Inequity in Childhood Immunization Between Urban and Rural Areas Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Population According to Religion, Tables-6, Pakistan
-No. 32A 11 I I ! I , 1 --.. ".._" I l <t I If _:ENSUS OF RAKISTAN, 1951 ( 1 - - I O .PUlA'TION ACC<!>R'DING TO RELIGIO ~ (TA~LE; 6)/ \ 1 \ \ ,I tin N~.2 1 • t ~ ~ I, . : - f I ~ (bFICE OF THE ~ENSU) ' COMMISSIO ~ ER; .1 :VERNMENT OF PAKISTAN, l .. October 1951 - ~........-.~ .1',l 1 RY OF THE INTERIOR, PI'ice Rs. 2 ~f 5. it '7 J . CH I. ~ CE.N TABLE 6.-RELIGION SECTION 6·1.-PAKISTAN Thousand personc:. ,Prorinces and States Total Muslim Caste Sch~duled Christian Others (Note 1) Hindu Caste Hindu ~ --- (l b c d e f g _-'--- --- ---- KISTAN 7,56,36 6,49,59 43,49 54,21 5,41 3,66 ;:histan and States 11,54 11,37 12 ] 4 listricts 6,02 5,94 3 1 4 States 5,52 5,43 9 ,: Bengal 4,19,32 3,22,27 41,87 50,52 1,07 3,59 aeral Capital Area, 11,23 10,78 5 13 21 6 Karachi. ·W. F. P. and Tribal 58,65 58,58 1 2 4 Areas. Districts 32,23 32,17 " 4 Agencies (Tribal Areas) 26,42 26,41 aIIjab and BahawaJpur 2,06,37 2,02,01 3 30 4,03 State. Districts 1,88,15 1,83,93 2 19 4,01 Bahawa1pur State 18,22 18,08 11 2 ';ind and Kbairpur State 49,25 44,58 1,41 3,23 2 1 Districts 46,06 41,49 1,34 3,20 2 Khairpur State 3,19 3,09 7 3 I.-Excluding 207 thousand persons claiming Nationalities other than Pakistani. -

Reclaiming Prosperity in Khyber- Pakhtunkhwa
Working paper Reclaiming Prosperity in Khyber- Pakhtunkhwa A Medium Term Strategy for Inclusive Growth Full Report April 2015 When citing this paper, please use the title and the following reference number: F-37109-PAK-1 Reclaiming Prosperity in Khyber-Pakhtunkhwa A Medium Term Strategy for Inclusive Growth International Growth Centre, Pakistan Program The International Growth Centre (IGC) aims to promote sustainable growth in developing countries by providing demand-led policy advice informed by frontier research. Based at the London School of Economics and in partnership with Oxford University, the IGC is initiated and funded by DFID. The IGC has 15 country programs. This report has been prepared under the overall supervision of the management team of the IGC Pakistan program: Ijaz Nabi (Country Director), Naved Hamid (Resident Director) and Ali Cheema (Lead Academic). The coordinators for the report were Yasir Khan (IGC Country Economist) and Bilal Siddiqi (Stanford). Shaheen Malik estimated the provincial accounts, Sarah Khan (Columbia) edited the report and Khalid Ikram peer reviewed it. The authors include Anjum Nasim (IDEAS, Revenue Mobilization), Osama Siddique (LUMS, Rule of Law), Turab Hussain and Usman Khan (LUMS, Transport, Industry, Construction and Regional Trade), Sarah Saeed (PSDF, Skills Development), Munir Ahmed (Energy and Mining), Arif Nadeem (PAC, Agriculture and Livestock), Ahsan Rana (LUMS, Agriculture and Livestock), Yasir Khan and Hina Shaikh (IGC, Education and Health), Rashid Amjad (Lahore School of Economics, Remittances), GM Arif (PIDE, Remittances), Najm-ul-Sahr Ata-ullah and Ibrahim Murtaza (R. Ali Development Consultants, Urbanization). For further information please contact [email protected] , [email protected] , [email protected] . -
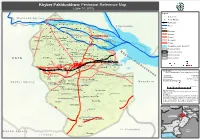
Khyber Pakhtunkhwa- Peshawar Reference Map (June 14, 2012)
Khyber Pakhtunkhwa- Peshawar Reference Map (June 14, 2012) Legend ! ! ! Settlements M o h m a n d A g e n c y ! ! ! ! ! ! "' Health Facilities WAZIRBAGH Railway Line ! ! ! ! "' ! SHA!GI BAL!A(KHAT!KI) ! ! ! Jogani "' Rivers ! C h a r s a d d a ! C h a r s a d d a ! ! ! ! ! ! Kha! tki ! ! Roads SAEED ABAD ! CHAGHAR MATTI "' FAQIR KILLAYGARA TAJIK"' Motorway ! ! "'! ! "' ! ! ! ! ! ! ! ! Highway HUSSAIN ABAD Gul Bela GUL BELLA ! "' TAKHT ABAD "' "' ! !Gar!hi S! her D!ad ! ! ! ! ! ! ! ! ! ! NASIR BAGH "' "' Primary KAFOOR DHERI Chaghar "'Matti ! "' MATHRA NAHAQI ! "' MATHRA "' KHARAKI Secondary ! Pana!m Dhe!ri ! ! ! ! ! ! ! ! ! ! ! ! ! "' ! ! ! "' CHARPERIZATakhat Abad ! "' Tertiary SUFAID DHERI PUTWAR BALLA KHAZANA ! "' ! ! "'! ! ! ! ! ! ! ! ! ! ! "' Flood Extenct (Oct -Nov 2010) ! ! Nahaqi ! Kaniza Ka!foor D!heri ! ! ! ! ! ! MA! NDRA !KHEL ! ! ! ! ! Peshawar District ! "' DARMANGI K Provincial boundary ! ! ! ! "' ! ! ! Khaza! na ! ! ! ! h "' Haryana Payan ! Mathra PAKHA GHULAM WADPAGA y District boundary ! TARAI PAYAN(SHAQI H.K) "' Kankola "' b ! ! Shahi Bala ! ! ! ! ! ! ! ! ! ! ! e Union Councils PALOSA!IUrban BUDH!AI F A T A "' ! ! "'! r ! Budhni Palosi Pajjagi ! ! P ! ! ! ! ! ! ! ! ! ! ! "' JO!GANI ! JHAGRA a Dag CHAMKAN"'I "' "' ! k REGAI PESHAWAR Laram "'BAZAR KALAN TARNAB FARM k "' "' ! Pakha Ghulam "' RASHID ABAD (NCB) h ! ! ! ! ! ! ! t ISLAMIA COLLEGE HOSPITAL, PESHAWZANANA HOSPITAL, PESHAWAR Wad Paga t ! PHANDOO PAYAN u "' "' "' Regi Palosi Lala n ! Urban Ar! ! ! LANDI ARBAB k Map Doc Name: "' h iMMAP_Peshawar District Reference -

Forestry in the Princely State of Swat and Kalam (North-West Pakistan)
Forestry in the Princely State of Swat and Kalam (North-West Pakistan) A Historical Perspective on Norms and Practices IP6 Working Paper No.6 Sultan-i-Rome, Ph.D. 2005 Forestry in the Princely State of Swat and Kalam (North-West Pakistan) A Historical Perspective on Norms and Practices IP6 Working Paper No.6 Sultan-i-Rome, Ph.D. 2005 The Swiss National Centre of Competence in Research (NCCR) North-South is based on a network of partnerships with research institutions in the South and East, focusing on the analysis and mitigation of syndromes of global change and globalisation. Its sub-group named IP6 focuses on institutional change and livelihood strategies: State policies as well as other regional and international institutions – which are exposed to and embedded in national economies and processes of globalisation and global change – have an impact on local people's livelihood practices and strategies as well as on institutions developed by the people themselves. On the other hand, these institutionally shaped livelihood activities have an impact on livelihood outcomes and the sustainability of resource use. Understanding how the micro- and macro-levels of this institutional context interact is of vital importance for developing sustainable local natural resource management as well as supporting local livelihoods. For an update of IP6 activities see http://www.nccr-north-south.unibe.ch (>Individual Projects > IP6) The IP6 Working Paper Series presents preliminary research emerging from IP6 for discussion and critical comment. Author Sultan-i-Rome, Ph.D. Village & Post Office Hazara, Tahsil Kabal, Swat–19201, Pakistan e-mail: [email protected] Distribution A Downloadable pdf version is availale at www.nccr- north-south.unibe.ch (-> publications) Cover Photo The Swat Valley with Mingawara, and Upper Swat in the background (photo Urs Geiser) All rights reserved with the author. -

3. Peshawar City District
Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized " ·.'·t i: ::•<< ·,c· " ·i: i .• : ;·c, ·ji;i:'f~?W B~nk · 'Cities l\lli~~e c i.fi~·{wL~•h•au·i·· s:i·u·ffi:~:;,' ·'·,;:,,········~ :~·~ ·--~ ,, ~ -1- •• !~·~r· 1: Acronyms and Abbreviations ACR Annual Confidential Report LG Local Government ADS Asian Development Bank LG&RD Local Government & Rural Development ADOs Assistant District Officers LGC Local Government Commission ADP Annual Development Program- LGO Local Government Ordinance AE Agriculture Extension LRG Local Revenue Generation AOs Agriculture Officers LS&DD Livestock & Dairy Development ATI Agriculture Training Institute MIS Management Information System SHU Basic Health Unit MC Monitoring Committee BOS Bureau of Statistics MCP Municipal Corporation Peshawar BPS Basic Pay Scale M&R Maintenance and Rehabilitation CAP City Assistance Plan MoUs Memorandum of Understandings CBO Community Based Organization MVT Motor Vehicle Tax CCP Capital City Police NFC National Finance Commission CDMD City Development and Municipal Department NGO Non-Government Organization CDS City Development Strategy NWFP Northwest Frontier Province cso Civil Society Organization OFWM On-Farm Water Management CrPC Criminal Procedure Code O&M Operation & Maintenance CNG Compressed Natural Gas OZT Octroi and Zila Tax DC District Council PCD Peshawar City District DCO District Coordination Officer PDA Peshawar Development Authority DCC District Coordination Committee PEP Primary Education Project -

Curriculum Vitae IMRAN AHMAD
Curriculum Vitae IMRAN AHMAD DOUBLE GOLD MEDALIST M.PHIL (GEOLOGY) Postal Address: Assistant Professor, Department of Geology, University of Malakand, Chakdara, Dir (Lower), (Khyber Pakhtunkhwa), Pakistan Cell phone: +92-333-8959643 E-mail: [email protected] QUALIFICATION: Degree Subject Year Percentage Position in class/batch Institute/Board PhD Geology 2017 In Progress Quaid-I-Azam University, Islamabad. M. Phil Geology 2016 80% First Position in Batch Quaid-I-Azam University, Islamabad. BS/M.Sc. Geology 2008 80.62% First Position in Batch University of Peshawar H.S.S.C Pre-Engineering 2004 75.09% First Position in class B.I.S.E Swat S.S.C Science Group 2002 82.12% First Position in class B.I.S.E Swat DISTINCTIONS: Award Awarded by Year On account of Gold Medal University of Peshawar 2008 Over all first position in 4-years BS/M.Sc Geology Presidential Award of Pakistan Government of Pakistan 2008 On securing highest score in all (Nominee) the universities of Khyber Pakhtunkhwa Province, Pakistan Position Holder Certificate Department of Geology, 2008 Obtained highest marks University of Peshawar Merit Certificate University of Peshawar 2008 Obtained 86% marks in my field of specialization (Final year in Structural Geology) Position Holder Certificate Govt. Degree College, 2004 First position in the college Mingora Swat (Pre-Engineering Group) Position Holder Certificate Madyan Public School, 2002 First position in the School Madyan Swat (Science Group) Talent Certificate FLORIDA STATE 2010 Field experience UNIVERSITY, USA Talent Certificate EDINBURGH 2010 Field experience UNIVERSITY, UK Gold Medal/Chancellor Medal Quaid-I-Azam 2016 First position in class/batch University, Islamabad with 80% marks. -

1 Annexure - D Names of Village / Neighbourhood Councils Alongwith Seats Detail of Khyber Pakhtunkhwa
1 Annexure - D Names of Village / Neighbourhood Councils alongwith seats detail of Khyber Pakhtunkhwa No. of General Seats in No. of Seats in VC/NC (Categories) Names of S. Names of Tehsil Councils No falling in each Neighbourhood Village N/Hood Total Col Peasants/Work S. No. Village Councils (VC) S. No. Women Youth Minority . district Council Councils (NC) Councils Councils 7+8 ers 1 2 3 4 5 6 7 8 9 10 11 12 13 Abbottabad District Council 1 1 Dalola-I 1 Malik Pura Urban-I 7 7 14 4 2 2 2 2 Dalola-II 2 Malik Pura Urban-II 7 7 14 4 2 2 2 3 Dabban-I 3 Malik Pura Urban-III 5 8 13 4 2 2 2 4 Dabban-II 4 Central Urban-I 7 7 14 4 2 2 2 5 Boi-I 5 Central Urban-II 7 7 14 4 2 2 2 6 Boi-II 6 Central Urban-III 7 7 14 4 2 2 2 7 Sambli Dheri 7 Khola Kehal 7 7 14 4 2 2 2 8 Bandi Pahar 8 Upper Kehal 5 7 12 4 2 2 2 9 Upper Kukmang 9 Kehal 5 8 13 4 2 2 2 10 Central Kukmang 10 Nawa Sher Urban 5 10 15 4 2 2 2 11 Kukmang 11 Nawansher Dhodial 6 10 16 4 2 2 2 12 Pattan Khurd 5 5 2 1 1 1 13 Nambal-I 5 5 2 1 1 1 14 Nambal-II 6 6 2 1 1 1 Abbottabad 15 Majuhan-I 7 7 2 1 1 1 16 Majuhan-II 6 6 2 1 1 1 17 Pattan Kalan-I 5 5 2 1 1 1 18 Pattan Kalan-II 6 6 2 1 1 1 19 Pattan Kalan-III 6 6 2 1 1 1 20 Sialkot 6 6 2 1 1 1 21 Bandi Chamiali 6 6 2 1 1 1 22 Bakot-I 7 7 2 1 1 1 23 Bakot-II 6 6 2 1 1 1 24 Bakot-III 6 6 2 1 1 1 25 Moolia-I 6 6 2 1 1 1 26 Moolia-II 6 6 2 1 1 1 1 Abbottabad No. -
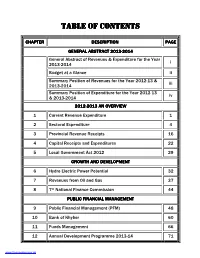
3 Table of Contents
TABLE OF CONTENTS TABLE OF CONTENTS CHAPTER DESCRIPTION PAGE GENERAL ABSTRACT 20132013----20142014 General Abstract of Revenue s & Expenditure for the Year i 2013-2014 Budget at a Glance ii Summary Position of Revenues for the Year 2012 -13 & iii 2013-2014 Summary Position of Expenditure for the Year 2012 -13 iv & 2013-2014 20122012----20132013 AN OVERVIEW 1 Current Revenue Expenditure 1 2 Sectoral Expenditure 4 3 Provincial Revenue Receipts 16 4 Capital Receipts and Expenditures 22 5 Local Government Act 2012 29 GROWTH AND DEVELOPDEVELOPMENTMENT 6 Hydro Electric Power Potential 32 7 Revenues from Oil and Gas 37 8 7th National Finance Commission 44 PUBLIC FINANCIAL MANAGEMENT 9 Public Financial Management (PFM) 48 10 Bank of Khyber 60 11 Funds Management 66 12 Annual Development Programme 2013-14 71 www.financekpp.gov.pk TABLE OF CONTENTS TABLE OF CONTENTS ANNEXURES DESCRIPTION PAGE I CDL Liabilities as on 01-07-2013 109 II Detail of Premature Debt Retirement 110 III Foreign Exchange Loan Liabilities as on 01-07-2013 111 Disbursement of Loans in R/o of Ongoing Foreign IV 113 Projects Share as on 30-06-2013 V General Revenue Receipts 114 VI Current Revenue Expenditure 117 Development Budget by Sector for the Year 2012-13 VII 119 & 2013-14 Annual Development Programme Since 1971-72 on VIII 124 ward Growth in Current Revenue Budget & Revenue IX 125 Receipts Since 1974-75 on ward Grant Wise General Abstract of Current Budget for the X 127 Year 2013-14 www.financekpp.gov.pk FOREWORD White Paper reflects the Provincial Government’s policies and presents an overview of the financial position of the Provincial Government. -

I Was Born on 2 March 1929 in Charsadda, Peshawar District in Khyber Pakhtoonkhwa Province of Pakistan
I was born on 2 March 1929 in Charsadda, Peshawar district in Khyber Pakhtoonkhwa province of Pakistan. I obtained a medical degree from King Edward Medical College, Lahore, Punjab in 1952. I had a year of house job in West medical ward with Professor Aslam Pirzada. I also spent six months training in tuberculosis ward in Lady Reading Hospital, Peshawar with Dr Ali Gauhar Khan. I went to Edinburg in 1956 to work with Professor J.H. Gaddum. He had found 5-Hydroxy tryptamine in dogs' brains. He also found that the effect of this substance on smooth muscles was antagonized by LSD, which is hallucinogenic. Dr R.B. Barlow, who was working with Professor Gaddum had synthesized a number of analogues of 5-Hydroxy tryptamine and tryptamine. I was assigned to test these compounds on smooth muscles on rat uterus and guinae pig ileum. I participated in most of the six monthly meetings of the British Pharmacological Society in various cities in the UK and presented my results and also submitted papers to the British Journal of Pharmacology. My final theses of Ph.D. in Pharmacology in 1959 was entitled "drugs modifying the action of 5-Hydroxy tryptamine on smooth muscles". A copy of this theses has been kept in the library of Jinah Postgraduate Medical Center in Karachi. On return to Pakistan in 1959, I was posted as Assistant Professor of Pharmacology at the King Edward Medical College, Lahore. In 1961 I was posted at Khyber Medical College, in Peshawar as professor of pharmacology. Two years later, I was transferred to Karachi, at Jinah postgraduate Medical Center, Basic Medical Sciences Institute which was created in collaboration with the governments of USA and Pakistan. -

Electoral Politics in Nwfp. 1988-1999
i ELECTORAL POLITICS IN NWFP. 1988-1999 Submitted by MUHAMMAD SHAKEEL AHMAD Supervised by Dr. NAUREEN TALHA NATIONAL INSTITUTE OF PAKISTAN STUDIES QUAID-I-AZAM UNIVERSITY ISLAMABAD 2010 ii ELECTORAL POLITICS IN NWFP. 1988-1999 A dissertation submitted to the National Institute of Pakistan Studies, Quaid-I-Azam University Islamabad (Pakistan) in partial fulfillment of the requirement for the degree of Doctor of Philosophy in Pakistan Studies. By MUHAMMAD SHAKEEL AHMAD NATIONAL INSTITUTE OF PAKISTAN STUDIES QUAID-I-AZAM UNIVERSITY ISLAMABAD 2010 iii DECLARATION I hereby declare that this thesis is the result of my individual research, and that it has not been submitted concurrently to any other university for any other degree. Muhammad Shakeel Ahmad iv CONTENTS S. NO TITLES PAGE NO 1 LIST OF TABLES, FIGURES AND DIAGRAMS vii 2 ACRONYMS xi 3 GLOSSARY xii 4 ACKNOWLEDGEMENT xiv 5 ABSTRACT xv 6 INTRODUCTION xvi Aims and Objective of the Study xvii Research Question-Hypothesis and Models xviii Significance of the Problem xix Review of Literature xxi Research Methodology xxxiii Summary of Chapters PART-1 THEORIES AND CONTEXTS 7 CHAPTER-1: THEORETICAL FRAMEWORK OF 1-32 ELECTORAL POLITICS 1.1 Introduction 1 1.2 Electoral Politics and the political organization 7 1.3 Electoral politics and political participation 14 1.4 Militaricracy to Electocracy 19 1.5 Impact of elections on legislature 23 1.6 Basic practices in Electoral Politics 26 1.7 Reforms in Electoral Politics 28 1.8 Conclusions 30 8 CHAPTER-2: NWFP’S ELECTORAL GEOGRAPHY 33-61 2.1 Introduction 33 2.2 Central NWFP 37 2.2.1 Geography and Population 38 2.2.2 Agriculture and canal system 38 2.2.3 Economy 41 2.2.4 Politics 43 2.3.1 Northern NWFP 46 2.3.2 Geography and Population 46 2.3.3 Economy 48 2.3.4 Politics 49 2.4.1 Southern NWFP 51 2.4.2 Geography and Population 52 2.4.3 Economy 52 2.4.4 Politics 53 2.5.1 North-Eastern NWFP 55 2.5.2 Economy 56 2.5.3 Politics 57 2.6 Conclusions 60 9 CHAPTER-3: ELECTORAL HISTORY OF NWFP 62-89 3. -
Governing Natural Resources and the Processes and Institutions That
Environmental in Pakistan Governing Natural Resources and the Processes and 02 Institutions that Affect Them No r t h - West Volume 2 Legislation Frontier Province 02 En v i r o n m e n t a l Governing Natural Resources and the Processes and Law in Institutions that Affect Them Pak i s t a n N.W.F.P Introduction to the Series 02 Foreword 04 Acknowledgements 06 01 Executive Summary 08 02 Methodology 12 03 Hierarchy of Legal Instruments 14 3.1 Constitution of the Islamic Republic of Pakistan 1973 15 3.2 Legislative Acts 15 3.3 Ordinances 15 3.4 Rules and Regulations 16 3.5 Orders 16 3.6 Notifications 16 3.7 Laws of West Pakistan 16 Introduction of Laws 4. Governance 18 5. Laws and Judicial Decisions Governing Natural Resources and Natural Resource Management 24 6. Laws and Judicial Decisions Governing Processes and Institutions that affect Natural Resources Management 42 7. Summary and Conclusions 60 01 Introduction to the Series 06 02 Foreword 08 03 Executive Summary 10 04 Governance 14 4.1 Constitution of Pakistan (Refer to the Federal Review) 4.3.2.1 NWFP Local Government Ordinance 2001 15 4.3.2.2 NWFP Amendment of laws Ordinance 2001 130 05 Laws and Judicial Decisions Governing Natural Resources and Natural Resource Management 134 5.1.1 Land Tenure 135 5.1.1.1 NWFP Gomal Zam Project (Control and Prevention of Speculation in Land) Ordinance 2001 135 5.1.1.2 Land Reforms (North–West Frontier Province Amendment) Act 1972 142 5.1.1.3 NWFP Land Reforms Rules 1972 147 5.1.1.4 West Pakistan Land Utilization Ordinance 1959 153 5.1.1.5 West Pakistan -

Contingency Plan Tingency Plan
CONTINGENCY PLAN MONSOON 2012 Provincial Disaster Management Authority Khyber Pakhtunkhwa Monsoon Contingency Plan 2012- Khyber Pakhtunkhwa CONTINGENCY PLAN MONSOON 2012 PROVINCIAL DISASTER MANAGEMENT AUTHORITY KHYBER PAKHTUNKHWA June 2012 2 Monsoon Contingency Plan 2012- Khyber Pakhtunkhwa 3 Monsoon Contingency Plan 2012- Khyber Pakhtunkhwa Prepared by Muhammad Bakhtiar Khan, Deputy Directotr (Relief) under the guidance of Zulfiqar Ali Shah, Director (Relief & Operations), supervised by Shahzad Khan Bangash, Director General, PDMA and Rashid Ahmad, Secretary, Relief, Rehabilitation & Settlement Department, Khyber Pakhtunkhwa. 4 Monsoon Contingency Plan 2012- Khyber Pakhtunkhwa Table of Contents Executive Summary .......................................................................................................................... 7 Chapter-1........................................................................................................................................ 10 Monsoon Contingency Plan 2012.................................................................................................... 10 1.1 An Overview..........................................................................................................................10 1.2 Contingency Plan for Monsoon 2012....................................................................................11 1.3 The Floods - 2010..................................................................................................................12 1.4 Response to Flood 2010........................................................................................................14