Looking Back
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List of Abbreviations
LIST OF ABBREVIATIONS S. No. 1. A&N Andaman & Nicobar 2. ACO Assistant Committee Officer 3. AEES Atomic Energy Education Society 4. AeBAS Aadhaar enabled Biometric Attendance System 5. AIIMS All India Institute of Medical Sciences 6. AIU Association of Indian Universities 7. AMC Annual Maintenance Contract 8. ARO Assistant Research Officer 9. ASEAN Association of South-East Asian Nations 10. ASGP Association of Secretaries-General of Parliaments 11. ASI Archaeological Survey of India 12. ASSOCHAM Associated Chambers of Commerce and Industry of India 13. ATNs Action Taken Notes 14. ATRs Action Taken Reports 15. AWS Automatic Weather Station 16. AYCL Andrew Yule & Company Ltd. 17. AYUSH Ayurvedic, Yoga and Naturopathy, Unani, Siddha and Homeopathy 18. BCD Basic Customs Duty 19. BEML Bharat Earth Movers Limited 20. BHAVINI Bhartiya Nabhikiya Vidyut Nigam Ltd. 21. BHEL Bharat Heavy Electricals Ltd. 22. BHMRC Bhopal Memorial Hospital & Research Centre 23. BIOS Bills Information Online System 24. BIS Bureau of Indian Standards 25. BMRCL Bangalore Metro Rail Corporation Ltd. 26. BOAT Board of Apprentice Ship Training 27. BOB Bank of Baroda 28. BPCL Bharat Petroleum Corporation Limited 29. BPST Bureau of Parliamentary Studies and Training 30. BRO Border Roads Organisation 31. BSF Border Security Force 32. BSNL Bharat Sanchar Nigam Limited 33. C&AG Comptroller & Auditor General 34. CARA Central Adoption Resource Authority 35. CAT Central Administrative Tribunal 36. CBI Central Bureau of Investigation 37. CBRN Chemical Biological Radiological Nuclear 38. CBDT Central Board of Direct Taxes 39. CCL Child Care Leave 40. CCRYN Central Council for Research in Yoga and Naturopathy 41. CCS Central Civil Services 42. -

EPORT 2017 -18 of TATA MEMORIAL CENTRE (A Grant-In-Aid Institute of the Department of Atomic Energy, Government of India)
ANNUAL REPORT 2017 -18 of TATA MEMORIAL CENTRE (A Grant-in-Aid Institute of the Department of Atomic Energy, Government of India) Tata Memorial Hospital, Mumbai. Advanced Centre for Treatment, Research and Education in Cancer, Navi Mumbai. Centre for Cancer Epidemiology, Navi Mumbai. Homi Bhabha Cancer Hospital and Research Centre, Visakhapatnam. Homi Bhabha Cancer Hospital, Sangrur. Homi Bhabha Cancer Hospital and Research Centre, Mohali. Dr. Bhubaneswar Borooah Cancer Institute, Guwahati. Homi Bhabha Cancer Hospital, Varanasi. Mahamana Pandit Madan Mohan Malviya Cancer Centre, Varanasi. Tata Memorial Centre Mission and Vision of the Tata Memorial Centre Mission The Tata Memorial Centre’s mission is to provide comprehensive cancer care to one and all, through its motto of excellence in service, education and research. Vision As the premier cancer centre in the country, we will provide leadership in guiding the national policy and strategy for cancer care by: Promoting outstanding services through evidence based practice of oncology Commitment of imparting education in cancer to students, trainees, professionals, employees and the public and, Emphasis on research that is affordable, innovative and relevant to the needs of the country. Tata Memorial Centre, Annual Report 2017 - 2018 Contents Tata Memorial Centre (TMC) Governing Council ...................................................................................... 9 Messages Director TMC .............................................................................................. -

Institutions Funded by Dae
GOVERNMENT OF INDIA DEPARTMENT OF ATOMIC ENERGY RAJYA SABHA STARRED QUESTION NO. 161 TO BE ANSWERED ON 11.08.2011 INSTITUTIONS FUNDED BY DAE 161 . SHRIMATI RENUBALA PRADHAN: Will the PRIME MINISTER be pleased to state: (a) the details of the institutions funded by the Department of Atomic Energy and the amount of plan and non-plan funds allocated to them so far during the last three years; (b) whether any achievements have been made by each such institution during the last three years; (c) if so, whether such achievements are of international repute; and (d) the details thereof, institution-wise, during the last three years? ANSWER THE MINISTER OF STATE FOR PERSONNEL, PUBLIC GRIEVANCES & PENSIONS AND IN THE PRIME MINISTER’S OFFICE (SHRI V. NARAYANASAMY) (a) to (d) A statement is laid on the Table of the House. ******* STATEMENT REFERRED TO IN REPLY TO RAJYASABHA STARRED QUESTION NO.161 FOR ANSWER ON 11.08.2011 BY SMT. RENUBALA PRADHAN REGARDING INSTITUTIONS FUNDED BY DAE (a) The details are given in Annexure 1; (b) Yes, Sir; (c) Yes, Sir; (d) The details are given in Annexure 2. ******* Annexure-1 The Aided Institutions under DAE are: 1. Tata Institute of Fundamental Research (TIFR), Mumbai 2. Tata Memorial Centre (TMC), Mumbai 3. Saha Institute of Nuclear Physics (SINP), Kolkata 4. Institute of Physics (IoP), Bhubaneswar 5. Institute of Mathematical Sciences (IMSc), Chennai 6. Harish Chandra Research Institute (HRI), Allahabad 7. Institute for Plasma Research (IPR), Gandhinagar 8. National Institute of Science, Education and Research (NISER), Bhubaneswar 9. Atomic Energy Education Society (AEES), Mumbai Details of Grants given to Aided Institutions under DAE for the period 2008-09 to 2011-12 under Plan and Non-Plan (` in crores) Aided Institutions Sr. -

Communication Dated 26 September 2008, Copied to the Agency by the Permanent Mission of India Regarding the Middle
s^llAEA Atoms for Peace Information Circular INFCIRC/731 Date: 25 July 2008 General Distribution Original: English Communication dated 25 July 2008 received from the Permanent Mission of India concerning a document entitled "Implementation of the India-United States Joint Statement of July 18, 2005: India's Separation Plan" The Secretariat has received a communication dated 25 July 2008 from the Permanent Mission of India to the Agency, attaching a document entitled "Implementation of the India-United States Joint Statement of July 18, 2005: India's Separation Plan". As requested by the Permanent Mission of India to the Agency, the communication and its attachment are herewith circulated for information. INFCIRC/731 Attachment $ m-*a *T jarift Tun* Permanent Mission of India to !'>•' International Organisations in Vienna Karnlnoirmg ? ™«**« A.,»W VIENNA No. Vicn/J IO/I7/07 25,h July 2008 I he Permanent Mission of India in Vienna presents its compliments to UlC Director-General of the Inlernalional Atomic Energy Agency (IAFA) and has the honour to enclose a document entitled "Implementation of the India-United Stales Joint Statement of July 18, 2005: India's Separation Plan.". It is the Government of India's intention to move forward in accordance with the provisions of the "Agreement between the Government of India and the International Atomic Energy Agency for the Application of Safeguards to Civilian Nuclear Facilities" reproduced as an attachment to the agenda item GOV/2008'30 dated 9 July 2008. aftci its entry into force. The Permanent Mission of India in Vienna requests the Agency lo distribute this letter along with the enclosed document to all Memhcr-Sialcs of the Agency for information. -
Stamps of India - Commemorative by Prem Pues Kumar [email protected] 9029057890
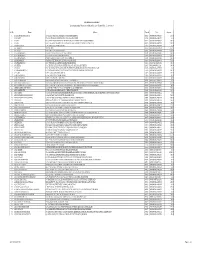
E-Book - 26. Checklist - Stamps of India - Commemorative By Prem Pues Kumar [email protected] 9029057890 For HOBBY PROMOTION E-BOOKS SERIES - 26. FREE DISTRIBUTION ONLY DO NOT ALTER ANY DATA ISBN - 1st Edition Year - 1st May 2020 [email protected] Prem Pues Kumar 9029057890 Page 1 of 76 Nos. YEAR PRICE NAME Mint FDC B. 1 2 3 1947 1 21-Nov-47 31/2a National Flag 2 15-Dec-47 11/2a Ashoka Lion Capital 3 15-Dec-47 12a Aircraft 1948 4 29-May-48 12a Air India International 5 15-Aug-48 11/2a Mahatma Gandhi 6 15-Aug-48 31/2a Mahatma Gandhi 7 15-Aug-48 12a Mahatma Gandhi 8 15-Aug-48 10r Mahatma Gandhi 1949 9 10-Oct-49 9 Pies 75th Anni. of Universal Postal Union 10 10-Oct-49 2a -do- 11 10-Oct-49 31/2a -do- 12 10-Oct-49 12a -do- 1950 13 26-Jan-50 2a Inauguration of Republic of India- Rejoicing crowds 14 26-Jan-50 31/2a Quill, Ink-well & Verse 15 26-Jan-50 4a Corn and plough 16 26-Jan-50 12a Charkha and cloth 1951 17 13-Jan-51 2a Geological Survey of India 18 04-Mar-51 2a First Asian Games 19 04-Mar-51 12a -do- 1952 20 01-Oct-52 9 Pies Saints and poets - Kabir 21 01-Oct-52 1a Saints and poets - Tulsidas 22 01-Oct-52 2a Saints and poets - MiraBai 23 01-Oct-52 4a Saints and poets - Surdas 24 01-Oct-52 41/2a Saints and poets - Mirza Galib 25 01-Oct-52 12a Saints and poets - Rabindranath Tagore 1953 26 16-Apr-53 2a Railway Centenary 27 02-Oct-53 2a Conquest of Everest 28 02-Oct-53 14a -do- 29 01-Nov-53 2a Telegraph Centenary 30 01-Nov-53 12a -do- 1954 31 01-Oct-54 1a Stamp Centenary - Runner, Camel and Bullock Cart 32 01-Oct-54 2a Stamp Centenary -
Format Section
ION EXCHANGE LIMITED List Of Outstanding Warrant as on 15th October, 2016 (Payment Date:- IO 14-09-2016) Sr. No. Name Address Pincode Folio Amount 1 A ANANDA RANJANA DOS 32, THOMAS NAGAR LITTLE MOUNT SAIDAPET MADRAS 600015 0000000000IOA0002323 162.00 2 A G KAISER C/O MOHD ISMAIL HUNDEKAR STATION ROAD YADGIR 585202 0000000000IOA0001776 84.00 3 A GOPAL H 14/3 HOUSING BOARD FLAT SOUTH SIVAN KOIL STREET VADAPALANI CHENNAI 600026 0000000000IOA0002592 300.00 4 A GOPAL H 14/3, HOUSING BOARD FLAT SOUTH SIVAN KOIL STREET VADAPALANI CHENNAI 600026 0000000000IOA0002553 150.00 5 A H SRINIVASAN 1/34 ASHOK NAGAR NEW DELHI 110018 0000000000IOA0001370 3.00 6 A K BHARAT TEST DUMMY 999999 0000000000IOA0011001 375.00 7 A K KHOLI K-16 LAJPAT NAGAR NEW DELHI 110024 0000000000IOA0011160 1,659.00 8 A L SUBRAMANIAN POCKET B-122 MAYUR VIHAR PHASE II DELHI 110091 0000000000IOA0002143 300.00 9 A L SUBRAMANIAN LT 15A DDA FLATS KALKAJI, NEW DELHI 110019 0000000000IOA0010003 282.00 10 A L SUBRAMANIAN B-122 POCKET B MAYUR VIHAR PHASE II N DELHI 110091 0000000000IOA0011124 300.00 11 A MANONMANI 6 RAILWAY FEEDER ROAD SULUR (P O) COIMBATORE 641402 0000000000IOA0000669 546.00 12 A PADMANABHAN 24/16 VEDACHALA GARDEN MANDAVELI CHENNAI 600028 0000IN30108022159972 600.00 13 A R SEETHA 15-1C RENGANATHAPURAM OFFICERS COLONY, ATSHAYA APP TRICHY 620017 00001203840000221028 300.00 14 A RAMAN FLAT NO 5, GROUND FLOOR NAVIN APARTMENT HANUMAN NAGAR, KATEMANDI KALYAN 421306 0000000000IOA0010015 84.00 15 A S CHANDRASHEKAR ION EXCHANGE INDIA LTD 2ND FLR,NEETA TOWERS OPP SANDVIK ,DAPODI -

List of Stamps from 1852 Onwards
LIST OF STAMPS FROM 1852 ONWARDS POSTAGE STAMPS – PRE-INDEPENDENCE Year Denomination Particulars 1 1852 /2a SCINDE DAWK 1 1854 /2a EAST INDIA CO, ISSUES 1a -do- 4a -do- 1854 4a QUEEN VICTORIA 1 /2a -do- 1a -do- 2a -do- 1855 4a -do- 8a -do- 1 1856-64 /2a -do- 1a -do- 2a -do- 4a -do- 8a -do- UNDER THE CROWN - QUEEN 1860 8p VICTORIA 1 1865 /2a Elephant’s Head Watermark 8p -do- 1a -do- 2a -do- 4a -do- 8a -do- 1866 6a -do- 1866-67 4a Octagonal design 6a8p -do- 1868 8a Die II 1 1873 /2a -do- 1874 9p -do- 1r -do- 1876 6a 12a 1 LIST OF STAMPS FROM 1852 ONWARDS 1 1882-88 /2a Empire of India – Queen Victoria 9p -do- 1a -do- 1a6p -do- 2a -do- 3a -do- 4a -do- 4a6p -do- 8a -do- 12a -do- 1R -do- 1 1891 2 /2a Surcharged 1 1892-97 2 /2a 1r 1895 2r 3r 5r 1 1898 /4a 1899 3p 1900-02 3p 1 /2a 1a 2a 1 2 /2a 1902-11 3p KING EDWARD VII 1 /2a -do- 1a -do- 2a -do- 1 2 /2a -do- 3a -do- 4a -do- 6a -do- 8a -do- 12a -do- 1r -do- 2r -do- 2 LIST OF STAMPS FROM 1852 ONWARDS 3r -do- 5r -do- 10r -do- 15r -do- 25r -do- 1 1905 /4a Surcharged 1 1906 /2a Postage and Revenue 1a -do- 1911 3p KING GEORGE V 1 /2a -do- 1a -do- 1 1 /2a -do- 2a -do- 1 2 /2a -do- 3a -do- 4a -do- 6a -do- 8a -do- 12a -do- 1r -do- 2r -do- 5r -do- 10r -do- 15r -do- 25r -do- 1921 9p Surcharged 1 1922 /4a -do- 1922-26 1a Colours changed 1 1 /2a -do- 1 2 /2a -do- 3a -do- 1926-31 3p Printed at ISP Nasik 1 /2a -do- 1a -do- 1 1 /2a -do- 2a -do- 3 LIST OF STAMPS FROM 1852 ONWARDS 1 2 /2a -do- 3a -do- 4a -do- 8a -do- 12a -do- 1r -do- 2r -do- 5r -do- 10r -do- 15r -do- 25r -do- 1929 2a Air Mail Series 3a -do- 4a -

Central Government Publications
March 2007 GOVERNMENT PUBLICATIONS (A) Central Government Publications 000 GENERALITIES 1 Centre for Development of Advanced Computing Annual report 2005-2006 / Centre for Development of Advanced Computing.-- Bangalor e , 200 6. 70+33p.; 28cm. In Hindi also. 004R P5 RC121584,1-4; RC121585,1-3 2 National Informatics Centre Services Inc. Annual report 2005-2006 / National Informatics Centre Services Inc.—- New Delhi, 2006. 48p.; 28cm. Bilingual. 005.16R P5 RC121605 3 Press Council of India Annual report 2005-2006 (27th) / Press Council of India.-- New Delhi, 2007. 137p.; 24cm. In Hindi also. 070.1061R P5 RC121679,1-4; RC121680,1-3 300 SOCIAL SCIENCES 4 National Scheduled Tribes Finance and Development Corporation (NSTFDC) Annual report 2005-2006 (5th) / National Scheduled Tribes Finance and Development Corporation (NSTFDC).-- New Delhi, 2006. 53+53p.; 28cm. Bilingual. 301.43R P5 RC121676,1-5 5 India. Lok Sabha (14th). Committee on Welfare of Scheduled Castes and Scheduled Tribes (2006-2007) Report of the study tour of the Committee on the welfare of scheduled castes and scheduled tribes on their visit to Mumbai, Mangalore, Mercara (COORG), Mysore and Bangalore during July 2006 / Committee on Welfare of Scheduled Castes and Scheduled Tribes (2006-2007), Lok Sabha (14th), India.-- New Delhi: Lok Sabha Secretariat, 2006. 75p.; cycl.; 28cm. In Hindi also. Chairman: Ratilal Kalidas Varma. LC 301.43R P6 RC121689-RC121690,1-5 6 India. Lok Sabha (14th). Committee on the Welfare of Scheduled Castes and Scheduled Tribes (2006-2007) 20th report on reservation for and employment of scheduled castes and scheduled Tribes in All India Institute of Medical Sciences including reservation for SCs and STs in admission therein relating to the Ministry of Health and Family Welfare (Department of Health) (Presented on March 2007) / Committee on the Welfare of Scheduled Castes and Scheduled Tribes (2006-2007), Lok Sabha (14th), India.—- New Delhi: Lok Sabha Secretariat, 2007. -

Notice No 10 Cancellation of AIQ Seat Before Joining State Counseling Seat
om No.SSC/C.R.No. 01 /NEET-PG-2020/Notice No 10/AIQ cancelation/2020 Date: 16/05/2020 NOTICE No.10 NEET-PG-2020 Cancellation of AIQ Seat before Joining State Quota Seat Ref: 1) U-12021/44/2019/25-MEC Dated: 29-04-2020, Notice from MCC. In view of the directions in above mentioned Notice from MCC, it has been noted that the following Candidates are holding a seat in Round-1 of NEET-PG counseling of All India Quota/Deemed University/Central Institutes. Any such Candidate who wish to participate in State Quota Counseling should resign the All India Seat and submit resignation letter before Joining State Quota Seat. Concerned colleges should ensure that the candidate submits resignation letter before Joining. Encl: List of Candidates -Sd- (Sandeep Kadam) lAS Commissioner and Competent Authority State CET CELL, Mumbai NEET (PG) 2020 Round No : 1 List of Candidates Holding AIQ Admission Sr. AIR NAME NEET RollNo Institite Quota Subject AIQ Admission Holding in Institute 1 63 ANKITA RANI 2066102564 G. S. MEDICAL COLLEGE MUMBAI COMMON RADIOLOGY Byramjee Jeejeebhoy Government Medical College, Pune 2 97 BEDRE DIKSHA ABHIMANYU 2066009954 G. S. MEDICAL COLLEGE MUMBAI COMMON MEDICINE Seth Gordhandas Sunderdas MedicalCollege, Mumbai 3 174 KUMBHAR SAURABH SHIVAJI 2066130571 T. N. MEDICAL COLLEGE MUMBAI COMMON MEDICINE Topiwala National Medical College,Mumbai 4 209 SHETTY TANISH ASHOK 2066102508 L. T. MEDICAL COLLEGE MUMBAI COMMON MEDICINE Lokmanya Tilak Municipal MedicalCollege, Mumbai 5 220 APARNA T 2066112039 G. S. MEDICAL COLLEGE MUMBAI COMMON SKIN AND VD Lokmanya Tilak Municipal Medical College, Mumbai 6 256 VETAL DARPAN MAHESH 2066131433 L. -
Compendium of Instructions for COVID-19 Testing Laboratory (First
COMPENDIUM OF INSTRUCTIONS FOR COVID-19 TESTING LABORATORY Medical Education and Drugs Department Government of Maharashtra FIRST EDITION 21 April 2020 Medical Education and Drugs Department COMPENDIUM OF INSTRUCTIONS FOR COVID-19 TESTING LABORATORY FIRST EDITION Editor -in -chief Dr. Sanjay Mukherjee, IAS Secretary Medical Education and Drugs Department Government of Maharashtra Editors Dr. Rajesh Karyakarte, Dr. Sachin Mulkutkar, Professor Professor B.J. Government Medical College, Grant Government Medical College, Pune Mumbai Co-Editors Dr. Rakesh Waghmare, Dr. Mandar Sadawarte, Associate Professor Assistant Professor Grant Government Medical College, Grant Government Medical College, Mumbai Mumbai FOREWORD As you are aware, COVID – 19 is widely spreading across the country, rising beyond 15000 positive cases in the 12th week. In order to manage and contain the spread of COVID – 19 any further, both Centre and State Government and Associated Departments have come out with Guidelines and Instructions for COVID-19 Testing to be adopted across the country and in each state. This Compendium is a compilation of instructions & guidelines for operating a Covid-19 Testing Laboratory issued by Ministry of Health & Family Welfare, Indian Council of Medical Research, Government of India and instructions issued by Medical Education and Drugs Department, Government of Maharashtra. We hope that this compilation helps Laboratory In-charges, Administrators and all people involved in Testing of COVID – 19 cases. The first edition is updated with the information issued till 21st April, 2020. The Editorial Board shall be updating this on a regular basis. We thank you all. INDEX S. N. SECTION TITLE WEBLINK PAGE A Testing 1. DMER SOP for Operating 1-5 - Strategy & Covid 19 Testing Laboratory Guidelines 2. -

THURSDAY, the 21ST MARCH, 2002 (The Rajya Sabha Met in the Parliament House at 11-00 A.M.) 11-00 A.M
THURSDAY, THE 21ST MARCH, 2002 (The Rajya Sabha met in the Parliament House at 11-00 a.m.) 11-00 a.m. 1. Obituary Reference The Chairman made a reference to the passing away of Shri Bhagwan Din (ex- Member). The House observed silence, all Members standing, as a mark of respect to the memory of the departed. 11-02 a.m. 2. Starred Questions The following Starred Questions were orally answered:- Starred Question No. 262 regarding Prime Minister’s Japan visit. RAJYA SABHA Starred Question No. 263 regarding Amendment to Industrial Disputes Act, 1947. Starred Question 264 regarding Ban on duplicate brands of goods. Answers to remaining Starred Question Nos. 261, 265 to 280 were laid on the Table. Answers to Starred Question Nos.241 to 260 put down in the List of March 20, 2002 were also laid on the Table. 3. Unstarred Questions Answers to Unstarred Question Nos.1903 to 2057 were laid on the Table. Answers to Unstarred Question Nos.1784 to 1902 put down in the List of March 20, 2002 were also laid on the Table. 12 Noon 4. Proclamation under Article 356 of the Constitution Shri L.K. Advani (Minister of Home Affairs) laid on the Table a copy each (in English and Hindi) of the following papers:— (i) Proclamation [G.S.R. No.168 (E)], issued by the President on 5th March, 2002, revoking the Proclamation issued by the President under the said article on 2nd June, 2001, in relation to the State of Manipur. (ii) Proclamation [G.S.R. No. 178(E)], issued by the President on the 8th March, 2002, under article 356 of the Constitution in relation to the State of Uttar Pradesh, under clause (3) of the said article. -
International Partners of ICMR an Overview of International
International Partners of ICMR An Overview of International Collaborative Projects in Health Research approved by Health Ministry’s Screening Committee (HMSC) during August, 2017 to July, 2020 (Volume V) International Health Division INDIAN COUNCIL OF MEDICAL RESEARCH, NEW DELHI Conceptualization, Design & Layout Mukesh Kumar, Harpreet Sandhu, Reema Roshan, Pratima Verma, Imran Ahmad, Rishi Chaudhary August, 2020 International Health Division (IHD), ICMR, Ansari Nagar, New Delhi-110029 Email: [email protected] Dated the 14th August, 2020 Foreword I am pleased to know that the International Health Division (IHD) of ICMR is publishing the fifth volume of the document entitled “An Overview of International Collaborative Research Projects in Health Research approved by Health Ministry’s Screening Committee (HMSC) during August, 2017 to July, 2020”. This document is in continuation of previous four volumes published by International Health Division in 2007, 2013, 2015, 2017, which have provided information on the international collaborative research projects approved by HMSC from January 2000 to July 2017. The earlier volumes released by IHD, enlisted the collaborative research projects undertaken by Scientists & Researchers in India in collaboration with their foreign partner scientists with foreign assistance and/or collaboration. The current document provides information about projects approved by HMSC during August 2017 to July 2020 alongwith information on ICMR’s international partnerships with different countries/agencies and details on the areas of interest and modes of collaboration. The recent decision taken for the organization of HMSC meetings at every alternate month and complete shifting over to the online submission/processing/review and consideration of international collaborative projects by the Health Ministry’s Screening Committee have further streamlined the procedures by cutting down the delays.