Web Annex B: Health Professionals' Mobile Digital Education
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bloomsbury Conservation Area Appraisal and Management Strategy
Bloomsbury Conservation Area Appraisal and Management Strategy Adopted 18 April 2011 i) CONTENTS PART 1: CONSERVATION AREA APPRAISAL 1.0 INTRODUCTION ........................................................................................................................ 0 Purpose of the Appraisal ............................................................................................................ 2 Designation................................................................................................................................. 3 2.0 PLANNING POLICY CONTEXT ................................................................................................ 4 3.0 SUMMARY OF SPECIAL INTEREST........................................................................................ 5 Context and Evolution................................................................................................................ 5 Spatial Character and Views ...................................................................................................... 6 Building Typology and Form....................................................................................................... 8 Prevalent and Traditional Building Materials ............................................................................ 10 Characteristic Details................................................................................................................ 10 Landscape and Public Realm.................................................................................................. -

CAMDEN STREET NAMES and Their Origins
CAMDEN STREET NAMES and their origins © David A. Hayes and Camden History Society, 2020 Introduction Listed alphabetically are In 1853, in London as a whole, there were o all present-day street names in, or partly 25 Albert Streets, 25 Victoria, 37 King, 27 Queen, within, the London Borough of Camden 22 Princes, 17 Duke, 34 York and 23 Gloucester (created in 1965); Streets; not to mention the countless similarly named Places, Roads, Squares, Terraces, Lanes, o abolished names of streets, terraces, Walks, Courts, Alleys, Mews, Yards, Rents, Rows, alleyways, courts, yards and mews, which Gardens and Buildings. have existed since c.1800 in the former boroughs of Hampstead, Holborn and St Encouraged by the General Post Office, a street Pancras (formed in 1900) or the civil renaming scheme was started in 1857 by the parishes they replaced; newly-formed Metropolitan Board of Works o some named footpaths. (MBW), and administered by its ‘Street Nomenclature Office’. The project was continued Under each heading, extant street names are after 1889 under its successor body, the London itemised first, in bold face. These are followed, in County Council (LCC), with a final spate of name normal type, by names superseded through changes in 1936-39. renaming, and those of wholly vanished streets. Key to symbols used: The naming of streets → renamed as …, with the new name ← renamed from …, with the old Early street names would be chosen by the name and year of renaming if known developer or builder, or the owner of the land. Since the mid-19th century, names have required Many roads were initially lined by individually local-authority approval, initially from parish named Terraces, Rows or Places, with houses Vestries, and then from the Metropolitan Board of numbered within them. -

Bloomsbury in Nineteenth-Century Fiction: Some Quotations Compiled by Matt Ingleby and Deborah Colville
Bloomsbury in Nineteenth-Century Fiction: Some Quotations compiled by Matt Ingleby and Deborah Colville From Theodore Hook’s Sayings and Doings (1824) One day, some week perhaps after the dismissal of Rushbrook, Henry was dining with the Meadowses, who were going to Mrs. Saddington’s assembly in Russell-square. It may be advantageously observed here, that this lady was the dashing wife of the eminent banker, whose acceptance to a bill due the next day my hero had in his pocket. To this party Mrs. Meadows pressed him to accompany them, never forgetting, as I hope my readers never will, that he, the said Henry Merton, Esq. held an appointment under Government of some four-and-twenty hundred pounds per annum, and was therefore a more suitable and agreeable companion for herself and daughter, than when he was “a single gentleman three months ago,” with no estate save that, which lay under his hat, and no income except that derivable from property entirely at the disposal of his father. Henry at first objected; but never having seen much of that part of the town in which this semi-fashionable lived, and desirous of ascertaining how people “make it out” in the recesses of Bloomsbury and the wilds of Guildford Street, and feeling that “all the world to him” would be there, at length agreed to go, and accordingly proceeded with the ladies in their carriage through Oxford-street, St. Giles’s, Tottenham-court-road and so past Dyott-street, and the British Museum, to the remote scene of gaiety, which they, however, reached in perfect safety. -
Initiating Change Locally in Bullying and Aggression Through the School Environment (INCLUSIVE): Trial Protocol
INCLUSIVE trial protocol v 1.1 24/02/2014 Initiating change locally in bullying and aggression through the school environment (INCLUSIVE): trial protocol Sponsor: UCL Institute of Child Health 30 Guilford Street WC1N 1EH London Funder: National Institute for Health research (NIHR) Public Health Research Programme Funder ref: 12/153/60 UCL Ethics Project ID 5248/001 This protocol has been authorised by: Name Role: Signature Date Prof R Viner Chief Investigator Prof C Bonell Co-Chief Investigator Contact Details –Study Team: Chief Investigator Prof Russell Viner UCL Institute of Child Health 30 Guilford Street London WC1N 1EH Tel : +44 (0) 207 905 2190 E-mail : [email protected] Co-Chief Investigator Prof Chris Bonell Institute of Education Department of Children, Families and Health Institute of Education University of London 18 Woburn Square London WC1H 0NR 1 INCLUSIVE trial protocol v 1.1 24/02/2014 +44 (0)20 7612 6731 E-mail: [email protected] TRIAL MANAGER Anne Mathiot 30 Guilford Street London WC1N 1EH Tel : +44 (0) 207 905 2772 Fax : +44 (0) 207 905 2834 E-mail : [email protected] DATA MANAGER Joanna Sturgess Clinical Trial Units London School of Hygiene and Tropical Medicine Room 186, Keppel Street WC1E 7HT London +44 (0)20 7958 8122 +44 (0) 20 7299 4663 [email protected] Please contact the Study Manager for general queries and supply of trial/study documentation 2 INCLUSIVE trial protocol v 1.1 24/02/2014 Table of Content: Aim page 4 Research objective milestones page 4 Design page 4 Study population page 4 Inclusion/Exclusion -
Central Zone Map (Pdf)
001. KATHLEEN LONSDALE BUILDING 100. HEALTH CENTRE 002. 25 GORDON STREET 103. LANGTON CLOSE 003. PEARSON BUILDING 104. SCHAFER HOUSE 004. SLADE SCHOOL - NORTH WING 105. JOHN DODGSON HOUSE 005. WILKINS BUILDING (MAIN BUILDING) 107. DRAYTON HOUSE 006. PHYSICS BUILDING 116. 48 GORDON SQUARE 007. LONDON CENTRE FOR NANOTECHNOLOGY 117. THE RUBIN BUILDING 009. BLOOMSBURY THEATRE 118. 11-13 RUSSELL SQUARE, FLAT 58 012. SOUTH WING 124. IAN BAKER HOUSE 013. CHADWICK BUILDING 125. ANDREW HUXLEY BUILDING 014. FRONT LODGES 126. SCHOOL OF SLAVONIC & EAST EUROPEAN STUDIES 015. TRANSIT HOUSES 131. SCHOOL OF PHARMACY, 29 - 39 BRUNSWICK SQUARE 016. MEDICAL SCIENCES & ANATOMY BUILDING 132. TAVISTOCK HOUSE, TAVISTOCK SQUARE 017. BIOLOGICAL SERVICES UNIT 134. 36-38 GORDON SQUARE 024. 26 GORDON SQUARE 138. MNH GOSH (4 ROOMS) 025. 25 GORDON SQUARE 139. GOSH (3 ROOMS) 026. 24 GORDON SQUARE 145. WHITFIELD STREET LABORATORIES ( 3 ROOMS) 028. 23 GORDON SQUARE 149. 33 BEDFORD PLACE 029. 22 GORDON SQUARE 150. 222 EUSTON ROAD 030. 21 GORDON SQUARE 153. 62-64 HAMPSTEAD ROAD 031. ANECHOIC ROOM 155. 17 RUSSELL SQUARE ( 2 ROOMS) 032. 20 GORDON SQUARE 162. IoE - 20 BEDFORD WAY 033. 19 GORDON SQUARE 163. IoE - 10 WOBURN SQUARE 034. CONTEMPLATION ROOM 1 164. IoE - 11 WOBURN SQUARE 035. 16,17,18 GORDON SQUARE 165. IoE - 12 WOBURN SQUARE 036. HENRY MORLEY BUILDING 166. IoE - 13 WOBURN SQUARE 401 037. MEDAWAR BUILDING 167. IoE - 14 WOBURN SQUARE 040. FOSTER COURT 168. IoE - 15 WOBURN SQUARE 280 041. EGYPTOLOGY 169. IoE - 16 WOBURN SQUARE 042. DMS WATSON BUILDING 170. IoE - 17 WOBURN SQUARE 348 264 044. -

Identifying and Appraising Promising Sources of UK Clinical, Health and Social Care Data for Use by NICE
EPPI-Centre Identifying and appraising promising sources of UK clinical, health and social care data for use by NICE Executive Summary Dylan Kneale, Meena Khatwa, James Thomas EPPI-Centre Social Science Research Unit UCL Institute of Education University College London September 2016 Identifying and appraising promising sources of UK clinical, health and social care data for use by NICE This is a summary of key findings from a report prepared by the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre), UCL Institute of Education for the NICE Science Policy and Research Programme. The full report contains additional details of the EPPI- Centre’s findings. The views expressed here are those of the authors and not necessarily those of NICE, the EPPI-Centre, or any of the stakeholders involved in this research (see acknowledgements section for a list). All data were correct as of August 2015 and any errors and inaccuracies are the sole responsibility of the authors. Executive Summary Introduction Understanding the topography of this real-world data landscape is of prime interest to NICE (National Institute for Health and Care Excellence) in this study, as well as gaining a snapshot of the key areas of debate in the field. Specifically NICE seeks to understand the way in which different real-world data sources could help to support NICE to realise its strategic objectives and to this end, NICE has identified five key uses of real-world data that can help the organisation meet its overall strategic objectives. These are to: (a) Research the effectiveness of interventions or practice in real-world (UK) settings (e.g. -

Forthcoming Events
No. 4568 May 18, 1957 NATURE 1035 FORTHCOMING EVENTS Friday, May 24 (Meetings marked wuh an asterisk• are open to the public) BIOCHEMICAL SOCIETY (in the Department of Biochemistry, Physio logy Institute, Newport Road, Cardiff), at 2 p.m.-Scientillc Papers. ROYAL PHOTOGRAPHIC SOCIETY OF GREAT BRITAIN (at 16 Princes Monday, May 20 Gate, Kensini.iton, London, S.W.7), at 7 p.m.-Dr. Gotthard Wolf UNIVERSITY OF LONDON (in the Physiology Theatre, University (Gottingen): "];'actual Reliability in Scientillc Films". College, Gower Street, London, W.C.1), at 5 p.m.-Dr. E. J. Hewitt: ROYAL INSTITUTION (at 21 Albemarle Street, London, W.1), at "Mlcronutrlent Element Metabolism in Plants".* (Further lectures 9 p.m.-Dr. Harold Heywood: "Solar Energy-a Challenge to the on May 27 and June 3.) Future". BRITISH SOCIETY FOR THE HISTORY OF SCIENCE, PHILOSOPHY OF SCIENCE GROUP (in the Joint Staff Common Room, University College, Gower Street, London, W.C.1), at 5.30 p.m.-Dr. J. R. Smythies: "The Notion of an Image Space". INSTITUTION OF MECHANICAL ENGINEERS (joint meeting with the APPOINTMENTS VACANT INSTITUTION OF CIVIL ENGINEERS and the INSTITUTION OF ELECTRICAL ENGINEERS, at the Institution of Civil Engineers, Great George Street, APPLICATIONS are invited for the following appointments on or London, S.W.1), at 5.30 p.m.-Report on "Hydroelectric Projects before the dates mentioned : in the U.S.S.R.". DEMONSTRATOR IN THE DEPARTMENT OF CHEMISTRY-The Regis INSTITUTB OF METAL FINISHING (at the Northampton Polytechnic, trar, King's College, Newcastle-upon-Tyne (May 24). GltADUATE DEMONSTRATOR IN PARASITOLOGY, to carry out research, St. -
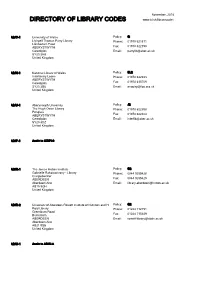
Download a PDF Copy of the Directory of Library Codes
November, 2018 DIRECTORY OF LIBRARY CODES www.bl.uk/librarycodes AB/C-1 University of Wales Policy: G Llyfrgell Thomas Parry Library Phone: 01970 621871 Llanbadarn Fawr ABERYSTWYTH Fax: 01970 622190 Ceredigion Email: [email protected] SY23 3AS United Kingdom AB/N-1 National Library of Wales Policy: SL2 Interlibrary Loans Phone: 01970 632933 ABERYSTWYTH Ceredigion Fax: 01970 615709 SY23 3BU Email: [email protected] United Kingdom AB/U-1 Aberystwyth University Policy: J2 The Hugh Owen Library Phone: 01970 622398 Penglais ABERYSTWYTH Fax: 01970 622404 Ceredigion Email: [email protected] SY23 3DZ United Kingdom AD/P-1 Apply to QZ/P22 AD/R-1 The James Hutton Institute Policy: G2 Gabrielle Rakotoarivony - Library Phone: 0844 9285428 Craigiebuckler ABERDEEN Fax: 0844 9285429 Aberdeenshire Email: [email protected] AB15 8QH United Kingdom AD/R-2 University of Aberdeen Rowett Institute of Nutrition and H Policy: G2 Reid Library Phone: 01224 712751 Greenburn Road Bucksburn Fax: 01224 715349 ABERDEEN Email: [email protected] Aberdeenshire AB21 9SB United Kingdom AD/U-1 Apply to AD/U-3 AD/U-2 Apply to AD/U-3 AD/U-3 University of Aberdeen Policy: J2 Sir Duncan Rice Library Phone: 01224 273330 Bedford Road ABERDEEN Fax: 01224 487048 Aberdeenshire Email: [email protected] AB24 3AA United Kingdom AD/U-5 Apply to AD/U-3 AD/U-6 Apply to AD/U-3 AD/U-7 University of Aberdeen Policy: G2 Interlibrary Loans Phone: 01224 552488 Medical School Library Foresterhill Fax: 01224 685157 ABERDEEN Email: [email protected] AB25 2ZD -
S:\EFD 4.0 Property\4.02 Space Allocation\4.7.1 CAD Property
001. KATHLEEN LONSDALE BUILDING 100. HEALTH CENTRE 002. 25 GORDON STREET 103. LANGTON CLOSE 003. PEARSON BUILDING 104. SCHAFER HOUSE 004. SLADE SCHOOL - NORTH WING 105. JOHN DODGSON HOUSE 005. WILKINS BUILDING (MAIN BUILDING) 107. DRAYTON HOUSE 006. PHYSICS BUILDING 116. 48 GORDON SQUARE 007. LONDON CENTRE FOR NANOTECHNOLOGY 117. THE RUBIN BUILDING 009. BLOOMSBURY THEATRE 118. 11-13 RUSSELL SQUARE, FLAT 58 012. SOUTH WING 124. IAN BAKER HOUSE 013. CHADWICK BUILDING 125. ANDREW HUXLEY BUILDING 014. FRONT LODGES 126. SCHOOL OF SLAVONIC & EAST EUROPEAN STUDIES 015. TRANSIT HOUSES 131. SCHOOL OF PHARMACY, 29 - 39 BRUNSWICK SQUARE 016. MEDICAL SCIENCES & ANATOMY BUILDING 132. TAVISTOCK HOUSE, TAVISTOCK SQUARE 017. BIOLOGICAL SERVICES UNIT 134. 36-38 GORDON SQUARE 024. 26 GORDON SQUARE 138. MNH GOSH (4 ROOMS) 025. 25 GORDON SQUARE 139. GOSH (3 ROOMS) 026. 24 GORDON SQUARE 145. WHITFIELD STREET LABORATORIES ( 3 ROOMS) 028. 23 GORDON SQUARE 149. 33 BEDFORD PLACE 029. 22 GORDON SQUARE 150. 222 EUSTON ROAD 030. 21 GORDON SQUARE 153. 62-64 HAMPSTEAD ROAD 031. ANECHOIC ROOM 155. 17 RUSSELL SQUARE ( 2 ROOMS) 032. 20 GORDON SQUARE 162. IoE - 20 BEDFORD WAY 033. 19 GORDON SQUARE 163. IoE - 10 WOBURN SQUARE 034. CONTEMPLATION ROOM 1 164. IoE - 11 WOBURN SQUARE 035. 16,17,18 GORDON SQUARE 165. IoE - 12 WOBURN SQUARE 036. HENRY MORLEY BUILDING 166. IoE - 13 WOBURN SQUARE 401 037. MEDAWAR BUILDING 167. IoE - 14 WOBURN SQUARE 040. FOSTER COURT 168. IoE - 15 WOBURN SQUARE 280 041. EGYPTOLOGY 169. IoE - 16 WOBURN SQUARE 042. DMS WATSON BUILDING 170. IoE - 17 WOBURN SQUARE 348 264 044. -

Nature Forthcoming Events Appointments Vacant
No.4543 November 24, 1956 NATURE 1197 UNIVERSITY OF LONDON (in the Physiology Theatre, University FORTHCOMING EVENTS College, Gower Street, London, W.C.l), at 5 p.m.-Prof. G. F. Marrian: "Some Recent Progress in the Biochemistry of the <Estrogenic Hor (Meetings marked with an asterisk• are open to the public) mones".• INSTITUTION OF CIVIL ENGINEERS (at Great George Street, West Monday, November 26 minster, London, S.W.l), at 5.30 p.m.-Dr. W. H. J. Vernon: INSTITUTE OF NEUROLOGY (in the Lecture Theatre, The National "Metallic Corrosion and Conservation", Hospital, Queen Square, London, W.C. 1), at 5 p.m.-Prof. S. T. Bok INSTITUTION OF ELECTRICAL ENGINEERS (at Savoy Place, London, (Amsterdam) : "The Structure of the Cerebral Cortex as Studied W.C.2), at 5.30 p.m.-Prof. R. 0. Kapp: "Differences of Opinion by Quantitative Methods-1''.* (Further lecture on November 30.) about Dimensionsn. ROYAL GEOGRAPHICAL SOCIETY (at 1 Kensington Gore, London, SOCIE~Y OF CHEMICAL INDUSTRY, PLASTICS AND POLYMER GROUP S.W.7), at 5 p.m.-Mr. B. W. Sparks: "Evolution of the Relief of (at the Royal Society of Tropical Medicine and Hygiene, Manson the Cam Valley". House, 26 Portland Place, London, W.l), at 6.30 p.m.-Prof. H. F. BRITISH SOCIETY FOR THE HISTORY OF SCIENCE (in the Lecture Mark : "Recent Progress in Heterogeneous Polymerization of Theatre of the Science Museum, Exhibition Road, South Kensington, Olefines". London, S.W.7), at 5.30 p.m.-Mr. John Fisher: "Electricity in Germany in the Eighteenth Century". Friday, November 30 ROYAL SOCIETY OF ARTS (at John Adam Street, Adelphi, London, TEXTILE INSTITUTE (at 10 Bmckfriars Street, Manchester 3) W.C.2), at 6 p.m.-Dr. -

Directory of Library Codes
September, 2021 DIRECTORY OF LIBRARY CODES www.bl.uk/librarycodes AB/C-1 Apply to AB/U-1 AB/N-1 National Library of Wales Policy: SL2 Interlibrary Loans Phone: 01970632933 ABERYSTWYTH Email: [email protected] Ceredigion SY23 3BU United Kingdom AB/U-1 Aberystwyth University Policy: J2 The Hugh Owen Library Phone: 01970622398 Penglais Email: [email protected] ABERYSTWYTH Ceredigion SY23 3DZ United Kingdom AD/P-1 Apply to QZ/P22 AD/R-1 The James Hutton Institute Policy: G2 Library Phone: 08449285428 Craigiebuckler Email: [email protected] ABERDEEN Aberdeenshire AB15 8QH United Kingdom AD/R-2 University of Aberdeen Rowett Institute of Nutrition and Policy: G2 Health Reid Library Phone: 01224712751 Greenburn Road Email: [email protected] Bucksburn ABERDEEN Aberdeenshire AB21 9SB United Kingdom AD/U-1 Apply to AD/U-3 AD/U-2 Apply to AD/U-3 AD/U-3 University of Aberdeen Policy: J2 Sir Duncan Rice Library Phone: 01224273330 Bedford Road Email: [email protected] ABERDEEN Aberdeenshire AB24 3AA United Kingdom AD/U-5 Apply to AD/U-3 AD/U-6 Apply to AD/U-3 AD/U-7 University of Aberdeen Policy: G2 Interlibrary Loans Phone: 01224552488 Medical School Library Email: [email protected] Foresterhill ABERDEEN AB25 2ZD United Kingdom AD/U-8 Apply to AD/U-3 BA/C-1 Bath College Policy: G2 Library Phone: 01225328899 Avon Street Email: [email protected] BATH Somerset BA1 1UP United Kingdom BA/P-1 Apply to QW/P-7 BA/S-1 The Royal Photographic Society Policy: F2 RPS House Phone: 01173164452 337 Paintworks Email: [email protected] -
S:\EFD 4.0 Property\4.7 Space Allocation\4.7.1 CAD Property Records\Stephanos Stephanides\Names\Gary Sabini\UCL FM Zones\UCL
001. KATHLEEN LONSDALE BUILDING 100. HEALTH CENTRE 002. 25 GORDON STREET 103. LANGTON CLOSE 003. PEARSON BUILDING 104. SCHAFER HOUSE 004. SLADE SCHOOL - NORTH WING 105. JOHN DODGSON HOUSE 005. WILKINS BUILDING (MAIN BUILDING) 107. DRAYTON HOUSE 006. PHYSICS BUILDING 116. 48 GORDON SQUARE 007. LONDON CENTRE FOR NANOTECHNOLOGY 117. THE RUBIN BUILDING 009. BLOOMSBURY THEATRE 118. 11-13 RUSSELL SQUARE, FLAT 58 012. SOUTH WING 124. IAN BAKER HOUSE 013. CHADWICK BUILDING 125. ANDREW HUXLEY BUILDING 014. FRONT LODGES 126. SCHOOL OF SLAVONIC & EAST EUROPEAN STUDIES 015. TRANSIT HOUSES 131. SCHOOL OF PHARMACY, 29 - 39 BRUNSWICK SQUARE 016. MEDICAL SCIENCES & ANATOMY BUILDING 132. TAVISTOCK HOUSE, TAVISTOCK SQUARE 017. BIOLOGICAL SERVICES UNIT 134. 36-38 GORDON SQUARE 024. 26 GORDON SQUARE 138. MNH GOSH (4 ROOMS) 025. 25 GORDON SQUARE 139. GOSH (3 ROOMS) 026. 24 GORDON SQUARE 145. WHITFIELD STREET LABORATORIES ( 3 ROOMS) 028. 23 GORDON SQUARE 149. 33 BEDFORD PLACE 029. 22 GORDON SQUARE 150. 222 EUSTON ROAD 030. 21 GORDON SQUARE 153. 62-64 HAMPSTEAD ROAD 031. ANECHOIC ROOM 155. 17 RUSSELL SQUARE ( 2 ROOMS) 032. 20 GORDON SQUARE 162. IoE - 20 BEDFORD WAY 033. 19 GORDON SQUARE 163. IoE - 10 WOBURN SQUARE 034. CONTEMPLATION ROOM 1 164. IoE - 11 WOBURN SQUARE 035. 16,17,18 GORDON SQUARE 165. IoE - 12 WOBURN SQUARE 036. HENRY MORLEY BUILDING 166. IoE - 13 WOBURN SQUARE 401 037. MEDAWAR BUILDING 167. IoE - 14 WOBURN SQUARE 040. FOSTER COURT 168. IoE - 15 WOBURN SQUARE 280 041. EGYPTOLOGY 169. IoE - 16 WOBURN SQUARE 042. DMS WATSON BUILDING 170. IoE - 17 WOBURN SQUARE 348 264 044.