Annandale and Eskdale Locality Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Report on the Current Position of Poverty and Deprivation in Dumfries and Galloway 2020
Dumfries and Galloway Council Report on the current position of Poverty and Deprivation in Dumfries and Galloway 2020 3 December 2020 1 Contents 1. Introduction 1 2. National Context 2 3. Analysis by the Geographies 5 3.1 Dumfries and Galloway – Geography and Population 5 3.2 Geographies Used for Analysis of Poverty and Deprivation Data 6 4. Overview of Poverty in Dumfries and Galloway 10 4.1 Comparisons with the Crichton Institute Report and Trends over Time 13 5. Poverty at the Local Level 16 5.1 Digital Connectivity 17 5.2 Education and Skills 23 5.3 Employment 29 5.4 Fuel Poverty 44 5.5 Food Poverty 50 5.6 Health and Wellbeing 54 5.7 Housing 57 5.8 Income 67 5.9 Travel and Access to Services 75 5.10 Financial Inclusion 82 5.11 Child Poverty 85 6. Poverty and Protected Characteristics 88 6.1 Age 88 6.2 Disability 91 6.3 Gender Reassignment 93 6.4 Marriage and Civil Partnership 93 6.5 Pregnancy and Maternity 93 6.6 Race 93 6.7 Religion or Belief 101 6.8 Sex 101 6.9 Sexual Orientation 104 6.10 Veterans 105 7. Impact of COVID-19 Pandemic on Poverty in Scotland 107 8. Summary and Conclusions 110 8.1 Overview of Poverty in Dumfries and Galloway 110 8.2 Digital Connectivity 110 8.3 Education and Skills 111 8.4 Employment 111 8.5 Fuel Poverty 112 8.6 Food Poverty 112 8.7 Health and Wellbeing 113 8.8 Housing 113 8.9 Income 113 8.10 Travel and Access to Services 114 8.11 Financial Inclusion 114 8.12 Child Poverty 114 8.13 Change Since 2016 115 8.14 Poverty and Protected Characteristics 116 Appendix 1 – Datazones 117 2 1. -

Dryburgh, Mr A
Title: Mr Forename: Archie Surname: Dryburgh Representing: Organisation Organisation (if applicable): Annandale East and Eskdale Ward Councillor for Dumfries and Galloway Council Email: What additional details do you want to keep confidential?: No If you want part of your response kept confidential, which parts?: Ofcom may publish a response summary: Yes I confirm that I have read the declaration: Yes Additional comments: Question 1: Do you agree that the existing obligations on Channel 3 and Channel 5 licensees in respect of national and international news and current affairs, original productions, and Out of London productions should be maintained at their current levels? If not, what levels do you consider appropriate, and why?: No, belive that border area should have some more coverage due to the region in which itv border originally covered Question 2: Do you agree with ITV?s proposals for changes to its regional news arrangements in England, including an increase in the number of news regions in order to provide a more localised service, coupled with a reduction in overall news minutage? : Yes Question 3: Do you agree with UTV?s proposal for non-news obligations should be reduced to 90 minutes a week? If not, what alternative would you propose and why?: n/a Question 4: Do you agree with the proposals by STV to maintain overall minutage for regional content in the northern and central licence areas of Scotland at 5 hours 30 minutes a week, as detailed in Annex 3? If not, what alternative would you propose, and why? : n/a Question -
The Norse Influence on Celtic Scotland Published by James Maclehose and Sons, Glasgow
i^ttiin •••7 * tuwn 1 1 ,1 vir tiiTiv^Vv5*^M òlo^l^!^^ '^- - /f^K$ , yt A"-^^^^- /^AO. "-'no.-' iiuUcotettt>tnc -DOcholiiunc THE NORSE INFLUENCE ON CELTIC SCOTLAND PUBLISHED BY JAMES MACLEHOSE AND SONS, GLASGOW, inblishcre to the anibersitg. MACMILLAN AND CO., LTD., LONDON. New York, • • The Macmillan Co. Toronto, • - • The Mactnillan Co. of Canada. London, • . - Simpkin, Hamilton and Co. Cambridse, • Bowes and Bowes. Edinburgh, • • Douglas and Foults. Sydney, • • Angus and Robertson. THE NORSE INFLUENCE ON CELTIC SCOTLAND BY GEORGE HENDERSON M.A. (Edin.), B.Litt. (Jesus Coll., Oxon.), Ph.D. (Vienna) KELLY-MACCALLUM LECTURER IN CELTIC, UNIVERSITY OF GLASGOW EXAMINER IN SCOTTISH GADHELIC, UNIVERSITY OF LONDON GLASGOW JAMES MACLEHOSE AND SONS PUBLISHERS TO THE UNIVERSITY I9IO Is buaine focal no toic an t-saoghail. A word is 7nore lasting than the world's wealth. ' ' Gadhelic Proverb. Lochlannaich is ànnuinn iad. Norsemen and heroes they. ' Book of the Dean of Lismore. Lochlannaich thi'eun Toiseach bhiir sgéil Sliochd solta ofrettmh Mhamiis. Of Norsemen bold Of doughty mould Your line of oldfrom Magnus. '' AIairi inghean Alasdair Ruaidh. PREFACE Since ever dwellers on the Continent were first able to navigate the ocean, the isles of Great Britain and Ireland must have been objects which excited their supreme interest. To this we owe in part the com- ing of our own early ancestors to these isles. But while we have histories which inform us of the several historic invasions, they all seem to me to belittle far too much the influence of the Norse Invasions in particular. This error I would fain correct, so far as regards Celtic Scotland. -

No. Forename Surname Club / Organisation Distance 123 Stuart
No. Forename Surname Club / Organisation Distance 123 Stuart ADAMSON Stewartry Wheelers 100 miles 147 Charlie ALEXANDER Hillhead Raiders CC 100 miles 148 Matt ANDERSON None 62miles 51 John ANDREW Dumfries CC 100 miles 266 David ARTHUR Athelite Triathlon Club 100 miles 12 Steven ASHWORTH None 100 miles 149 Alan AULD Strathclyde Police 100 miles 150 Simon BAIN Glasgow Green Cycling Club 100 miles 139 Andrew BAIRD West Lothian Clarion 100 miles 151 Stuart BARR None 100 miles 102 Mary BARRETT SSCC 100 miles 153 Stewart BECK None 100 miles 63 David BELDING Walkers CC 100 miles 154 Steven BELL None 100 miles 155 Ian BELL None 100 miles 27 Michael BETHWAITE Honister 92 100 miles 285 Andy Blackett None 62miles 70 Gordon BONALLO West Lothian Clarion 100 miles 157 Leon BOND Honister 92 100 miles 158 Alan BOWIE None 62miles 159 Allan BOYD None 100 miles 160 Brian BOYD None 62miles 161 Raymond BOYD None 100 miles 162 Hugh BOYLE None 100 miles 8 Anna BROOKS Morningside medical practice 62miles 163 Chris BROWN None 100 miles 164 Stephen BROWN None 100 miles 165 Ian BROWN None 100 miles 304 Drew BRUNTON None 100 miles 250 Dawn BUCHANAN Athelite Triathlon Club 100 miles 168 Pat BURNS None 100 miles 169 Kevin BURNS None 100 miles 170 Peter Burtwistle Royal Albert Cycling Club 100 miles 92 Lorne CALLAGHAN West Lothian Clarion 100 miles 20 Ewan CAMPBELL ??? 172 Barry CAMPBELL None 100 miles 174 Iain CAMPBELL None 100 miles 79 Jacqui CARRICK HERVELO 62miles 80 Nigel CARRICK Kelso Wheelers 100 miles 176 Derek CARRIGAN None 100 miles 179 Malcolm CARSON None -
The Lowland Clearances and Improvement in Scotland
University of Massachusetts Amherst ScholarWorks@UMass Amherst Doctoral Dissertations Dissertations and Theses August 2015 Uncovering and Recovering Cleared Galloway: The Lowland Clearances and Improvement in Scotland Christine B. Anderson University of Massachusetts Amherst Follow this and additional works at: https://scholarworks.umass.edu/dissertations_2 Part of the Archaeological Anthropology Commons Recommended Citation Anderson, Christine B., "Uncovering and Recovering Cleared Galloway: The Lowland Clearances and Improvement in Scotland" (2015). Doctoral Dissertations. 342. https://doi.org/10.7275/6944753.0 https://scholarworks.umass.edu/dissertations_2/342 This Open Access Dissertation is brought to you for free and open access by the Dissertations and Theses at ScholarWorks@UMass Amherst. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of ScholarWorks@UMass Amherst. For more information, please contact [email protected]. Uncovering and Recovering Cleared Galloway: The Lowland Clearances and Improvement in Scotland A dissertation presented by CHRISTINE BROUGHTON ANDERSON Submitted to the Graduate School of the University of Massachusetts Amherst in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY May 2015 Anthropology ©Copyright by Christine Broughton Anderson 2015 All Rights Reserved Uncovering and Recovering Cleared Galloway: The Lowland Clearances and Improvement in Scotland A Dissertation Presented By Christine Broughton Anderson Approved as to style and content by: H Martin Wobst, Chair Elizabeth Krause. Member Amy Gazin‐Schwartz, Member Robert Paynter, Member David Glassberg, Member Thomas Leatherman, Department Head, Anthropology DEDICATION To my parents. ACKNOWLEDGEMENTS It is with a sense of melancholy that I write my acknowledgements. Neither my mother nor my father will get to celebrate this accomplishment. -

Community Bulletin
Happy Community Passover EDITION 63 #Support DG Thursday 1 April 2021 Dock Park in Dumfries is springing into bloom Inside Admirable Crichton Take Burns Rebranded Be Kind Connect Notice Support Give Diamond Geezer www.dumgal.gov.uk/supportdg Tel 030 33 33 3000 Welcome to @dgcouncil @DumfriesGallowayCouncil Community Email updates dumgal.gov.uk/newsletters Cllr Elaine Murray Cllr Rob Davidson Council Leader Depute Leader Wow! It’s Easter weekend and the sun is shining. After what feels like a very long year, it seems as if we’re Recycling Rollout turning a corner. The Council’s recycling roll out continues with nearly all households in the Stewartry area receiving two new Declining numbers of new Covid cases in our region recycling bins or sacks. and great progress in the rollout of vaccinations mean that we have cause for optimism. However, we mustn’t let our guard down. We must continue to defend ourselves against a still deadly virus and do all that we can to keep infection rates low. Everyone should continue to follow the FACTS guidance. Anyone with Covid-19 symptoms should self-isolate with their household and book a test at a testing unit. Spring is a time for renewal and new beginnings. This First collections of this new service begin next week: issue of Community highlights a number of youth check the calendar that came with the bins/sacks. initiatives and projects that give a taster of what can be A dedicated waste communications hub will address any achieved once Covid restrictions are eased. The future is queries regarding missed deliveries and can be contacted indeed bright. -

Health and Social Care NITHSDALE LOCALITY REPORT March 2021
Dumfries and Galloway Integration Joint Board Health and Social Care NITHSDALE LOCALITY REPORT March 2021 Version: DRAFT March 2021 1. General Manager’s Introduction 1.1 The COVID-19 Pandemic The past year has presented unprecedented challenges for health and social care across Dumfries and Galloway. The first 2 cases of COVID-19 in the UK were confirmed by 31 January 2020. The first positive cases in Dumfries and Galloway were identified on 16 March 2020. Following direction from the Scottish Government, in March 2020 Dumfries and Galloway Health and Social Care Partnership started their emergency response to the pandemic. Hospital wards were emptied and some cottage hospitals temporarily closed. Many planned services were stopped whilst others changed their delivery model. Many staff were redeployed to assist with anticipated high levels of demand across the Partnership. There were many issues that had to be addressed including: the supply and distribution of Personal Protective Equipment (PPE) across the Health and Social Care system over 500 people’s regular care and support ‘packages’ were readjusted to respond to the needs presented by COVID-19 our relationships with care homes changed significantly we quickly kitted out a site that could be used as a temporary cottage hospital in Dumfries During the period of June to October 2020, the Partnership focused on adapting services to reflect the heightened infection prevention and control measures needed to combat COVID-19 and rapidly expanding COVID-19 testing capacity across the region. We rolled out training and technology to enable many more video and telephone consultations. We had to rethink how people could access our premises, with additional cleaning and social distancing to keep people safe. -

Hotspots of Farm Business Diversification in Scotland
Hotspots of farm business diversification in Scotland Jonathan Hopkins1, Carla Barlagne1, Lee-Ann Sutherland1, Keith Matthews2, Andrew Barnes3, Luiza Toma3 1Social, Economic and Geographical Sciences Group, The James Hutton Institute, Aberdeen 2Information and Computational Sciences Group, The James Hutton Institute, Aberdeen 3Land Economy and Environment Group, Scotland’s Rural College, Edinburgh On-farm wind turbine in Aberdeenshire Purpose of document This note forms an output of Research Deliverable 2.4.2 ‘How Rural Economies Can Adapt to Key External Drivers’, undertaken as part of the RESAS Strategic Research Programme (2016-2021). This work has helped to “…identify indicators of innovation and diversification”1. This note presents an analysis of questionnaire and public datasets to identify areas in Scotland where there is evidence of high levels of farm diversification activity (‘farm diversification hotspots’). The note describes the uptake of non-farming enterprises and income diversification in Scotland, focusing in particular on renewable energy projects and agri-tourism development. Key findings • Levels of diversification are high in the rural areas north of central Scotland: Argyll, Stirling, Perth and Kinross, Fife, and Angus. • Lanarkshire and Aberdeenshire have a high concentration of on-farm renewable energy schemes, in particular onshore wind projects. • Different types of renewable energy technology tend to cluster together. In addition to onshore wind schemes (found frequently in central and eastern Scotland), hydro developments are concentrated in mountainous regions and near the west coast, and solar projects have been developed in the sunnier east (e.g. Fife, Angus). • Evidence suggests that farm diversification into agri-tourism has taken place in accessible scenic regions and in areas close to population centres. -

Dumfries and Galloway Practitioners Hub Newsletter
Dumfries and Galloway Practitioners Newsletter Hub Issue 16 April 2015 Welcome to the April edition of the Dumfries & Galloway Practitioners Hub USEFUL newsletter. INFORMATION You can follow our Council’s Welfare Reform reports here. Increased use of UNIVERSAL CREDIT : INFORMATION AND SUPPORT AVAILABLE real time information Universal Credit is coming to Dumfries and Galloway this month Better data sharing Universal Credit (UC) will go live in Dumfries and Galloway from 27 April 2015 between HMRC and but this is initially a very small scale roll out. The maximum uptake is DWP to reduce estimated at 1,500 claimants by April 2016. fraud and error in the benefits system NEW - “Universal Credit guidance” for practitioners was announced in This factsheet pulls together all the main things that practitioners should need the March budget to know Universal Credit in one document - what to do and what key help is statement. available in Dumfries and Galloway. It covers managing queries, making a claim, getting paid The Cumulative knowing if someone is on Universal Credit Impact of Welfare rent payments and help to pay the rent, changes in circumstances Reform on support available - digital support, personal budgeting, alternative payment Households in arrangements, having and using a bank account Scotland Council Tax and Discretionary Housing Payments sanctions and appeals Published on the 2 March 2015, this Click here to download it. research was commissioned and NEW – “Organisations that can help you” for benefit recipients published by the Scottish Parliament’s We have created directories which cover Dumfries and Galloway. They are Welfare Reform targeted primarily at benefit recipients but may be useful to anyone. -

Dumfries and Galloway War Memorials
Annandale and Eskdale War Memorials Annan Memorial High Street, Annan Dumfries and Galloway DG12 6AJ Square base surmounted by pedestal and Highland Soldier standing at ease with rifle. Applegarth and Sibbaldbie Parishoners Memorial Applegarth Church Applegarth Dumfries and Galloway DG11 1SX Sandstone. Two stepped square base surmounted by two stepped plinth, tapering shaft and Latin cross. Brydekirk Memorial Brydekirk Parish Church Brydekirk Dumfries and Galloway DG12 5ND Two stepped base surmounted by square pedestal and small cross. Surrounded by wrought iron railings. Canonbie Memorial B7201 Canonbie Dumfries & Galloway DG14 0UX Tapered base surmounted by pedestal and figure of a serviceman with head bowed, rifle over shoulder. Cummertrees Memorial Cummertrees Parish Church Cummertrees Dumfries & Galloway DG1 4NP Wooden lych-gate with tiled roof mounted onto a stone base. Inscription over entrance. Dalton Memorial Dalton Parish Church Dalton Dumfries & Galloway DG11 1DS Tapered square plinth surmounted by tapered shaft and Celtic cross. Dornock Memorial B721 Eastriggs Dumfries & Galloway DG12 6SY White marble. Three stepped base surmounted by double plinth, tapering pedestal and column which narrows at the top. Ecclefechan, Hoddom Memorial Ecclefechan Dumfries & Galloway DG11 3BY Granite. Tapered stone base surmounted by two stepped granite base, pedestal and obelisk. Surrounded by wrought iron railings. Eskdalemuir Memorial Eskdalemuir Parish Church B709 Eskdalemuir Dumfries & Galloway DG13 0QH Three stepped square stone base surmounted by rough hewn stone pedestal and tapered top. Ewes Memorial Ewes Parish Church A7 Ewes Langholm Dumfries & Galloway DG13 0HJ White marble. Square base surmounted by plinth and Latin cross mounted on a rough hewn base. Gretna Green Memorial Gretna Green Dumfries & Galloway DG16 5DU Granite. -
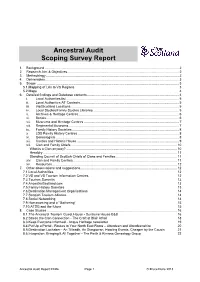
Ancestral Audit Scoping Survey Report
Ancestral Audit Scoping Survey Report 1. Background ................................................................................................................................................ 2 2. Research Aim & Objectives ........................................................................................................................ 2 3. Methodology ............................................................................................................................................... 2 4. Deliverables ................................................................................................................................................ 3 5. Scope ......................................................................................................................................................... 3 5.1.Mapping of LAs to VS Regions 3 5.2.Maps 4 6. Detailed findings and Database contents ................................................................................................... 4 i. Local Authorities list ......................................................................................................................... 5 ii. Local Authorities AT Contacts. ......................................................................................................... 5 iii. VisitScotland Locations .................................................................................................................... 5 iv. Local Studies/Family Studies Libraries. .......................................................................................... -

ROMAN COINS FOUND in SCOTLAND, 1951-60 by ANN
ROMAN COINS FOUND IN SCOTLAND, 1951-60 by ANN . ROBERTSONES , M.A., F.M.A., F.S.A., F.S.A.SGOT. THE late Sir George Macdonald published four lists of Roman coins found in Scot- land, which brought the record of such finds up to igsg.1 A subsequent list, pub- lishe myselfy db , included Roman coins foun Scotlann di d between 193 I95O.d 9an 2 e followinTh g list includes bot Romae hth n coins foun Scotlann di d durine gth decade 1951-60 alsd o,an those coins which were found earlier t aboubu , t whicw hne information has come to light in recent years. The list has been divided into four parts: ) FIND(I . SA FROM ROMA NANTONINE SITETH N SO E WALL (II) FINDS FROM ROMA ANTONINE TH NN O SITE T E SWALNO L . FINDB S FROM NATIVE SITES . ISOLATEC D FINDS WIT RECORDEO HN D ASSOCIATIONS D. HOARDS The finds within each of the above groups have been arranged according to counties, for the convenience of those collating material from a particular area. Coin references have been given bot o Cohent h , Description historique des monnaies frappees sous Fempire romain (2nd ed., relevane 1880-92)th o t d t volumean , f Matso - tingly and Sydenham, Roman Imperial Coinage (1923-51), if these have already been published presene Th . t locatio coia f no find, where known alss ha ,o been noted. Grateful acknowledgment must once again be made of the cooperation and kindness of the countless informants who not only supplied details of the circum- stances of discovery, but who also made it possible for me to examine and identify almost every one of the coins myself.