Blood Cultures - Aerobic & Anaerobic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Use of Cell Culture in Virology for Developing Countries in the South-East Asia Region © World Health Organization 2017
USE OF CELL C USE OF CELL U LT U RE IN VIROLOGY FOR DE RE IN VIROLOGY V ELOPING C O U NTRIES IN THE NTRIES IN S O U TH- E AST USE OF CELL CULTURE A SIA IN VIROLOGY FOR R EGION ISBN: 978-92-9022-600-0 DEVELOPING COUNTRIES IN THE SOUTH-EAST ASIA REGION World Health House Indraprastha Estate, Mahatma Gandhi Marg, New Delhi-110002, India Website: www.searo.who.int USE OF CELL CULTURE IN VIROLOGY FOR DEVELOPING COUNTRIES IN THE SOUTH-EAST ASIA REGION © World Health Organization 2017 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial- ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition.” Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. -

Pdfs/ Ommended That Initial Cultures Focus on Common Pathogens, Pscmanual/9Pscssicurrent.Pdf)
Clinical Infectious Diseases IDSA GUIDELINE A Guide to Utilization of the Microbiology Laboratory for Diagnosis of Infectious Diseases: 2018 Update by the Infectious Diseases Society of America and the American Society for Microbiologya J. Michael Miller,1 Matthew J. Binnicker,2 Sheldon Campbell,3 Karen C. Carroll,4 Kimberle C. Chapin,5 Peter H. Gilligan,6 Mark D. Gonzalez,7 Robert C. Jerris,7 Sue C. Kehl,8 Robin Patel,2 Bobbi S. Pritt,2 Sandra S. Richter,9 Barbara Robinson-Dunn,10 Joseph D. Schwartzman,11 James W. Snyder,12 Sam Telford III,13 Elitza S. Theel,2 Richard B. Thomson Jr,14 Melvin P. Weinstein,15 and Joseph D. Yao2 1Microbiology Technical Services, LLC, Dunwoody, Georgia; 2Division of Clinical Microbiology, Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, Minnesota; 3Yale University School of Medicine, New Haven, Connecticut; 4Department of Pathology, Johns Hopkins Medical Institutions, Baltimore, Maryland; 5Department of Pathology, Rhode Island Hospital, Providence; 6Department of Pathology and Laboratory Medicine, University of North Carolina, Chapel Hill; 7Department of Pathology, Children’s Healthcare of Atlanta, Georgia; 8Medical College of Wisconsin, Milwaukee; 9Department of Laboratory Medicine, Cleveland Clinic, Ohio; 10Department of Pathology and Laboratory Medicine, Beaumont Health, Royal Oak, Michigan; 11Dartmouth- Hitchcock Medical Center, Lebanon, New Hampshire; 12Department of Pathology and Laboratory Medicine, University of Louisville, Kentucky; 13Department of Infectious Disease and Global Health, Tufts University, North Grafton, Massachusetts; 14Department of Pathology and Laboratory Medicine, NorthShore University HealthSystem, Evanston, Illinois; and 15Departments of Medicine and Pathology & Laboratory Medicine, Rutgers Robert Wood Johnson Medical School, New Brunswick, New Jersey Contents Introduction and Executive Summary I. -

BBL Group a Selective Strep Agar with 5% Sheep Blood (Ssa )
BBL™ Group A Selective Strep Agar with 5% Sheep Blood (ssA™) and ! BBL™ Trypticase™ Soy Agar with 5% Sheep Blood (TSA II)–Bi-Plate " L007379 • Rev. 09 • December 2006 QUALITY CONTROL PROCEDURES I INTRODUCTION Group A Selective Strep Agar with 5% Sheep Blood (ssA) is a selective medium for use in the isolation and presumptive identification of group A streptococci from throat cultures and other specimens. Trypticase Soy Agar with 5% Sheep Blood (TSA II) is used for the growth of fastidious organisms and for the visualization of hemolytic reactions. The TSA II medium sector is marked "I" and the ssA medium sector is marked "II" in the bi-plate dish. II PERFORMANCE TEST PROCEDURE A. Group A Selective Strep Agar with 5% Sheep Blood 1. Inoculate representative samples with the cultures diluted to contain 103–104 CFU/0.01 mL. a. To each plate, add 0.01 mL of the dilution and streak for isolation. Make a stab in the primary streak area before streaking the rest of the plate. b. Place a Taxo™ A disc at the intersection of the first and second area of streaking on all plates inoculated with S. pyogenes strains. c. Incubate plates at 35 ± 2°C in an aerobic atmosphere supplemented with carbon dioxide. d. Include Trypticase Soy Agar with 5% Sheep Blood (TSA II) plates as nonselective controls for all organisms. 2. Examine plates after 18–24 h for beta hemolysis in the stabbed area and for amount of growth, inhibition, colony size and hemolytic reactions. Read and record the size of the zone around the Taxo A disc with S. -

Comparison of Throat Culture and Latex Agglutination Test for Streptococcal Pharyngitis
Comparison of Throat Culture and Latex Agglutination Test for Streptococcal Pharyngitis Paul M. Fischer, MD, and Pamela L. Mentrup, MLT Augusta, Georgia Numerous reports have recently appeared in the clinical microbiology litera ture that describe agglutination tests for identifying patients with group A streptococcal pharyngitis. These studies have indicated a close correlation between the results of the agglutination tests and traditional throat culturing. This paper describes a comparison study of 100 consecutive throat swab specimens using a commercially available agglutination test and routine throat culturing. The cultures were interpreted by an individual who was blinded to the agglutination test results. All agglutination testing was done by two laboratory members of a family practice office staff. The agglutination procedure was easy to perform and clear to interpret. The test sensitivity and specificity compared well with that reported in the literature from microbiol ogy laboratories. The new agglutination tests are useful in the office labora tory for the identification of group A streptococci. Their primary advantage compared with throat culturing is the rapid availability of test results. Most clinicians recognize the need to differ An additional problem with throat culturing has entiate group A streptococcal pharyngitis from been that clinicians are uncomfortable with the other infectious causes of pharyngitis because of 24- to 48-hour test time. Inconsistent patterns of the reduction in suppurative sequelae and clinical practice have therefore developed, includ rheumatic fever when streptococcal pharyngitis is ing waiting for the culture results before treating, treated with antibiotics.1 New evidence has also prescribing penicillin to all patients until the re supported the intuitive feeling of some clinicians sults are available, or treating all patients without that early antibiotic treatment will decrease the confirming the diagnosis by culture. -

Prevalence and Antibiotic Resistance Pattern of Streptococcus Genus And
Journal of Medical Microbiology and Infectious Diseases ISSN: 2345-5349 eISSN: 2345-5330 Prevalence and Antibiotic Resistance Pattern of Streptococcus Genus and Other Pathogens Isolated from Throat Culture Samples of Patients in Fatemeh Al- Zahra Hospital of Sari, Iran 1 2* 3 1 Mohsen Nazari , Mohammad Taha Ebrahimi , Niloofar Mobarezpour , Amin Sepehr 1Department of Bacteriology, Pasteur Institute of Iran, Tehran, Iran; 2Department of Microbiology, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran; 3PPD Tuberculin Department, Razi Vaccine & Serum Research Institute, Karaj, Iran A R T I C L E I N F O A B S T R A C T Original Article Introduction: Tracheal tubes are among the primary means of infection transmission in hospitals. Therefore, identifying microbial agents transmitted via this route is necessary to control and prevent these infections. This study aimed Keywords: Antibiotic Resistance pattern, Tracheal Tube, Streptococcal to investigate the prevalence of pharyngeal-contaminating microorganisms and species their antibiotic resistance pattern. Methods: In this cross-sectional study, we used 117 pharyngeal swabs samples obtained from patients referred to Fatemeh Zahra Hospital of Sari, Iran, in 2018. The Samples were obtained using the Received: 15 Jul. 2020 sterile cotton swab from the throat and then cultured in the sheep blood agar. Received in revised form: 26 Jan. 2021 The positive colonies for the alpha-hemolytic test were subcultured on the Accepted: 26 Jan. 2021 Mueller-Hinton agar for further assays, including the susceptibility to optochin, DOI: 10.29252/JoMMID.8.4.143 catalase test, Gram's polychromatic stain, microscopic examination, pyrrolidonyl aminopeptidase (PYR) test, sensitization to bacitracin, and latex agglutination *Correspondence assay. -
Update Antibiotics: Why and Why Not to 2018
Antibiotics Why and Why Not 2018 Academic Detailing Service Planning committee Content Experts Clinical reviewers Paul Bonnar MD FRCPC, Assistant Professor Division of Infectious Disease, Dalhousie University, Medical Director, NSHA Antimicrobial Stewardship Program Jeannette Comeau MD MSc FRCPC FAAP, Pediatric Infectious Diseases Consultant, Assistant Professor, Dalhousie University, Medical Director, Infection Prevention and Control, Medical Lead, Antibiotic Stewardship IWK Health Centre Ian Davis MD CCFP FRCPC, Assistant Professor Divisions of Infectious Disease and Microbiology and Immunology, Dalhousie University Lynn Johnston MD MSc FRCPC, Professor Division of Infectious Disease, Dalhousie University Valerie Murphy BScPharm ACPR Antimicrobial Stewardship Pharmacist, Nova Scotia Health Authority, Central Zone Tasha Ramsey BScPharm, ACPR, PharmD, Assistant Professor, College of Pharmacy, Dalhousie University, Infectious Diseases and Internal Medicine Clinical Coordinator, Pharmacy Department, Nova Scotia Health Authority Kathy Slayter BScPharm, Pharm D, FCSHP, Clinical Pharmacy Specialist, Antimicrobial Stewardship/Infectious Diseases, Adjunct Assistant Professor Faculty of Medicine; Department of Medicine, Division of Infectious Diseases and Faculty of Graduate Studies, Dalhousie University, Canadian Center for Vaccinology Drug evaluation pharmacists Jennifer Fleming BScPharm ACPR Drug Evaluation Unit, Nova Scotia Health Kim Kelly BScPharm, Drug Evaluation Unit, Nova Scotia Health (retired) Family Physician Advisory Panel -

Microbiology Specimen Collection
Martin Health System Stuart, Florida Laboratory Services Microbiology Specimen Collection The recovery of pathogenic organisms responsible for an infectious process is dependent on proper collection and transportation of a specimen. An improperly collected or transported specimen may lead to failure to isolate the causative organism(s) of an infectious disease or may result in the recovery and subsequent treatment of contaminating organisms. Improper handling of specimens may also lead to accidental exposure to infectious material. GENERAL GUIDELINES FOR COLLECTION: 1. Follow universal precaution guidelines, treating all specimens as potentially hazardous. 2. Whenever possible, collect specimen before antibiotics are administered. 3. Collect the specimen from the actual site of infection, avoiding contamination from adjacent tissues or secretions. 4. Collect the specimen at optimal time i.e. Early morning sputum for AFB First voided specimen for urine culture Specimens ordered x 3 should be 24 hours apart (exception: Blood cultures which are collected as indicated by the physician) 5. Collect sufficient quantity of material for tests requested. 6. Use appropriate collection and transport container. Refer to the Microbiology Quick Reference Chart or to the specific source guidelines. Containers should always be tightly sealed and leak-proof 7. Label the specimen with the Patient’s First and Last Name Date of Birth Collection Date and Time Collector’s First and Last Name Source 8. Submit specimen in the sealed portion of a Biohazard specimen bag. 9. Place signed laboratory order in the outside pocket of the specimen bag. 10. Include any pertinent information i.e. recent travel or relocation, previous antibiotic therapy, unusual suspected organisms, method or environment of wound infliction 11. -

CDC/NHSN Surveillance Definitions for Specific Types of Infections
Surveillance Definitions CDC/NHSN Surveillance Definitions for Specific Types of Infections INTRODUCTION This chapter contains the CDC/NHSN surveillance definitions and criteria for all specific types of infections. Comments and reporting instructions that follow the site-specific criteria provide further explanation and are integral to the correct application of the criteria. This chapter also provides further required criteria for the specific infection types that constitute organ/space surgical site infections (SSI) (e.g., mediastinitis [MED] that may follow a coronary artery bypass graft, intra-abdominal abscess [IAB] after colon surgery). Additionally, it is necessary to refer to the criteria in this chapter when determining whether a positive blood culture represents a primary bloodstream infection (BSI) or is secondary to a different type of HAI (see Appendix 1 Secondary Bloodstream Infection (BSI) Guide). A BSI that is identified as secondary to another site of HAI must meet one of the criteria of HAI detailed in this chapter. Secondary BSIs are not reported as separate events in NHSN, nor can they be associated with the use of a central line. Also included in this chapter are the criteria for Ventilator-Associated Events (VAEs). It should be noted that Ventilator-Associated Condition (VAC), the first definition within the VAE surveillance definition algorithm and the foundation for the other definitions within the algorithm (IVAC, Possible VAP, Probable VAP) may or may not be infection-related. CDC/NHSN SURVEILLANCE DEFINITIONS OF HEALTHCARE–ASSOCIATED INFECTION Present on Admission (POA) Infections To standardize the classification of an infection as present on admission (POA) or a healthcare- associated infection (HAI), the following objective surveillance criteria have been adopted by NHSN. -

Infectious Mononucleosis
THEME: Systemic viral infections Infectious mononucleosis BACKGROUND Infectious mononucleosis is caused by the ubiquitous Epstein-Barr virus. It is a common condition usually affecting adolescents and young adults. Most cases are mild to moderate in severity with full recovery taking place over several weeks. More severe cases Patrick G P Charles and unusual complications occasionally occur. OBJECTIVE After presenting a case of severe infectious mononucleosis, the spectrum of disease is given. Diagnosis and complications are reviewed as well as management including the possible role for antiviral medications or corticosteroid therapy. DISCUSSION The majority of cases of infectious mononucleosis are self limiting and require only supportive care. More severe cases, although unusual, may require admission to hospital and even to an intensive care unit. Corticosteroid therapy may be indicated for severe airway obstruction or other severe complications, but should be avoided unless the benefits outweigh potential risks. Antiviral therapy has no proven benefit. Patrick G P Charles, Case history MBBS, is a registrar, Victorian Infectious A 21 year old exchange student was admitted with a week long history of sore throat, fever, lethargy, anorexia Disease Reference and headache. His intake of food and fluids had been markedly reduced. He sought medical advice when he Laboratory, North noticed he had become jaundiced. He had no risk factors for, nor contact with, viral hepatitis. Melbourne, Victoria. Initial examination revealed he was volume depleted and clearly icteric. He was febrile at 38.6ºC and had generalised lymphadenopathy, hepatosplenomegaly and markedly enlarged tonsils that were mildly inflamed. There was no tonsillar exudate or palatal petechiae. -

Laboratory Diagnosis of Sexually Transmitted Infections, Including Human Immunodeficiency Virus
Laboratory diagnosis of sexually transmitted infections, including human immunodeficiency virus human immunodeficiency including Laboratory transmitted infections, diagnosis of sexually Laboratory diagnosis of sexually transmitted infections, including human immunodeficiency virus Editor-in-Chief Magnus Unemo Editors Ronald Ballard, Catherine Ison, David Lewis, Francis Ndowa, Rosanna Peeling For more information, please contact: Department of Reproductive Health and Research World Health Organization Avenue Appia 20, CH-1211 Geneva 27, Switzerland ISBN 978 92 4 150584 0 Fax: +41 22 791 4171 E-mail: [email protected] www.who.int/reproductivehealth 7892419 505840 WHO_STI-HIV_lab_manual_cover_final_spread_revised.indd 1 02/07/2013 14:45 Laboratory diagnosis of sexually transmitted infections, including human immunodeficiency virus Editor-in-Chief Magnus Unemo Editors Ronald Ballard Catherine Ison David Lewis Francis Ndowa Rosanna Peeling WHO Library Cataloguing-in-Publication Data Laboratory diagnosis of sexually transmitted infections, including human immunodeficiency virus / edited by Magnus Unemo … [et al]. 1.Sexually transmitted diseases – diagnosis. 2.HIV infections – diagnosis. 3.Diagnostic techniques and procedures. 4.Laboratories. I.Unemo, Magnus. II.Ballard, Ronald. III.Ison, Catherine. IV.Lewis, David. V.Ndowa, Francis. VI.Peeling, Rosanna. VII.World Health Organization. ISBN 978 92 4 150584 0 (NLM classification: WC 503.1) © World Health Organization 2013 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for non-commercial distribution – should be addressed to WHO Press through the WHO web site (www.who.int/about/licensing/copyright_form/en/index.html). -
Antibiotic Susceptibility Evaluation of Group a Streptococcus Isolated
Original Article Infection & http://dx.doi.org/10.3947/ic.2015.47.4.225 Infect Chemother 2015;47(4):225-230 Chemotherapy ISSN 2093-2340 (Print) · ISSN 2092-6448 (Online) Antibiotic Susceptibility Evaluation of Group A Streptococcus Isolated from Children with Pharyngitis: A Study from Iran Shirin Sayyahfar1, Alireza Fahimzad2, Amir Naddaf3, and Sara Tavassoli4 1Division of Pediatric Infectious Diseases, Departement of Pediatrics, Ali Asghar Children Hospital, Iran University of Medical Sciences; 2Division of Pediatric Infectious Diseases, Departement of Pediatrics, Pediatric Infectious Research Center, Mofid Children Hospital, Shahid Beheshti University of Medical Sciences, Tehran; 3Department of Pediatrics, Fasa University of Medical sciences, Fasa; 4Traditional Medicine, Tehran University of Medical Sciences, Tehran, Iran Background: The aim of this study was to evaluate the antibiotic susceptibility of Group A streptococcus (GAS) to antibiotics usually used in Iran for treatment of GAS pharyngitis in children. Materials and Methods: From 2011 to 2013, children 3-15 years of age with acute tonsillopharyngitis who attended Mofid Children’s Hospital clinics and emergency ward and did not meet the exclusion criteria were enrolled in a prospective study in a sequential manner. The isolates strains from throat culture were identified as GAS by colony morphology, gram staining, beta hemolysis on blood agar, sensitivity to bacitracin, a positive pyrrolidonyl aminopeptidase (PYR) test result, and the presence of Lancefield A antigen determined by agglutination test. Antimicrobial susceptibility was identified by both disk diffusion and broth dilution methods. Results: From 200 children enrolled in this study, 59 (30%) cases were culture positive for GAS. All isolates were sensitive to penicil- lin G. -
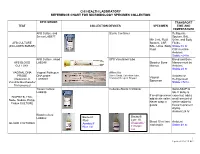
Chi Health Laboratory Reference Chart for Microbiology Specimen Collection
CHI HEALTH LABORATORY REFERENCE CHART FOR MICROBIOLOGY SPECIMEN COLLECTION EPIC ORDER TRANSPORT TEST COLLECTION DEVICES SPECIMEN TIME AND TEMPERATURE AFB Culture and Sterile Container Refrigerate Smear LAB877 Sputum, BAL, Min 2 mL Fluid: Urine, and Body AFB CULTURE Sputum, CSF, Fluids (INCLUDES SMEAR) BAL, Urine, Body Stable:72 hr. Fluid CSF must be Ambient Stable:<24 hr. AFB Culture, blood SPS Vacutainer tube Blood and Bone AFB BLOOD LAB246 Blood or Bone Marrow must be CULTURE Marrow Ambient Stable:24 hr VAGINAL DNA Vaginal Pathogen Affirm Kit PROBE DNA probe Sterile Swab, Collection Tube, Ambient or Vaginal (Detection of LAB3001 Transport Reagent Dropper Refrigerated Specimen Candida/Gardnerella/ Stable:<72 hr. Trichomonas) Tissue Culture Cultures-Sterile Container Send ASAP to LAB898 lab. If delay is If small specimen expected, add a BIOPSIES, FNA, add sterile saline. small amount of Node, Nodule, Polyp, Never wrap in sterile saline to Tissue CULTURE gauze tissue to prevent drying. Ambient 24 hr Blood Culture Bactec® LAB462 Bactec® Lytic 10 Plus+ Blood 10 ml into Ambient BLOOD CULTURES Anaerobic/ Aerobic/F each bottle Stable:48 hr. Blue Lid F Purple Lid 1 Updated 1/10/19 KG EPIC ORDER TRANSPORT TEST COLLECTION DEVICES SPECIMEN TIME AND TEMPERATURE Bordetella Nasopharyngeal Freeze pertussis/ Mini Swab Stable: 3 months BORDETELLA Parapertussis by PERTUSSIS PCR PCR LAB923 (discard large UVTM swab) Universal Viral Transport Media Mini-tip ESwab Bacterial Culture Chlamydia by PCR Dirty Urine First (Urine) LAB5763 Morning Void (No clean catch CHLAMYDIA Chlamydia/ or midstream Stable at 2-30° TRACHOMATIS by Gonorrhea by PCR Cobas® Urine PCR Media tube urine).