Metabolism Data for Common Medications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Opioid Powders Page: 1 of 9
Federal Employee Program® 1310 G Street, N.W. Washington, D.C. 20005 202.942.1000 Fax 202.942.1125 5.70.64 Section: Prescription Drugs Effective Date: April 1, 2020 Subsection: Analgesics and Anesthetics Original Policy Date: October 20, 2017 Subject: Opioid Powders Page: 1 of 9 Last Review Date: March 13, 2020 Opioid Powders Description Buprenorphine Powder, Butorphanol Powder, Codeine Powder, Hydrocodone Powder, Hydromorphone Powder, Levorphanol Powder, Meperidine Powder, Methadone Powder, Morphine Powder, Oxycodone Powder, Oxymorphone Powder Background Pharmacy compounding is an ancient practice in which pharmacists combine, mix or alter ingredients to create unique medications that meet specific needs of individual patients. Some examples of the need for compounding products would be: the dosage formulation must be changed to allow a person with dysphagia (trouble swallowing) to have a liquid formulation of a commercially available tablet only product, or to obtain the exact strength needed of the active ingredient, to avoid ingredients that a particular patient has an allergy to, or simply to add flavoring to medication to make it more palatable. Buprenorphine, butorphanol, codeine, hydrocodone, hydromorphone, levorphanol, meperidine, methadone, morphine, oxycodone, and oxymorphone powders are opioid drugs that are used for pain control. The intent of the criteria is to provide coverage consistent with product labeling, FDA guidance, standards of medical practice, evidence-based drug information, and/or published guidelines. Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, and because of the greater risks of overdose and death (1-15). Regulatory Status 5.70.64 Section: Prescription Drugs Effective Date: April 1, 2020 Subsection: Analgesics and Anesthetics Original Policy Date: October 20, 2017 Subject: Opioid Powders Page: 2 of 9 FDA-approved indications: 1. -

Hydromorphone
Hydromorphone WHAT IS HYDROMORPHONE? sedation, and reduced anxiety. It may also cause Hydromorphone belongs to a class of drugs mental clouding, changes in mood, nervousness, called “opioids,” which includes morphine. It and restlessness. It works centrally (in the has an analgesic potency of two to eight times brain) to reduce pain and suppress cough. greater than that of morphine and has a rapid Hydromorphone use is associated with both onset of action. physiological and psychological dependence. WHAT IS ITS ORIGIN? What is its effect on the body? Hydromorphone is legally manufactured and Hydromorphone may cause: distributed in the United States. However, • Constipation, pupillary constriction, urinary retention, users can obtain hydromorphone from nausea, vomiting, respiratory depression, dizziness, forged prescriptions, “doctor-shopping,” impaired coordination, loss of appetite, rash, slow or theft from pharmacies, and from friends and rapid heartbeat, and changes in blood pressure acquaintances. What are its overdose effects? What are the street names? Acute overdose of hydromorphone can produce: Common street names include: Severe respiratory depression, drowsiness • D, Dillies, Dust, Footballs, Juice, and Smack progressing to stupor or coma, lack of skeletal muscle tone, cold and clammy skin, constricted What does it look like? pupils, and reduction in blood pressure and heart Hydromorphone comes in: rate • Tablets, capsules, oral solutions, and injectable Severe overdose may result in death due to formulations respiratory depression. How is it abused? Which drugs cause similar effects? Users may abuse hydromorphone tablets by Drugs that have similar effects include: ingesting them. Injectable solutions, as well as • Heroin, morphine, hydrocodone, fentanyl, and tablets that have been crushed and dissolved oxycodone in a solution may be injected as a substitute for heroin. -

Pre - PA Allowance Age 12 Years of Age Or Older – Ultracet (Tramadol and Acetaminophen) and Codeine/APAP Products
OPIOID IR COMBO DRUGS Apadaz* (benzhydrocodone-acetaminophen), Codeine-acetaminophen, Dvorah* (dihydrocodeine-caffeine-acetaminophen*), Hydrocodone-acetaminophen, Hydrocodone- acetaminophen solution 10-325mg*, Hydrocodone-ibuprofen, Nalocet* (oxycodone- acetaminophen*), Oxycodone-acetaminophen, Oxycodone-aspirin, Oxycodone-ibuprofen, Primlev*/Prolate* (oxycodone-acetaminophen*), Tramadol-acetaminophen, Trezix (dihydrocodeine-caffeine-acetaminophen) *Prior authorization for certain non-covered formulations applies only to formulary exceptions Pre - PA Allowance Age 12 years of age or older – Ultracet (tramadol and acetaminophen) and Codeine/APAP products Quantity Patients 18 years or older will be able to fill the Pre-PA Allowance after they have filled an initial 7 day supply of IR opioid therapy or if they have been on IR or ER opioid therapy in the last 180 days Patients age 17 and under will require a PA after they have filled a 3 day supply of the Pre- PA Allowance Patients with opioid addiction treatment or methadone in the last 30 days will not be eligible for Pre-PA Allowance Immediate Release Tablets or Capsules ≤ 50 MME/day Medication Strength Quantity Limit Codeine/APAP soln 120-12 mg/5 mL Hydrocodone/APAP soln 7.5/325 mg/15 mL 5400 mL per 90 days Hydrocodone/APAP elixir 10/300 mg/15 mL Oxycodone/APAP soln 5-325 mg/5 mL 3000 mL per 90 days Hydrocodone/ibuprofen 5/200 mg, 7.5/200 mg, 10/200 mg 270 units per 90 days Oxycodone/ibuprofen 5/400 mg Oxycodone/APAP 10/325 mg Codeine/APAP 60/300 mg Hydrocodone/APAP 7.5/300 mg, 7.5/325 -
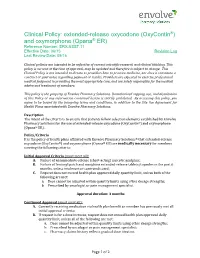
(Oxycontin®) and Oxymorphone (Opana® ER) Reference Number: ERX.NSST.17 Effective Date: 06/15 Revision Log Last Review Date: 09/16
Clinical Policy: extended-release oxycodone (OxyContin®) and oxymorphone (Opana® ER) Reference Number: ERX.NSST.17 Effective Date: 06/15 Revision Log Last Review Date: 09/16 Clinical policies are intended to be reflective of current scientific research and clinical thinking. This policy is current at the time of approval, may be updated and therefore is subject to change. This Clinical Policy is not intended to dictate to providers how to practice medicine, nor does it constitute a contract or guarantee regarding payment or results. Providers are expected to exercise professional medical judgment in providing the most appropriate care, and are solely responsible for the medical advice and treatment of members. This policy is the property of Envolve Pharmacy Solutions. Unauthorized copying, use, and distribution of this Policy or any information contained herein is strictly prohibited. By accessing this policy, you agree to be bound by the foregoing terms and conditions, in addition to the Site Use Agreement for Health Plans associated with Envolve Pharmacy Solutions. Description The intent of the criteria is to ensure that patients follow selection elements established by Envolve Pharmacy Solutions for the use of extended-release oxycodone (OxyContin®) and oxymorphone (Opana® ER). Policy/Criteria It is the policy of health plans affiliated with Envolve Pharmacy Solutions® that extended-release oxycodone (OxyContin®) and oxymorphone (Opana® ER) are medically necessary for members meeting the following criteria: Initial Approval Criteria (must meet all): A. Failure of an immediate-release (short-acting) narcotic analgesic; B. Failure of fentanyl patch and morphine extended-release tablets/capsules in the past 6 months, unless intolerant or contraindicated; C. -

Veterinary Anesthetic and Analgesic Formulary 3Rd Edition, Version G
Veterinary Anesthetic and Analgesic Formulary 3rd Edition, Version G I. Introduction and Use of the UC‐Denver Veterinary Formulary II. Anesthetic and Analgesic Considerations III. Species Specific Veterinary Formulary 1. Mouse 2. Rat 3. Neonatal Rodent 4. Guinea Pig 5. Chinchilla 6. Gerbil 7. Rabbit 8. Dog 9. Pig 10. Sheep 11. Non‐Pharmaceutical Grade Anesthetics IV. References I. Introduction and Use of the UC‐Denver Formulary Basic Definitions: Anesthesia: central nervous system depression that provides amnesia, unconsciousness and immobility in response to a painful stimulation. Drugs that produce anesthesia may or may not provide analgesia (1, 2). Analgesia: The absence of pain in response to stimulation that would normally be painful. An analgesic drug can provide analgesia by acting at the level of the central nervous system or at the site of inflammation to diminish or block pain signals (1, 2). Sedation: A state of mental calmness, decreased response to environmental stimuli, and muscle relaxation. This state is characterized by suppression of spontaneous movement with maintenance of spinal reflexes (1). Animal anesthesia and analgesia are crucial components of an animal use protocol. This document is provided to aid in the design of an anesthetic and analgesic plan to prevent animal pain whenever possible. However, this document should not be perceived to replace consultation with the university’s veterinary staff. As required by law, the veterinary staff should be consulted to assist in the planning of procedures where anesthetics and analgesics will be used to avoid or minimize discomfort, distress and pain in animals (3, 4). Prior to administration, all use of anesthetics and analgesic are to be approved by the Institutional Animal Care and Use Committee (IACUC). -

Heterodimerization of Μ and Δ Opioid Receptors: a Role in Opiate Synergy
The Journal of Neuroscience, 2000, Vol. 20 RC110 1of5 Heterodimerization of and ␦ Opioid Receptors: A Role in Opiate Synergy I. Gomes, B. A. Jordan, A. Gupta, N. Trapaidze, V. Nagy, and L. A. Devi Departments of Pharmacology and Anesthesiology, New York University School of Medicine, New York, New York 10016 Opiate analgesics are widely used in the treatment of severe -selective ligands results in a significant increase in the bind- pain. Because of their importance in therapy, different strate- ing of a ␦ receptor agonist. This robust increase is also seen in gies have been considered for making opiates more effective SKNSH cells that endogenously express both and ␦ recep- while curbing their liability to be abused. Although most opiates tors. Furthermore, we find that a ␦ receptor antagonist en- exert their analgesic effects primarily via opioid receptors, a hances both the potency and efficacy of the receptor signal- number of studies have shown that ␦ receptor-selective drugs ing; likewise a antagonist enhances the potency and efficacy can enhance their potency. The molecular basis for these find- of the ␦ receptor signaling. A combination of agonists ( and ␦ ings has not been elucidated previously. In the present study, receptor selective) also synergistically binds and potentiates we examined whether heterodimerization of and ␦ receptors signaling by activating the –␦ heterodimer. Taken together, could account for the cross-modulation previously observed these studies show that heterodimers exhibit distinct ligand between these two receptors. We find that co-expression of binding and signaling characteristics. These findings have im- and ␦ receptors in heterologous cells followed by selective portant clinical ramifications and may provide new foundations immunoprecipitation results in the isolation of –␦ het- for more effective therapies. -

1 Impact of Opioid Agonists on Mental Health in Substitution
Impact of opioid agonists on mental health in substitution treatment for opioid use disorder: A systematic review and Bayesian network meta-analysis of randomized clinical trials Supplementary Table 1_ Specific search strategy for each database The following general combination of search terms, Boolean operators, and search fields were used where “*” means that any extension of that word would be considered: Title field [opium OR opiate* OR opioid OR heroin OR medication assisted OR substitution treatment OR maintenance treatment OR methadone OR levomethadone OR buprenorphine OR suboxone OR (morphine AND slow) OR diamorphine OR diacetylmorphine OR dihydrocodeine OR hydromorphone OR opium tincture OR tincture of opium OR methadol OR methadyl OR levomethadyl] AND Title/Abstract field [trial* OR random* OR placebo] AND All fields [depress* OR anxiety OR mental] Wherever this exact combination was not possible, a more inclusive version of the search strategy was considered. Database Search Strategy Ovid for EBM Reviews - Cochrane Central Register of (opium or opiate$ or opioid or heroin or medication Controlled Trials August 2018; Embase 1974 to assisted or substitution treatment or maintenance September 07, 2018; MEDLINE(R) and Epub Ahead treatment or methadone or levomethadone or of Print, In-Process & Other Non-Indexed Citations buprenorphine or suboxone or (morphine and slow) or and Daily 1946 to September 07, 2018 diamorphine or diacetylmorphine or dihydrocodeine or hydromorphone or opium tincture or tincture of opium or methadol or methadyl -

The Inhibition of Enkephalin Catabolism by Dual Enkephalinase Inhibitor: a Novel Possible Therapeutic Approach for Opioid Use Disorders
Alvarez-Perez Beltran (Orcid ID: 0000-0001-8033-3136) Maldonado Rafael (Orcid ID: 0000-0002-4359-8773) THE INHIBITION OF ENKEPHALIN CATABOLISM BY DUAL ENKEPHALINASE INHIBITOR: A NOVEL POSSIBLE THERAPEUTIC APPROACH FOR OPIOID USE DISORDERS ALVAREZ-PEREZ Beltran1*, PORAS Hervé 2*, MALDONADO Rafael1 1 Laboratory of Neuropharmacology, Department of Experimental and Health Sciences, Universitat Pompeu Fabra, Barcelona Biomedical Research Park, c/Dr Aiguader 88, 08003 Barcelona, Spain, 2 Pharmaleads, Paris BioPark, 11 Rue Watt, 75013 Paris, France *Both authors participated equally to the manuscript Correspondence: Rafael Maldonado, Laboratori de Neurofarmacologia, Universitat Pompeu Fabra, Parc de Recerca Biomèdica de Barcelona (PRBB), c/Dr. Aiguader, 88, 08003 Barcelona, Spain. E-mail: [email protected] ABSTRACT Despite the increasing impact of opioid use disorders on society, there is a disturbing lack of effective medications for their clinical management. An interesting innovative strategy to treat these disorders consists in the protection of endogenous opioid peptides to activate opioid receptors, avoiding the classical opioid-like side effects. Dual Enkephalinase Inhibitors (DENKIs) physiologically activate the endogenous opioid system by inhibiting the enzymes responsible for the breakdown of enkephalins, protecting endogenous enkephalins, increasing their half-lives and physiological actions. The activation of opioid receptors by the increased enkephalin levels, and their well-demonstrated safety, suggest that DENKIs could represent a novel analgesic therapy and a possible effective treatment for acute opioid withdrawal, as well as a promising alternative to opioid substitution therapy minimizing side effects. This new pharmacological class of compounds could bring effective and safe medications avoiding the This article has been accepted for publication and undergone full peer review but has not been through the copyediting, typesetting, pagination and proofreading process which may lead to differences between this version and the Version of Record. -

Hydromorphone and Morphine Are Not the Same Drug!
HYDROmorphone and Morphine are not the same drug! HYDROmorphone and morphine are deemed high risk/high alert medications. An Independent Double Check (IDC) must be done to avoid errors when administering all high risk drugs. Please refer to Clinical Practice Standard 1-20-6-3-260. HYDROmorphone and morphine need to knows: HYDROmorphone is 5 times more potent than morphine! (e.g., 1 mg of HYDROmorphone PO is equivalent to 5 mg of morphine PO) When administered via the subcutaneous route, these drugs are twice as strong! Therefore when converting between oral and subcutaneous routes half the dose. (10 mg of oral morphine = 5 mg of subcutaneous morphine) HYDROmorphone and morphine: The name game. Both drugs are used in the management of moderate to severe pain. HYDROmorphone and morphine come in different brand names and formulations. HYDROmorphone = Dilaudid (Injectable), Jurnista (SR), HYDROmorph Contin (SR) Morphine = Morphine Sulphate (Injectable), MS-IR, M.O.S. (Liquid/Tablet/SR), M-Eslon (SR), Statex (Liquid/Tablet/Supp.), Doloral (Liquid), MS Contin (SR), Kadian (SR) (SR=Slow Release CAP) *As per NH, use the generic names (NOT THE BRAND NAME), of these drugs in your documentation. Common side effects: 3 ‘B’s of opioid prescribing: Common: Nausea, Vomiting, Constipation, Sedation, Syncope, Xerostomia (Dry Mouth), If your client is on an opioid: Delirium, Restlessness, Urinary Retention. Do they have a Breakthrough? Less Common: Respiratory Depression, Do they have something for Barfing? Opioid-Induced Neurotoxicity, Myoclonus, Do they have something for their Bowels? Pruritis (itching). Opioid induced neurotoxicity: What does it look like? Opioid induced neurotoxicity is the result of a build up of toxic opioid metabolites in the blood stream. -

Effects of Medication-Assisted Treatment (MAT) on Functional Outcomes Among Patients with Opioid Use Disorder (OUD)
NATIONAL DEFENSE RESEARCH INSTITUTE Effects of Medication- Assisted Treatment (MAT) for Opioid Use Disorder on Functional Outcomes A Systematic Review Margaret A. Maglione, Laura Raaen, Christine Chen, Gulrez Shah Azhar, Nima Shahidinia, Mimi Shen, Ervant J. Maksabedian Hernandez, Roberta M. Shanman, Susanne Hempel Prepared for the Office of the Secretary of Defense Approved for public release; distribution unlimited For more information on this publication, visit www.rand.org/t/RR2108 Published by the RAND Corporation, Santa Monica, Calif. © Copyright 2018 RAND Corporation R® is a registered trademark. Limited Print and Electronic Distribution Rights This document and trademark(s) contained herein are protected by law. This representation of RAND intellectual property is provided for noncommercial use only. Unauthorized posting of this publication online is prohibited. Permission is given to duplicate this document for personal use only, as long as it is unaltered and complete. Permission is required from RAND to reproduce, or reuse in another form, any of its research documents for commercial use. For information on reprint and linking permissions, please visit www.rand.org/pubs/permissions. The RAND Corporation is a research organization that develops solutions to public policy challenges to help make communities throughout the world safer and more secure, healthier and more prosperous. RAND is nonprofit, nonpartisan, and committed to the public interest. RAND’s publications do not necessarily reflect the opinions of its research clients and sponsors. Support RAND Make a tax-deductible charitable contribution at www.rand.org/giving/contribute www.rand.org Preface Over the past two decades, the U.S. Department of Defense (DoD) has invested unparalleled resources into developing effective treatments for military-related psychological health conditions. -

Opioid-Containing Cough and Cold Products - Assessing the Potential Risk of Opioid Use Disorder and Related Harms in Children and Adolescents
Summary Safety Review –Opioid-containing cough and cold products - Assessing the potential risk of opioid use disorder and related harms in children and adolescents Product: Cough and cold products containing opioids (including codeine, hydrocodone or normethadone) Potential Safety Issue: Opioid use disorders and related harms in children and adolescents Key Messages • The growing number of overdoses and harms caused by opioids is a major public health concern in Canada. Cough and cold products containing opioids (including codeine, hydrocodone or normethadone) are authorized for sale in Canada to treat cough and cold symptoms in adults and children. • Health Canada reviewed the risk of opioid use disorder and related harms from these products after the United States Food and Drug Administration (US FDA) advised against using these products in children and adolescents in 2018. Health Canada’s safety review found limited evidence to link opioid-containing cough and cold products with opioid use disorders and related harms in children and adolescents. • These products are linked to other known harms (i.e., breathing problems), and there is limited evidence to support the effectiveness of these products in children and adolescents. There are other products available in Canada to help relieve the symptoms of cough and cold in children. • Therefore, Health Canada, as a precautionary measure, is advising Canadians against the use of these products among children and adolescents under 18 years of age. Health Canada will notify the manufacturers to update the product safety information of opioid- containing cough and cold products to limit the recommended age of use (indication) to adults only, 18 years of age and older. -

List of Narcotic Drugs Under International Control
International Narcotics Control Board Yellow List Annex to Forms A, B and C 59th edition, July 2020 LIST OF NARCOTIC DRUGS UNDER INTERNATIONAL CONTROL Prepared by the INTERNATIONAL NARCOTICS CONTROL BOARD* Vienna International Centre P.O. Box 500 A-1400 Vienna, Austria Internet address: http://www.incb.org/ in accordance with the Single Convention on Narcotic Drugs, 1961** Protocol of 25 March 1972 amending the Single Convention on Narcotic Drugs, 1961 * On 2 March 1968, this organ took over the functions of the Permanent Central Narcotics Board and the Drug Supervisory Body, r etaining the same secretariat and offices. ** Subsequently referred to as “1961 Convention”. V.20-03697 (E) *2003697* Purpose The Yellow List contains the current list of narcotic drugs under international control and additional relevant information. It has been prepared by the International Narcotics Control Board to assist Governments in completing the annual statistical reports on narcotic drugs (Form C), the quarterly statistics of imports and exports of narcotic drugs (Form A) and the estimates of annual requirements for narcotic drugs (Form B) as well as related questionnaires. The Yellow List is divided into four parts: Part 1 provides a list of narcotic drugs under international control in the form of tables and is subdivided into three sections: (1) the first section includes the narcotic drugs listed in Schedule I of the 1961 Convention as well as intermediate opiate raw materials; (2) the second section includes the narcotic drugs listed in Schedule II of the 1961 Convention; and (3) the third section includes the narcotic drugs listed in Schedule IV of the 1961 Convention.