ROR1-CAR T-Cells Are Effective Against Lung and Breast Cancer in Advanced Microphysiologic 3D Tumor Models
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Unique Cell Surface Expression of Receptor Tyrosine Kinase ROR1 In
Human Cancer Biology Unique Cell Surface Expression of Receptor Tyrosine Kinase ROR1 in Human B-Cell Chronic Lymphocytic Leukemia Sivasubramanian Baskar,1KaYin Kwong,1Thomas Hofer,1Jessica M. Levy,1Michael G. Kennedy,1 Elinor Lee,3 Louis M. Staudt,2 Wyndham H.Wilson,2 Adrian Wiestner,3 and Christoph Rader1 Abstract Purpose: Gene expression profiling identified receptor tyrosine kinase ROR1, an embryonic protein involved in organogenesis, as a signature gene in B-cell chronic lymphocytic leukemia (B-CLL). To assess the suitability of ROR1 as a cell surface antigen for targeted therapy of B-CLL, we carried out a comprehensive analysis of ROR1protein expression. Experimental Design: Peripheral blood mononuclear cells, sera, and other adult tissues from B-CLL patients and healthy donors were analyzed qualitatively and quantitatively for ROR1 pro- tein expression by flow cytometry, cell surface biotinylation,Western blotting, and ELISA. Results: ROR1protein is selectively expressed on the surface of B-CLL cells, whereas normal B cells, other normal blood cells, and normal adult tissues do not express cell surface ROR1.More- over, cell surface expression of ROR1is uniform and constitutive, i.e., independent of anatomic niches, independent of biological and clinical heterogeneity of B-CLL, independent of B-cell activation, and found at similar levels in all B-CLL samples tested. The antibody binding capacity of B-CLL cell surface ROR1was determined to be in the range of103 to 104 molecules per cell. A portion of B-CLL cell surface ROR1was actively internalized upon antibody binding. Soluble ROR1protein was detectable in sera of <25% of B-CLL patients and a similar fraction of healthy donors at concentrations below 200 ng/mL. -

ROR1/CD19 Receptor Complex Promotes Growth of Mantle Cell Lymphoma Cells Independently of the B Cell Receptor–BTK Signaling Pathway † Qian Zhang,* Hong Y
Published September 18, 2019, doi:10.4049/jimmunol.1801327 Cutting Edge: ROR1/CD19 Receptor Complex Promotes Growth of Mantle Cell Lymphoma Cells Independently of the B Cell Receptor–BTK Signaling Pathway † Qian Zhang,* Hong Y. Wang,* Xiaobin Liu,* Selene Nunez-Cruz,* Mowafaqx Jillab, Olga Melnikov,† Kavindra Nath,‡ Jerry Glickson,‡ and Mariusz A. Wasik*,†, Inhibitors of Bruton tyrosine kinase (BTK), a kinase these mechanisms is of uttermost importance in design- downstream of BCR, display remarkable activity in a ing an appropriate therapeutic strategy to counteract the subset of mantle cell lymphoma (MCL) patients, but reprogramming. the drug resistance remains a considerable challenge. In ROR1 belongs to the receptor tyrosine kinase-like orphan this study, we demonstrate that aberrant expression of receptor (ROR) family and displays very restricted expression ROR1 (receptor tyrosine kinase-like orphan receptor 1), in normal tissues (11, 12). ROR1 is aberrantly expressed in seen in a large subset of MCL, results in BCR/BTK– various malignancies, including small lymphocytic lymphoma/ independent signaling and growth of MCL cells. ROR1 chronic lymphocytic leukemia (SLL/CLL) and MCL. ROR1 forms a functional complex with CD19 to persistently activates signaling molecules, such as RAC-1 and contractin activate the key cell signaling pathways PI3K–AKT and (13, 14), to promote cell proliferation, survival, and migration MEK–ERK in the BCR/BTK–independent manner. (13–15). CD19 is a B cell–specific receptor capable of stimu- lating the growth of malignant B cells (16). In normal This study demonstrates that ROR1/CD19 complex B lymphocytes, it is activated by SRC family kinases and effectively substitutes for BCR–BTK signaling to SYK, both downstream of BCR (17). -

Wnt5a/ROR1 Activates DAAM1 and Promotes the Migration in Osteosarcoma Cells
ONCOLOGY REPORTS 43: 601-608, 2020 Wnt5a/ROR1 activates DAAM1 and promotes the migration in osteosarcoma cells BIN DAI1*, YUCHENG SHEN1*, TING YAN2 and AILIANG ZHANG3 1Department of Orthopedics, Binhai County People's Hospital, Binhai, Jiangsu 224500; 2Safety Assessment and Research Center for Drug, Pesticide and Veterinary Drug of Jiangsu Province, Nanjing Medical University, Nanjing, Jiangsu 211166; 3Department of Spine Surgery, Third Affiliated Hospital of Soochow University, Changzhou, Jiangsu 213003, P.R. China Received May 11, 2019; Accepted November 8, 2019 DOI: 10.3892/or.2019.7424 Abstract. Receptor tyrosine kinase like orphan receptor 2 the last 100 years, the 5-year survival rate of classical osteo- (ROR2) regulates Wnt5a-induced cell migration by phosphory- sarcoma has been ~20% (2). Surgical and/or en bloc resection lating PI3K/Akt and activating RhoA in osteosarcoma. However, and radiotherapy are the primary options for the treatment of the role of Wnt5a signaling and its corresponding receptors in osteosarcoma. However, patients with advanced osteosarcoma the regulation of osteosarcoma metastasis remains poorly under- often suffer from metastasis or other complications. The stood. ROR1 monoclonal antibody (mAb) and short hairpin underlying molecular mechanism of cell migration is still (sh)RNA targeting ROR2 markedly inhibited the activity of unclear in osteosarcoma. dishevelled associated activator of morphogenesis 1 (DAAM1) Wnt ligands are a group of autocrine proteins binding to and RhoA and retarded cell migration in osteosarcoma. ROR1 LDL receptor-related proteins (LRPs), Frizzled (Fzd) recep- mAb and ROR2 shRNA destroyed the microfilament formation tors and/or receptor tyrosine kinase-like orphan receptors of osteosarcoma cells. Silencing of DAAM1 (with DAAM1 (RORs) (3,4). -

Background Technical Information Applications
Ror1 Antibody Applications: WB, IP, ICC Detected MW: 135 kDa Cat. No. CP10217 Species & Reactivity: Human Isotype: Mouse IgG1 BACKGROUND Receptor tyrosine kinase like orphan (Ror) proteins was activated and autophosphorylated by CKI- are type-I transmembrane receptor tyrosine epislon phosphorylation, the tyrosine kinase members of the neurotrophic tyrosine autophosphorylation and tyrosine kinase activation kinase receptor superfamily. The extracellular of Ror1 was not detected following CKI-epislon- region of Ror proteins contains an immunoglobulin mediated serine/threonine phosphorylation of domain, a Cys-rich domain, also called the Frizzled Ror1. These data imply the possibility that tyrosine domain, and a Kringle domain. Intracellularly, Ror kinase activity of Ror1 and Ror2 are regulated proteins possess a tyrosine kinase domain and a differentially.5 proline-rich domain straddled by two Ser/Thr-rich domains. The vertebrate Ror family members, References: Ror1 and Ror2, shares 58% amino acid sequence 1. Li, P. et al: PLOS one 5: e11859, 2010 identity. Analyses of mutants that are defective in 2. Paganoni, S. et al: Glia 46:456-66, 2004 the single nematode Ror demonstrate a role in cell 3. Paganoni, S. et al: Neurosci. 165:1261-74, 2010 4. Fukuda, T. et al: Proc. Natl. Acad. Sci. USA 105:3047- migration and in orienting cell polarity. Mice 52, 2008 lacking one of the two Ror gene products display 5. Kani, S.: Med. J. Kobe Univ. 64:59-65, 2004 defects in bone and heart formation. Similarly, two different human bone development disorders, dominant brachydactyly B and recessive Robinow syndrome result from mutations in one of the TECHNICAL INFORMATION human Ror genes. -

The Insulin and IGF-1 Receptors
The insulin and IGF-1 receptors Author: Pierre De Meyts Author title: MD, PHD, F.A.C.E. A bit of history The birth of the receptor concept dates back to the early work of John Newport Langley (1852-1925), a Cambridge physiologist, who postulated in 1905 that a "receptive substance" on the surface of skeletal muscle mediated the action of nicotine (1). At about the same time, Paul Ehrlich (1854-1915), a German immunologist who was the founding father of chemotherapy, came up with a "side chain theory" of cell receptors to explain the selectivity of immune reactions, winning him the Nobel Prize in Physiology or Medicine in 1908. His famous adage "Corpora non agunt nisi fixata" ("Substances do not act unless they are bound") is an elegant and concise early statement of the receptor theory (2). The receptor concept was put on more solid ground with the seminal 1948 paper of Raymond P. Ahlquist (1914-1983), an American pharmacologist of Swedish descent at the Medical College of Georgia, who proposed that the excitatory and inhibitory effects of adrenotropic agents were mediated by two separate receptors which he termed a and b (3). The receptors would however remain hypothetical entities until the late 60's, when direct methods to study their biochemistry were developed. The concept that insulin exerts its effects by acting at the membrane of target cells was proposed over 60 years ago by Rachmiel Levine (1910-1991), considered by many as one of the founding fathers of modern diabetology, then working at Walter Reese Hospital in Chicago. -

Protein Tyrosine Kinases: Their Roles and Their Targeting in Leukemia
cancers Review Protein Tyrosine Kinases: Their Roles and Their Targeting in Leukemia Kalpana K. Bhanumathy 1,*, Amrutha Balagopal 1, Frederick S. Vizeacoumar 2 , Franco J. Vizeacoumar 1,3, Andrew Freywald 2 and Vincenzo Giambra 4,* 1 Division of Oncology, College of Medicine, University of Saskatchewan, Saskatoon, SK S7N 5E5, Canada; [email protected] (A.B.); [email protected] (F.J.V.) 2 Department of Pathology and Laboratory Medicine, College of Medicine, University of Saskatchewan, Saskatoon, SK S7N 5E5, Canada; [email protected] (F.S.V.); [email protected] (A.F.) 3 Cancer Research Department, Saskatchewan Cancer Agency, 107 Wiggins Road, Saskatoon, SK S7N 5E5, Canada 4 Institute for Stem Cell Biology, Regenerative Medicine and Innovative Therapies (ISBReMIT), Fondazione IRCCS Casa Sollievo della Sofferenza, 71013 San Giovanni Rotondo, FG, Italy * Correspondence: [email protected] (K.K.B.); [email protected] (V.G.); Tel.: +1-(306)-716-7456 (K.K.B.); +39-0882-416574 (V.G.) Simple Summary: Protein phosphorylation is a key regulatory mechanism that controls a wide variety of cellular responses. This process is catalysed by the members of the protein kinase su- perfamily that are classified into two main families based on their ability to phosphorylate either tyrosine or serine and threonine residues in their substrates. Massive research efforts have been invested in dissecting the functions of tyrosine kinases, revealing their importance in the initiation and progression of human malignancies. Based on these investigations, numerous tyrosine kinase inhibitors have been included in clinical protocols and proved to be effective in targeted therapies for various haematological malignancies. -

Legendscreen™ Human and Mouse PE Kits
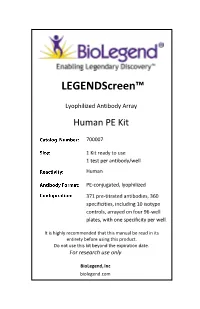
LEGENDScreen™ Human and Mouse PE Kits Introducing LEGENDScreen™ Human and Mouse PE Kits LEGENDScreen™ is the most cost-effective way to test this many directly-conjugated antibodies in a single assay. These kits can be used to screen cell lines and primary cells (PBMCs, bone marrow-derived cells, and cells isolated from tissues such as spleen and lymph node). The workflow is simple and easy. Just reconstitute the antibodies, add your cells, collect the samples, and then analyze. Cell staining is done directly in the plates, so no additional transfer of reconstituted antibody is required. The LEGENDScreen™ Human and Mouse Cell PE Kits are convenient, easy-to-use, and powerful tools for immunology, BioLegend’s LEGENDScreen™ products are lyophilized, fluorophore-conjugated antibodies stem cell, cancer research, and several other fields of research. provided in 96-well plates for the purpose of screening cell surface molecules on your cells of interest. Customize LEGENDScreen™ Individual fluorophore-conjugated antibodies or antibody We understand your needs for customization of research tools cocktails have been used as powerful tools for immunology, to fit your specific requirements. Our Custom Solutions Team cancer, and stem cell research. However, there is an increasing can customize LEGENDScreen™ products to include only the need for tools that can quickly screen cells for a large number of specificities that you want and provide them in bulk sizing. cell surface markers. The BioLegend LEGENDScreen™ Human and Mouse PE Kits are made to meet this need. Product Size Cat. No. LEGENDScreen™ Human PE Kit 1 kit (1 test per antibody) 700007 Why choose LEGENDScreen™? LEGENDScreen™ Mouse PE Kit 1 kit (1 test per antibody) 700005 • Large selection of specificities per kit. -

Targeting ROR1 Identifies New Treatment Strategies in Hematological Cancers Hanna Karvonen1, Wilhelmiina Niininen1, Astrid Murum
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Trepo - Institutional Repository of Tampere University This is an Accepted Manuscript of an article published by Portland Press. Biochemical Society Transactions. 2017.45(2):475-464. Available online: http:// dx.doi.org/10.1042/BST20160272. Targeting ROR1 identifies new treatment strategies in hematological cancers Hanna Karvonen1, Wilhelmiina Niininen1, Astrid Murumägi2 and Daniela Ungureanu1 1 BioMediTech, BMT, University of Tampere, 33014, Tampere, Finland 2 Institute for Molecular Medicine Finland, FIMM, University of Helsinki, 00290, Helsinki, Finland Corresponding author name and email: Daniela Ungureanu email: [email protected] Abbreviations: ALL, acute lymphocytic leukemia; B-ALL, B-cell acute lymphoblastic leukemia; BCR, B- cell receptor; BTK, Bruton tyrosine kinase; CLL, chronic lymphocytic leukemia; mAb, monoclonal antibody; MCL, mantle cell lymphoma; NHL, Non-Hodgkin lymphoma; ROR1/2, Receptor tyrosine kinase-like orphan receptor 1/2; Wnt, wingless-related integration site Abstract ROR1 is a member of the ROR receptor family consisting of two closely related type I transmembrane proteins, ROR1 and ROR2. Due to mutations in their canonical motifs required for proper kinase activity, RORs are classified as pseudokinases lacking detectable catalytic activity. ROR1 stands out for its selective and high expression in numerous blood and solid malignancies compared to a minimal expression in healthy adult tissues, suggesting high potential for this molecule as drug target for cancer therapy. Current understanding attributes a survival role for ROR1 in cancer cells, however its oncogenic function is cancer-type specific and involves various signaling pathways. High interest in ROR1 targeted therapies resulted in the development of ROR1 monoclonal antibodies such as cirmtuzumab, currently in phase I clinical trial for CLL. -
Legendscreen™
LEGENDScreen™ Lyophilized Antibody Array Human PE Kit 700007 1 Kit ready to use 1 test per antibody/well Human PE-conjugated, lyophilized 371 pre-titrated antibodies, 360 specificities, including 10 isotype controls, arrayed on four 96-well plates, with one specificity per well. It is highly recommended that this manual be read in its entirety before using this product. Do not use this kit beyond the expiration date. For research use only BioLegend, Inc biolegend.com LEGENDSCREEN™ Human PE Kit For Research Purposes Only. Not for use in diagnostic or therapeutic procedures. Purchase does not include or carry the right to resell or transfer this product either as a stand-alone product or as a component of another product. Any use of this product other than the permitted use without the express written authorization of BioLegend is strictly prohibited. 2 Biolegend.com LEGENDSCREEN™ Human PE Kit Table of Contents Page Description ........................................................................................ 4 Materials Provided ............................................................................ 4 Materials to be Provided by the End-User ........................................ 5 Storage and Handling ........................................................................ 5 Preparation of Cells for Staining ....................................................... 5 Plate Preparation .............................................................................. 6 Cell Staining Procedure ..................................................................... -

ROR1 Is Upregulated in Endometrial Cancer and Represents a Novel Therapeutic Target Dongli Liu1, Kate Gunther1, Luis A
www.nature.com/scientificreports OPEN ROR1 is upregulated in endometrial cancer and represents a novel therapeutic target Dongli Liu1, Kate Gunther1, Luis A. Enriquez1, Benjamin Daniels2, Tracy A. O’Mara3, Katrina Tang4, Amanda B. Spurdle3 & Caroline E. Ford1* ROR1 and ROR2 are receptor tyrosine kinases with altered expression in a range of cancers. Silencing ROR1 or ROR2 in diferent tumour types has been shown to inhibit proliferation and decrease metastatic potential. The aim of this study was to investigate the role of ROR1 and ROR2 in endometrial cancer via immunohistochemistry (IHC) in a large endometrial cancer patient cohort (n = 499) and through in vitro analysis in endometrial cancer cell lines. Correlation was assessed between ROR1/2 expression and clinicopathological parameters. Kaplan Meier curves were produced for 5-year progression free survival (PFS) and overall survival (OS) with low/moderate versus high ROR1/2 intensity. Cox multivariate regression was applied to analyse the efect of selected covariates on the PFS and OS. The efect of ROR1 and/or ROR2 modulation on cell proliferation, adhesion, migration and invasion was analysed in two endometrial cancer cell lines (KLE and MFE-296). We observed a signifcant decrease in OS and PFS in patients with high ROR1 expression. ROR1 silencing and ROR2 overexpression signifcantly inhibited proliferation of KLE endometrial cancer cells and decreased migration. This study supports the oncogenic role of ROR1 in endometrial cancer, and warrants investigation of future application of ROR1-targeting therapies in endometrial cancer patients. Endometrial cancer (EC) is the most prevalent gynaecological cancer and the sixth most common malignancy worldwide1. -

Tumor Antigen and Receptor Densities Regulate Efficacy of A
Original Article Tumor Antigen and Receptor Densities Regulate Efficacy of a Chimeric Antigen Receptor Targeting Anaplastic Lymphoma Kinase Alec J. Walker,1,4 Robbie G. Majzner,2,4 Ling Zhang,1 Kelsey Wanhainen,1 Adrienne H. Long,1 Sang M. Nguyen,1 Paola Lopomo,1 Marc Vigny,3 Terry J. Fry,1 Rimas J. Orentas,1 and Crystal L. Mackall2 1Pediatric Oncology Branch, Center for Cancer Research (CCR), National Cancer Institute (NCI), NIH, Bethesda, MD 20892, USA; 2Department of Pediatrics, Stanford University School of Medicine, Stanford, CA 94305, USA; 3INSERM/UPMC, Institut du Fer à Moulin, 75005 Paris, France – We explored the utility of targeting anaplastic lymphoma ki- oncogenesis in vitro and in vivo6 9 and correlates with poor prognosis nase (ALK), a cell surface receptor overexpressed on pediatric in patients with neuroblastoma.10,11 Strategies to target ALK in neuro- solid tumors, using chimeric antigen receptor (CAR)-based blastoma using small molecule inhibitors have seen limited success, immunotherapy. T cells expressing a CAR incorporating the potentially due to resistant kinase mutations.12 Targeting ALK overex- single-chain variable fragment sequence of the ALK48 mAb pression, independently of the highly mutated kinase domain, could linked to a 4-1BB-CD3z signaling domain lysed ALK-express- provide clinical benefit without risk for this type of mutagenic escape. ing tumor lines and produced interferon-gamma upon antigen stimulation but had limited anti-tumor efficacy in two xeno- T cells engineered to express chimeric antigen receptors (CARs) have graft models of human neuroblastoma. Further exploration recently joined the rapidly growing repertoire of immunotherapeutics demonstrated that cytokine production was highly dependent available to treat cancer. -

Evaluation of Expression and Function of VEGFR-2, PDGFR-Α, PDGFR-Β
Evaluation of Expression and Function of VEGFR2, PDGFRα, PDGFRβ, KIT, and RET in Canine Apocrine Gland of the Anal Sac Adenocarcinoma and Thyroid Carcinoma Thesis Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of The Ohio State University By Bridget Karen Urie, BS, MA, DVM Graduate Program in Comparative and Veterinary Medicine The Ohio State University 2012 Thesis Committee: Cheryl A. London, DVM, PhD, DACVIM, Co-Advisor William C. Kisseberth, DVM, PhD, DACVIM, Co-Advisor Ducan S. Russell, BMVS [Hons], DACVP Copyrighted by Bridget Karen Urie 2012 Abstract Biological responses to toceranib phosphate have been reported in both canine apocrine gland anal sac adenocarcinomas (AGASACA) and thyroid carcinomas (TC). However, little is known about the molecular biology of either of these tumor types and the mechanism of the biological activity of toceranib. In the present study, we investigated the presence and expression of known targets of toceranib and interrogated AGASACA and TC samples for the expression of VEGFR2, PDGFR, KIT and RET at both the message and protein level to begin to dissect the molecular basis for this observed activity. Samples from 24 primary AGASACA, 11 with paired metastatic lymph nodes, and 15 TC were evaluated using reverse-transcriptase polymerase chain reaction for detection of mRNA, phosphoprotein arrays to screen for evidence of protein phosphorylation, and tissue microarrays for immunohistochemical evaluation of protein expression. Messenger RNA from VEGFR2, PDGFR, KIT and RET was detected in all AGASACA samples. Messenger RNA for VEGFR2, PDGFR, and Kit was detected in all TC samples, while mRNA for Ret was amplified in 10/15 TC samples.