Coronary Artery Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Distance Learning Program Anatomy of the Human Heart/Pig Heart Dissection Middle School/ High School
Distance Learning Program Anatomy of the Human Heart/Pig Heart Dissection Middle School/ High School This guide is for middle and high school students participating in AIMS Anatomy of the Human Heart and Pig Heart Dissections. Programs will be presented by an AIMS Anatomy Specialist. In this activity students will become more familiar with the anatomical structures of the human heart by observing, studying, and examining human specimens. The primary focus is on the anatomy and flow of blood through the heart. Those students participating in Pig Heart Dissections will have the opportunity to dissect and compare anatomical structures. At the end of this document, you will find anatomical diagrams, vocabulary review, and pre/post tests for your students. National Science Education (NSES) Content Standards for grades 9-12 • Content Standard:K-12 Unifying Concepts and Processes :Systems order and organization; Evidence, models and explanation; Form and function • Content Standard F, Science in Personal and Social Perspectives: Personal and community health • Content Standard C, Life Science: Matter, energy and organization of living systems • Content Standard A Science as Inquiry National Science Education (NSES) Content Standards for grades 5-8 • Content Standard A Science as Inquiry • Content Standard C, Life Science: Structure and function in living systems; Diversity and adaptations of organisms • Content Standard F, Science in Personal and Social Perspectives: Personal Health Show Me Standards (Science and Health/Physical Education) • Science 3. Characteristics and interactions of living organisms • Health/Physical Education 1. Structures of, functions of and relationships among human body systems Objectives: The student will be able to: 1. -

Blood Vessels
BLOOD VESSELS Blood vessels are how blood travels through the body. Whole blood is a fluid made up of red blood cells (erythrocytes), white blood cells (leukocytes), platelets (thrombocytes), and plasma. It supplies the body with oxygen. SUPERIOR AORTA (AORTIC ARCH) VEINS & VENA CAVA ARTERIES There are two basic types of blood vessels: veins and arteries. Veins carry blood back to the heart and arteries carry blood from the heart out to the rest of the body. Factoid! The smallest blood vessel is five micrometers wide. To put into perspective how small that is, a strand of hair is 17 micrometers wide! 2 BASIC (ARTERY) BLOOD VESSEL TUNICA EXTERNA TUNICA MEDIA (ELASTIC MEMBRANE) STRUCTURE TUNICA MEDIA (SMOOTH MUSCLE) Blood vessels have walls composed of TUNICA INTIMA three layers. (SUBENDOTHELIAL LAYER) The tunica externa is the outermost layer, primarily composed of stretchy collagen fibers. It also contains nerves. The tunica media is the middle layer. It contains smooth muscle and elastic fiber. TUNICA INTIMA (ELASTIC The tunica intima is the innermost layer. MEMBRANE) It contains endothelial cells, which TUNICA INTIMA manage substances passing in and out (ENDOTHELIUM) of the bloodstream. 3 VEINS Blood carries CO2 and waste into venules (super tiny veins). The venules empty into larger veins and these eventually empty into the heart. The walls of veins are not as thick as those of arteries. Some veins have flaps of tissue called valves in order to prevent backflow. Factoid! Valves are found mainly in veins of the limbs where gravity and blood pressure VALVE combine to make venous return more 4 difficult. -

Heart Valve Disease: Mitral and Tricuspid Valves
Heart Valve Disease: Mitral and Tricuspid Valves Heart anatomy The heart has two sides, separated by an inner wall called the septum. The right side of the heart pumps blood to the lungs to pick up oxygen. The left side of the heart receives the oxygen- rich blood from the lungs and pumps it to the body. The heart has four chambers and four valves that regulate blood flow. The upper chambers are called the left and right atria, and the lower chambers are called the left and right ventricles. The mitral valve is located on the left side of the heart, between the left atrium and the left ventricle. This valve has two leaflets that allow blood to flow from the lungs to the heart. The tricuspid valve is located on the right side of the heart, between the right atrium and the right ventricle. This valve has three leaflets and its function is to Cardiac Surgery-MATRIx Program -1- prevent blood from leaking back into the right atrium. What is heart valve disease? In heart valve disease, one or more of the valves in your heart does not open or close properly. Heart valve problems may include: • Regurgitation (also called insufficiency)- In this condition, the valve leaflets don't close properly, causing blood to leak backward in your heart. • Stenosis- In valve stenosis, your valve leaflets become thick or stiff, and do not open wide enough. This reduces blood flow through the valve. Blausen.com staff-Own work, CC BY 3.0 Mitral valve disease The most common problems affecting the mitral valve are the inability for the valve to completely open (stenosis) or close (regurgitation). -

Coronary Artery Disease
Coronary Artery Disease INFORMATION GUIDE Other names: Atherosclerosis CAD Coronary heart disease (CHD) Hardening of the arteries Heart disease Ischemic (is-KE-mik) heart disease Narrowing of the arteries The purpose of this guide is to help patients and families find sources of information and support. This list is not meant to be comprehensive, but rather to provide starting points for information seeking. The resources may be obtained at the Mardigian Wellness Resource Center located off the Atrium on Floor 2 of the Cardiovascular Center. Visit our website at http://www.umcvc.org/mardigian-wellness-resource-center and online Information guides at http://infoguides.med.umich.edu/home Books, Brochures, Fact Sheets Michigan Medicine. What is Ischemic Heart Disease and Stroke. http://www.med.umich.edu/1libr/CCG/IHDshort.pdf National Heart, Lung and Blood Institute (NHLBI). In Brief: Your Guide to Living Well with Heart Disease. A four-page fact sheet. Available online at: http://www.nhlbi.nih.gov/health/public/heart/other/your_guide/living_hd_f s.pdf National Heart, Lung and Blood Institute (NHLBI). Your Guide to Living Well with Heart Disease. A 68-page booklet is a step-by-step guide to helping people with heart disease make decisions that will protect and improve their lives A printer- friendly version is available at: http://www.nhlbi.nih.gov/health/public/heart/other/your_guide/living_well. pdf Coronary Artery Disease Page 1 Mardigian Wellness Resource Center Coronary Artery Disease INFORMATION GUIDE Books Bale, Bradley. Beat the Heart Attack Gene: A Revolutionary Plan to Prevent Heart Disease, Stroke and Diabetes. New York, NY: Turner Publishing, 2014. -

Association of Cardiomegaly with Coronary Artery Histopathology and Its Relationship to Atheroma
32 Journal of Atherosclerosis and Thrombosis Vol.18, No.1 Coronary Histopathology in Cardiomegaly 33 Original Article Association of Cardiomegaly with Coronary Artery Histopathology and its Relationship to Atheroma Richard Everett Tracy Department of Pathology, Louisiana State University Health Sciences Center, New Orleans, USA Aims: Hypertrophied hearts at autopsy often display excessive coronary artery atherosclerosis, but the histopathology of coronary arteries in hearts with and without cardiomegaly has rarely been com- pared. Methods: In this study, forensic autopsies provided hearts with unexplained enlargement plus com- parison specimens. Right coronary artery was opened longitudinally and flattened for formalin fixa- tion and H&E-stained paraffin sections were cut perpendicular to the endothelial surface. The mi- croscopically observed presence or absence of a necrotic atheroma in the specimen was recorded. At multiple sites far removed from any form of atherosclerosis, measurements were taken of intimal thickness, numbers of smooth muscle cells (SMC) and their ratio, the thickness per SMC, averaged over the entire nonatheromatous arterial length. When the mean thickness per SMC exceeded a cer- tain cutoff point, the artery was declared likely to contain a necrotic atheroma. Results: The prevalence of specimens with necrotic atheromas increased stepwise with increasing heart weight, equally with fatal or with incidental cardiomegaly, and equally with hypertension- or obesity-related hypertrophy, rejecting further inclusion of appreciable age, race, or gender effects. The prevalence of specimens with thickness per SMC exceeding the cutoff point was almost always nearly identical to the prevalence of observed necrotic atheroma, showing the two variables to be tightly linked to each other with quantitative consistency across group comparisons of every form. -
Heart Failure
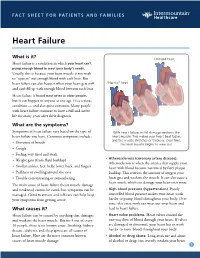
FACT SHEET FOR PATIENTS AND FAMILIES Heart Failure What is it? Enlarged heart Heart failure is a condition in which your heart can’t pump enough blood to meet your body’s needs. Usually, this is because your heart muscle is too weak to “squeeze” out enough blood with each beat. But heart failure can also happen when your heart gets stiff “Normal” heart and can’t fill up with enough blood between each beat. Heart failure is found most often in older people, but it can happen to anyone at any age. It’s a serious condition — and also quite common. Many people with heart failure continue to have a full and active life for many years after their diagnosis. What are the symptoms? Symptoms of heart failure vary based on the type of With heart failure, initial damage weakens the heart failure you have. Common symptoms include: heart muscle. This makes your heart beat faster, and the muscle stretches or thickens. Over time, • Shortness of breath the heart muscle begins to wear out. • Cough • Feeling very tired and weak • Atherosclerosis (coronary artery disease). • Weight gain (from fluid buildup) Atherosclerosis is when the arteries that supply your • Swollen ankles, feet, belly, lower back, and fingers heart with blood become narrowed by fatty plaque • Puffiness or swelling around the eyes buildup. This restricts the amount of oxygen your • Trouble concentrating or remembering heart gets and weakens the muscle. It can also cause a heart attack, which can damage your heart even more. The main cause of heart failure (heart muscle damage and weakness) cannot be cured, but symptoms can be • High blood pressure (hypertension). -

Cardiology Self Learning Package
Cardiology Self Learning Package Module 1: Anatomy and Physiology of the Module 1: Anatomy and Physiology of the Heart Heart. Page 1 Developed by Tony Curran (Clinical Nurse Educator) and Gill Sheppard (Clinical Nurse Specialist) Cardiology (October 2011) CONTENT Introduction…………………………………………………………………………………Page 3 How to use the ECG Self Learning package………………………………………….Page 4 Overview of the Heart…………………………………………………...…………..…….Page 5 Location, Size and Shape of the Heart…………………………………………………Page 5 The Chambers of the Heart…………….………………………………………..……….Page 7 The Circulation System……………………………………….………………..…………Page 8 The Heart Valve Anatomy………………………….…………………………..…………Page 9 Coronary Arteries…………………………………………….……………………..……Page 10 Coronary Veins…………………………………………………………………..……….Page 11 Cardiac Muscle Tissue……………………………………………………………..……Page 12 The Conduction System………………………………………………………………...Page 13 Cardiac Cycle……………………………………………………………………………..Page 15 References…………………………………………………………………………………Page 18 Module Questions………………………………………………………………………..Page 19 Module Evaluation Form………………………………………………………………..Page 22 [Module 1: Anatomy and Physiology of the Heart Page 2 Developed by Tony Curran (Clinical Nurse Educator) and Gill Sheppard (Clinical Nurse Specialist) Cardiology (October 2011) INTRODUCTION Welcome to Module 1: Anatomy and Physiology of the Heart. This self leaning package is designed to as tool to assist nurse in understanding the hearts structure and how the heart works. The goal of this module is to review: Location , size and shape of the heart The chambers of the heart The circulation system of the heart The heart’s valve anatomy Coronary arteries and veins Cardiac muscle tissue The conduction system The cardiac cycle This module will form the foundation of your cardiac knowledge and enable you to understand workings of the heart that will assist you in completing other modules. Learning outcomes form this module are: To state the position of the heart, the size and shape. -

KNOW the FACTS ABOUT Heart Disease
KNOW THE FACTS ABOUT Heart Disease What is heart disease? Having high cholesterol, high blood pressure, or diabetes also can increase Heart disease is the leading cause of your risk for heart disease. Ask your death in the United States. More than doctor about preventing or treating these 600,000 Americans die of heart disease medical conditions. each year. That’s one in every four deaths in this country.1 What are the signs and symptoms? The term “heart disease” refers to several The symptoms vary depending on the types of heart conditions. The most type of heart disease. For many people, common type is coronary artery disease, chest discomfort or a heart attack is the which can cause heart attack. Other first sign. kinds of heart disease may involve the Someone having a heart attack may valves in the heart, or the heart may not experience several symptoms, including: pump well and cause heart failure. Some people are born with heart disease. l Chest pain or discomfort that doesn’t go away after a few minutes. l Pain or discomfort in the jaw, neck, Are you at risk? or back. Anyone, including children, can l Weakness, light-headedness, nausea develop heart disease. It occurs when (feeling sick to your stomach), or a substance called plaque builds up in a cold sweat. your arteries. When this happens, your arteries can narrow over time, reducing l Pain or discomfort in the arms blood flow to the heart. or shoulder. Smoking, eating an unhealthy diet, and l Shortness of breath. not getting enough exercise all increase If you think that you or someone you your risk for having heart disease. -

SIGN 152 • Cardiac Arrhythmias in Coronary Heart Disease
www.healthcareimprovementscotland.org Edinburgh Office | Gyle Square |1 South Gyle Crescent | Edinburgh | EH12 9EB Telephone 0131 623 4300 Fax 0131 623 4299 Glasgow Office | Delta House | 50 West Nile Street | Glasgow | G1 2NP Telephone 0141 225 6999 Fax 0141 248 3776 The Healthcare Environment Inspectorate, the Scottish Health Council, the Scottish Health Technologies Group, the Scottish Intercollegiate Guidelines Network (SIGN) and the Scottish Medicines Consortium are key components of our organisation. SIGN 152 • Cardiac arrhythmias in coronary heart disease A national clinical guideline September 2018 Evidence KEY TO EVIDENCE STATEMENTS AND RECOMMENDATIONS LEVELS OF EVIDENCE 1++ High-quality meta-analyses, systematic reviews of RCTs, or RCTs with a very low risk of bias 1+ Well-conducted meta-analyses, systematic reviews, or RCTs with a low risk of bias 1 - Meta-analyses, systematic reviews, or RCTs with a high risk of bias High-quality systematic reviews of case-control or cohort studies ++ 2 High-quality case-control or cohort studies with a very low risk of confounding or bias and a high probability that the relationship is causal Well-conducted case-control or cohort studies with a low risk of confounding or bias and a moderate probability that the 2+ relationship is causal 2 - Case-control or cohort studies with a high risk of confounding or bias and a significant risk that the relationship is not causal 3 Non-analytic studies, eg case reports, case series 4 Expert opinion RECOMMENDATIONS Some recommendations can be made with more certainty than others. The wording used in the recommendations in this guideline denotes the certainty with which the recommendation is made (the ‘strength’ of the recommendation). -

Coronary Artery Disease Management
HealthPartners Inspire® Special Needs Basic Care Clinical Care Planning and Resource Guide CORONARY ARTERY DISEASE MANAGEMENT The following Evidence Base Guideline was used in developing this clinical care guide: National Institute of Health (NIH); American Heart Association (AHA) Documented Health Condition: Coronary Artery Disease, Coronary Heart Disease, Heart Disease What is Coronary Artery Disease? Coronary artery disease (CAD) is a disease in which a waxy substance called plaque builds up inside the coronary arteries. These arteries supply oxygen‐rich blood to your heart muscle. When plaque builds up in the arteries, the condition is called atherosclerosis (ATH‐er‐o‐skler‐O‐sis). The buildup of plaque occurs over many years. Over time, plaque can harden or rupture (break open). Hardened plaque narrows the coronary arteries and reduces the flow of oxygen‐rich blood to the heart. If the plaque ruptures, a blood clot can form on its surface. A large blood clot can mostly or completely block blood flow through a coronary artery. Over time, ruptured plaque also hardens and narrows the coronary arteries. Common Causes of Coronary Artery Disease? If the flow of oxygen‐rich blood to your heart muscle is reduced or blocked, angina or a heart attack can occur. Angina is chest pain or discomfort. It may feel like pressure or squeezing in your chest. The pain also can occur in your shoulders, arms, neck, jaw, or back. Angina pain may even feel like indigestion. A heart attack occurs if the flow of oxygen‐rich blood to a section of heart muscle is cut off. If blood flow isn’t restored quickly, the section of heart muscle begins to die. -

Cardiovascular Disease: a Costly Burden for America. Projections
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA PROJECTIONS THROUGH 2035 CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035 american heart association CVD Burden Report CVD Burden association heart american table of contents INTRODUCTION ...................................................................................5 ABOUT THIS STUDY ................................................................................................... 6 WHAT IS CVD? ......................................................................................................... 6 Atrial Fibrillation Congestive Heart Failure Coronary Heart Disease High Blood Pressure Stroke PROJECTIONS: PREVALENCE OF CVD .............................................................7 Latest Projections Age, Race, Sex – Differences That Matter PROJECTIONS: COSTS OF CVD ................................................................. 8-11 The Cost Generators: Aging Baby Boomers Medical Costs Breakdown Direct Costs + Indirect Costs RECOMMENDATIONS .............................................................................13-14 Research Prevention Affordable Health Care 3 CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035 american heart association CVD Burden Report CVD Burden association heart american Introduction Cardiovascular disease (CVD) has been the leading killer In addition, CVD has become our nation’s costliest chronic of Americans for decades. In years past, a heart attack disease. In 2014, stroke and heart -

Fulminant Myocarditis in a Patient with Severe Coronary Artery Disease
Journal of Cardiology Cases 9 (2014) 15–17 Contents lists available at www.sciencedirect.com Journal of Cardiology Cases journa l homepage: www.elsevier.com/locate/jccase Case Report Fulminant myocarditis in a patient with severe coronary artery disease a a,∗ b Satoshi Fujita (MD) , Ryuji Okamoto (MD, FJCC) , Takeshi Takamura (MD) , a a a Hiroshi Nakajima (MD) , Masaki Tanabe (MD) , Shiro Nakamori (MD) , c a a Kaoru Dohi (MD, FJCC) , Takashi Tanigawa (MD, FJCC) , Mashio Nakamura (MD, FJCC) , a Masaaki Ito (MD, FJCC) a Department of Cardiology and Nephrology, Mie University Graduate School of Medicine, 2-174 Edobashi, Tsu, Mie 514-8507, Japan b Department of Cardiology, Ise Red Cross Hospital, Ise, Japan c Department of Laboratory Medicine, Mie University Graduate School of Medicine, Tsu, Japan a r a t i c l e i n f o b s t r a c t Article history: A 55-year-old man complaining of fever and exertional dyspnea was admitted for coronary angiography Received 4 December 2012 to differentiate between fulminant myocarditis and acute coronary syndrome. He had been treated for Received in revised form 20 June 2013 17 years for angina pectoris. His electrocardiogram demonstrated ST segment changes in almost all leads. Accepted 21 August 2013 Cardiac catheterization demonstrated severe stenosis in the left descending artery, the diagonal branch, and the right coronary artery. Ultrasonography, however, revealed diffuse hypokinesis of the left ven- Keywords: tricle and edematous wall thickening, suggesting fulminant myocarditis. This is the first report in which Fulminant myocarditis a patient with fulminant myocarditis with severe coronary artery disease was successfully treated with Coronary artery disease mechanical cardiopulmonary support, intensive pharmacological therapy, and staged coronary interven- Differential diagnosis tion procedures.