disease. l Chest pain or discomfort that doesn’t go away after a few minutes. l Pain or discomfort in the jaw, neck, Are you at risk? or back. Anyone, including children, can l Weakness, light-headedness, nausea develop heart disease. It occurs when (feeling sick to your stomach), or a substance called plaque builds up in a cold sweat. your arteries. When this happens, your arteries can narrow over time, reducing l Pain or discomfort in the arms blood flow to the heart. or shoulder. Smoking, eating an unhealthy diet, and l Shortness of breath. not getting enough exercise all increase If you think that you or someone you your risk for having heart disease. -

SIGN 152 • Cardiac Arrhythmias in Coronary Heart Disease
www.healthcareimprovementscotland.org Edinburgh Office | Gyle Square |1 South Gyle Crescent | Edinburgh | EH12 9EB Telephone 0131 623 4300 Fax 0131 623 4299 Glasgow Office | Delta House | 50 West Nile Street | Glasgow | G1 2NP Telephone 0141 225 6999 Fax 0141 248 3776 The Healthcare Environment Inspectorate, the Scottish Health Council, the Scottish Health Technologies Group, the Scottish Intercollegiate Guidelines Network (SIGN) and the Scottish Medicines Consortium are key components of our organisation. SIGN 152 • Cardiac arrhythmias in coronary heart disease A national clinical guideline September 2018 Evidence KEY TO EVIDENCE STATEMENTS AND RECOMMENDATIONS LEVELS OF EVIDENCE 1++ High-quality meta-analyses, systematic reviews of RCTs, or RCTs with a very low risk of bias 1+ Well-conducted meta-analyses, systematic reviews, or RCTs with a low risk of bias 1 - Meta-analyses, systematic reviews, or RCTs with a high risk of bias High-quality systematic reviews of case-control or cohort studies ++ 2 High-quality case-control or cohort studies with a very low risk of confounding or bias and a high probability that the relationship is causal Well-conducted case-control or cohort studies with a low risk of confounding or bias and a moderate probability that the 2+ relationship is causal 2 - Case-control or cohort studies with a high risk of confounding or bias and a significant risk that the relationship is not causal 3 Non-analytic studies, eg case reports, case series 4 Expert opinion RECOMMENDATIONS Some recommendations can be made with more certainty than others. The wording used in the recommendations in this guideline denotes the certainty with which the recommendation is made (the ‘strength’ of the recommendation). -

Coronary Artery Disease Management
HealthPartners Inspire® Special Needs Basic Care Clinical Care Planning and Resource Guide CORONARY ARTERY DISEASE MANAGEMENT The following Evidence Base Guideline was used in developing this clinical care guide: National Institute of Health (NIH); American Heart Association (AHA) Documented Health Condition: Coronary Artery Disease, Coronary Heart Disease, Heart Disease What is Coronary Artery Disease? Coronary artery disease (CAD) is a disease in which a waxy substance called plaque builds up inside the coronary arteries. These arteries supply oxygen‐rich blood to your heart muscle. When plaque builds up in the arteries, the condition is called atherosclerosis (ATH‐er‐o‐skler‐O‐sis). The buildup of plaque occurs over many years. Over time, plaque can harden or rupture (break open). Hardened plaque narrows the coronary arteries and reduces the flow of oxygen‐rich blood to the heart. If the plaque ruptures, a blood clot can form on its surface. A large blood clot can mostly or completely block blood flow through a coronary artery. Over time, ruptured plaque also hardens and narrows the coronary arteries. Common Causes of Coronary Artery Disease? If the flow of oxygen‐rich blood to your heart muscle is reduced or blocked, angina or a heart attack can occur. Angina is chest pain or discomfort. It may feel like pressure or squeezing in your chest. The pain also can occur in your shoulders, arms, neck, jaw, or back. Angina pain may even feel like indigestion. A heart attack occurs if the flow of oxygen‐rich blood to a section of heart muscle is cut off. If blood flow isn’t restored quickly, the section of heart muscle begins to die. -

Cardiovascular Disease: a Costly Burden for America. Projections
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA PROJECTIONS THROUGH 2035 CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035 american heart association CVD Burden Report CVD Burden association heart american table of contents INTRODUCTION ...................................................................................5 ABOUT THIS STUDY ................................................................................................... 6 WHAT IS CVD? ......................................................................................................... 6 Atrial Fibrillation Congestive Heart Failure Coronary Heart Disease High Blood Pressure Stroke PROJECTIONS: PREVALENCE OF CVD .............................................................7 Latest Projections Age, Race, Sex – Differences That Matter PROJECTIONS: COSTS OF CVD ................................................................. 8-11 The Cost Generators: Aging Baby Boomers Medical Costs Breakdown Direct Costs + Indirect Costs RECOMMENDATIONS .............................................................................13-14 Research Prevention Affordable Health Care 3 CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035 american heart association CVD Burden Report CVD Burden association heart american Introduction Cardiovascular disease (CVD) has been the leading killer In addition, CVD has become our nation’s costliest chronic of Americans for decades. In years past, a heart attack disease. In 2014, stroke and heart -

Coronary Artery Disease
Coronary Artery Disease Your heart is a muscle — a very important muscle that your entire body depends on. As with all muscles, the heart is dependent on blood supply to provide necessary nutrients, fuel and oxygen. The heart gets its blood supply from the coronary arteries. The coronary arteries surround the heart. When the coronary arteries become blocked, narrowed or completely obstructed, the heart cannot get the nutrients, fuel and oxygen it needs. This can cause the heart to become weak or stop altogether or cause a heart attack. This blockage, narrowing or obstruction is known as coronary artery disease (CAD). Who Gets Coronary Artery Disease? Worldwide, coronary artery disease is responsible for over one-third of deaths in adults over age 35! Coronary artery disease is also the number one killer in the United States. For persons aged 40 years, the lifetime risk of developing coronary artery disease is 49 percent in men and 32 percent in women. For those reaching age 70 years, the lifetime risk is 35 percent in men and 24 percent in women. For total coronary events, the incidence rises steeply with age, with women lagging behind men by 10 years. A variety of other factors can increase risk of developing coronary aretery disease including: • Excess fats and cholesterol in the blood • High blood pressure • Excess sugar in the blood (high blood glucose, often due to diabetes) • Early onset of coronary disease in the family history • Sedentary lifestyle (sitting a lot) • Poor diet (higher in processed foods, animal-based proteins and fats) What are the Symptoms? Coronary artery disease (CAD) makes it more difficult for oxygen-rich blood to move through arteries supplying the heart. -

Acute Coronary Syndrome: Diagnostic Evaluation CRAIG BARSTOW, MD, and MATTHEW RICE, MD, Womack Army Medical Center, Fort Bragg, North Carolina JONATHAN D
Acute Coronary Syndrome: Diagnostic Evaluation CRAIG BARSTOW, MD, and MATTHEW RICE, MD, Womack Army Medical Center, Fort Bragg, North Carolina JONATHAN D. McDIVITT, MD, Naval Hospital, Jacksonville, Florida Myocardial infarction (MI), a subset of acute coronary syndrome, is damage to the cardiac muscle as evidenced by elevated cardiac troponin levels in the setting of acute ischemia. Coronary artery disease is the leading cause of mor- tality in the United States. Chest pain is a common presentation in patients with MI; however, there are multiple non- cardiac causes of chest pain, and the diagnosis cannot always be made based on initial presentation. The assessment of a possible MI includes evaluation of risk factors and presenting signs and symptoms, rapid electrocardiography, and serum cardiac troponin measurements. A validated risk score, such as the Thrombolysis in Myocardial Infarction score, may also be useful. Electrocardiography should be performed within 10 minutes of presentation. ST elevation MI is diagnosed with ST segment elevation in two contiguous leads on electrocardiography. In the absence of ST seg- ment elevation, non–ST elevation ACS can be diagnosed. An elevated cardiac troponin level is required for diagnosis, and an increase or decrease of at least 20% is consistent with MI. In some patients with negative electrocardiography findings and normal cardiac biomarkers, additional testing may further reduce the likelihood of coronary artery dis- ease. Cardiac catheterization is the standard method for diagnosing coronary artery disease, but exercise treadmill testing, a stress myocardial perfusion study, stress echocardiography, and computed tomography are noninvasive alternatives. (Am Fam Physician. 2017;95(3):170-177. -

Angina Symptoms Describe Angina As Feeling Like a Vise Is Squeezing Their Chest Or Feeling Like a Heavy Weight Has Been Placed on Their Chest
Diseases and Conditions Angina By Mayo Clinic Staff Angina is a term used for chest pain caused by reduced blood flow to the heart muscle. Angina (an-JIE-nuh or AN-juh-nuh) is a symptom of coronary artery disease. Angina is typically described as squeezing, pressure, heaviness, tightness or pain in your chest. Angina, also called angina pectoris, can be a recurring problem or a sudden, acute health concern. Angina is relatively common but can be hard to distinguish from other types of chest pain, such as the pain or discomfort of indigestion. If you have unexplained chest pain, seek medical attention right away. Symptoms associated with angina include: Chest pain or discomfort Pain in your arms, neck, jaw, shoulder or back accompanying chest pain Nausea Fatigue Shortness of breath Sweating Dizziness The chest pain and discomfort common with angina may be described as pressure, squeezing, fullness or pain in the center of your chest. Some people with angina symptoms describe angina as feeling like a vise is squeezing their chest or feeling like a heavy weight has been placed on their chest. For others, it may feel like indigestion. The severity, duration and type of angina can vary. It's important to recognize if you have new or changing chest discomfort. New or different symptoms may signal a more dangerous form of angina (unstable angina) or a heart attack. Stable angina is the most common form of angina, and it typically occurs with exertion and goes away with rest. If chest discomfort is a new symptom for you, it's important to see your doctor to find out what's causing your chest pain and to get proper treatment. -

Coronary Artery Disease
Building Healthier Communities Coronary Artery Disease Who is at Risk? Risk factors for coronary artery disease fall into two treatment of high cholesterol as an effective strategy groups –modifiable (risk factors one can modify and in the prevention and treatment of coronary artery control) and nonmodifiable (risk factors one cannot disease –even for adolescents and young adults. control). Nonmodifiable risk factors include a per- son’s age, gender, and family history. Hypertension (high blood pressure). As we age, our arteries naturally get stiffer. Thus, hypertension Older age. Of all known risk factors, older age is the often develops after the age of 50, even among those most potent risk factor for coronary artery disease, with good exercise and nutritional habits. Women de- since the arteries of older adults have been exposed to velop hypertension with aging but about a decade the other risk factors (e.g., high cholesterol, hyperten- later than men. Interestingly, up to 70 percent of 70- sion, and smoking) for a longer period of time. Fur- year olds and 80 percent of 80-year olds have high ther, the incidence of hypertension and diabetes, two blood pressure. The type of hypertension that devel- common late-life conditions among people in the ops in older age is different from hypertension that United States, increases dramatically among older age develops at younger ages and is far more risky. Treat- groups and may further accelerate the worsening of ing hypertension associated with aging markedly re- coronary artery disease. In addition, older adults are duces the risk of coronary artery disease, heart failure, more vulnerable to heart disease and regularly have heart attacks, and other diseases (stroke, kidney dis- more complications and worse outcomes as com- ease, and dementia).