Asis with Tropicamide and Phenylephrine on Intraocular Pressure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medication List
Medication List Walgreens Plus™ members receive discounts on thousands of generic and brand-name medications included on this Medication List, which is divided into two sections, “Value Priced” Medications and “Discounted” Medications*. The price for a medication identified as “Value-Priced” is listed below: Get savings up to 85% off Cash Prices • 30-day-supply drugs cost $5 (tier 1), $10 (tier 2) or $15 (tier 3) on Atorvastatin (generic Lipitor) and • 90-day-supply drugs cost $10 (tier 1), $20 (tier 2) or $30 (tier 3) Rosuvastatin (generic Crestor) †† The Discounted Medications section lists the discounts offered to Walgreens Plus members on other generic and brand-name medications not included in the Value-Priced Medication section. The price for a medication is based on its tier and whether it is a 30-day or 90-day supply†. There may be an additional cost for quanities greater than those listed. This discount prescription pricing applies only to Walgreen Plus members on prescriptions purchased in select Walgreens stores that are not billed to insurance and/or used in combination with other health or pharmacy benefit programs. For further details, see your pharmacist or Walgreens.com/Plus. VALUE GENERICS NAPROXEN 250MG TAB 2 60 180 Antifungal NAPROXEN 500MG TAB 2 60 180 Quantity NAPROXEN 375MG TAB 2 60 180 Drug Name Tier 30 90 NAPROXEN DR 500MG TAB 3 60 180 FLUCONAZOLE 150MG TAB 2 1 3 TERBINAFINE 250MG TAB 2 30 90 Asthma Quantity Antiviral Drug Name Tier 30 90 Quantity ALBUTEROL 0.083% INH SOLN 25X3ML 2 75 225 Drug Name Tier 30 90 AMINOPHYLLINE -

World Health Organization Model List of Essential Medicines, 21St List, 2019
World Health Organizatio n Model List of Essential Medicines 21st List 2019 World Health Organizatio n Model List of Essential Medicines 21st List 2019 WHO/MVP/EMP/IAU/2019.06 © World Health Organization 2019 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. World Health Organization Model List of Essential Medicines, 21st List, 2019. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. -
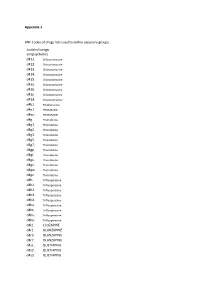
Appendix 1 BNF Codes of Drugs Lists Used to Define Exposure Groups
Appendix 1 BNF Codes of drugs lists used to define exposure groups. Anticholinergic antipsychotics d411. Chlorpromazine d412. Chlorpromazine d413. Chlorpromazine d414. Chlorpromazine d415. Chlorpromazine d41a. Chlorpromazine d41b. Chlorpromazine d41c. Chlorpromazine d41d. Chlorpromazine d4b1. Perphenazine d4e1. PROMAZINE d4ex. PROMAZINE d4g.. Thioridazine d4g1. Thioridazine d4g2. Thioridazine d4g3. Thioridazine d4g5. Thioridazine d4g7. Thioridazine d4gp. Thioridazine d4gt. Thioridazine d4gu. Thioridazine d4gv. Thioridazine d4gw. Thioridazine d4gz. Thioridazine d4h.. Trifluoperazine d4h1. Trifluoperazine d4h2. Trifluoperazine d4h3. Trifluoperazine d4h4. Trifluoperazine d4hs. Trifluoperazine d4ht. Trifluoperazine d4hu. Trifluoperazine d4hx. Trifluoperazine d4l2. CLOZAPINE d4r1. OLANZAPINE d4r3. OLANZAPINE d4r7. OLANZAPINE d4s1. QUETIAPINE d4s2. QUETIAPINE d4s3. QUETIAPINE d4s5. QUETIAPINE d4ss. QUETIAPINE d4sx. QUETIAPINE Tricyclic antidepressants d7... d71.. Amitriptyline d711. Amitriptyline d712. Amitriptyline d713. Amitriptyline d719. Amitriptyline d71a. Amitriptyline d71b. Amitriptyline d71c. Amitriptyline d71d. Amitriptyline d71e. Amitriptyline d71f. Amitriptyline d71u. Amitriptyline d71v. Amitriptyline d71w. Amitriptyline d71y. Amitriptyline d71z. Amitriptyline d73.. Clomipramine d731. Clomipramine d732. Clomipramine d733. Clomipramine d736. Clomipramine d73s. Clomipramine d73t. Clomipramine d73u. Clomipramine d73v. Clomipramine d73w. Clomipramine d73z. Clomipramine d75.. DOSULEPIN d751. DOSULEPIN d752. DOSULEPIN d755. DOSULEPIN d756. -

Queensland Health List of Approved Medicines
Queensland Health List of Approved Medicines Drug Form Strength Restriction abacavir * For use in accord with PBS Section 100 indications * oral liquid See above 20 mg/mL See above tablet See above 300 mg See above abacavir + lamivudine * For use in accord with PBS Section 100 indications * tablet See above 600 mg + 300 mg See above abacavir + lamivudine + * For use in accord with PBS Section 100 indications * zidovudine tablet See above 300 mg + 150 mg + 300 mg See above abatacept injection 250 mg * For use in accord with PBS Section 100 indications * abciximab (a) Interventional Cardiologists for complex angioplasty (b) Interventional and Neuro-interventional Radiologists for rescue treatment of thromboembolic events that occur during neuroendovascular procedures. * Where a medicine is not TGA approved, patients should be made fully aware of the status of the medicine and appropriate consent obtained * injection See above 10 mg/5 mL See above abiraterone For use by medical oncologists as per the PBS indications for outpatient and discharge use only tablet See above 250 mg See above 500 mg See above acamprosate Drug and alcohol treatment physicians for use with a comprehensive treatment program for alcohol dependence with the goal of maintaining abstinence. enteric tablet See above 333 mg See above acarbose For non-insulin dependent diabetics with inadequate control despite diet; exercise and maximal tolerated doses of other anti-diabetic agents tablet See above 50 mg See above 100 mg See above acetazolamide injection 500 mg tablet 250 mg acetic acid ear drops 3% 15mL solution 2% 100mL green 3% 1 litre 6% 1 Litre 6% 200mL Generated on: 30-Aug-2021 Page 1 of 142 Drug Form Strength Restriction acetylcysteine injection For management of paracetamol overdose 2 g/10 mL See above 6 g/30 mL See above aciclovir cream Infectious disease physicians, haematologists and oncologists 5% See above eye ointment For use on the advice of Ophthalmologists only. -

Drugs Which Can Affect Near Vision: a Useful List
Drugs Which Can Affect Near Vision: A Useful List Joanne L. Smith B.Sc., Ph.Phm.* J. Raymond Buncic, M.D., F.R.C.S.(C)t ABSTRACT This paper documents a list of drugs that cause problems with near vision, by virtue of effects on accommodation, occasionally refractive error and diplopia. It is meant as a reference aid to the clinician when confronted with problems of focusing on near objects or print. There are many drugs that have been reported to interfere with near or reading vision, producing blurring, decreased accommodation and diplopia. This paper lists the drugs that have been reported in the literature to produce symptoms which interfere with near vision. Case reports for the listed drugs vary greatly from many to few. The drugs have been divided into the following categories: those causing (A) blurring at near, (B) diplopia and (C) induced myopia. Those drugs which only rarely cause these symptoms have been omitted. From the Departments of Pharmacy* and Ophthalmologyt, The Hospital For Sick Children, Toronto, Ontario, Canada Requests for reprints should be addressed to: Dr. J. Raymond Buncic, Department of Ophthalmology, The Hospital For Sick Children, 555 University Ave., Toronto, Ontario, Canada M5G lX8 TABLE 1 DRUGS COMMONLY CAUSING DIFFICULTY WITH FOCUSING AT NEAR OR BLURRED VISION. DRUG INCIDENCE REFERENCE Antipsychotics Chlorpromazine 14-23 8 Clozapine 5 8,14 Fluphenazine 1.2-4.3 8 Haloperidol 6.8-16 8 Loxapine 12,14 Perphenazine 7.4-17.8 8 Pimozide 20 8 Risperidone 1-2%, >/= 10% 11 Thioridazine 0.6-18 8 Thiothixene 20 8 -
Reclassification of Hyoscine Butylbromide for Oral Use
Reclassification of Hyoscine butylbromide for oral use in medicines containing not more than 20 milligrams per dose (Addition of oral liquids in the current classification) Present classification: Restricted Proposed classification: Restricted AFT Pharmaceuticals Limited Level 1, Nielsen Building 129 Hurstmere Rd Takapuna, Auckland, 0622 PO Box 33-203, Takapuna, Auckland Page 1 of 16 Objective: This application seeks reclassification of hyoscine butylbromide for oral use in medicines containing not more than 20 milligrams per dose. Page 2 of 16 PART A 1. International Non-Proprietary Name of the Medicine Hyoscine butylbromide 2. Proprietary name(s) Gastrosoothe (Proposed) (hyoscine butylbromide 1 mg/mL) 3. Name of the company/organisation/individual requesting a reclassification AFT Pharmaceuticals Ltd 129 Hurstmere Road Takapuna 0622 Auckland New Zealand 4. Dose form(s) and strength(s) for which a change is sought Dose form: Oral liquid Strength: 1 mg/mL Pack size: 200 mL. 5. Proposed pack size, storage conditions and any other qualifications Proposed pack size: Bottle containing 200 mL (1 mg/mL) of hyoscine butylbromide oral liquid Storage conditions: Store below 30 °C. 6. Indications for which change is sought Indication: for the relief of muscle spasm of the gastrointestinal tract 7. Present classification of the medicine Ingredient Conditions (if any) Classification Hyoscine except when specified elsewhere in this schedule Prescription butylbromide Hyoscine for oral use in medicines containing not more than 10 milligrams per Restricted butylbromide dose form and in packs containing not more than 20 tablets or capsules; for oral use in medicines containing not more than 20 milligrams per dose form and in packs containing not more than 10 tablets or capsules for the relief of muscle spasm of the gastrointestinal tract Page 3 of 16 8. -

Axert , a New “Triptan”
Rx Details January 1, 2014 Formulary Update The January 2014 Drug Formulary update is included as an attachment. Significant updates include: Oxycodone ER (OxyContin). Quantity Limits for OxyContin have been updated for Commercial Drug Formularies and State Health Care Programs, effective April 1 2014. Quantity limits now allow a maximum of 120mg morphine equivalents per day (MED), similar to other opioid medications. New Daily New Daily mg Strength MED* Quantity Limit limit 10 mg 4 (no change) 40 60 15 mg 4 (no change) 60 90 20 mg 4 (no change) 80 120 30 mg 2 60 90 40 mg 2 80 120 60 mg 0 0 0 80 mg 0 0 0 * MED (morphine equivalents per day) is used to determine dosage levels of different opioids by converting them to morphine equivalents. Additional communications are being sent to affected providers and members. Exceptions allowing higher quantities can be requested if medically necessary. Requests should include a treatment plan, and must include an assessment of the risk of addiction, abuse, and diversion. Tricyclic antidepressants. These tricyclic antidepressants will be limited for elderly members (ages 65 and older) in Commercial and State Health Care Programs, effective April 1 2014. • amitriptyline (Elavil), chlordiazepoxide/ amitriptyline (Limbitrol), and perphenazine/ amitriptyline (Etrafon) • doxepin (Silenor) • imipramine (Tofranil) • trimipramine (Surmontil) • clomipramine (Anafranil). Clomipramine will be approved for obsessive‐compulsive disorder (no additional coverage criteria). These tricyclic antidepressants are anticholinergic, with a high rate of side effects in the elderly. Nortriptyline (Pamelor) and desipramine (Norpramin) remain on formulary for all age groups. Additional communications are being sent to affected providers and members. -

SUPPLEMENT Etable 1
SUPPLEMENT eTable 1. List of medications used for exclusions and prescription drug history variables Anticonvulsants (past use Medications used for prescription drug history variables evaluated as an exclusion criterion) Antidepressants Anticholinergics Carbamazepine Bupropion Aclidinium Clobazam Atropine Clonazepam Other antidepressants: Cyclopentolate Clorazepate Amitriptyline Glycopyrrolate Diazepam Amoxapine Homatropine Divalproex Butriptyline Ipratropium Ethosuximide Citalopram Methscopolamine Ethotoin Clomipramine Scopolamine Ezogabine Desipramine Tiotropium Felbamate Desvenlafaxine Tropicamide Fosphenytoin Dibenzepin Gabapentin Dotheipin Lacosamide Doxepin Lamotrigine Duloxetine Levetiracetam Escitalopram Lorazepam Fluoxetine Mephenytoin Fluvoxamine Mephobarbital Imipramine Metharbital Iprindole Methsuximide Isocarboxazid Oxcarbazepine Levomilnacipran Paramethadione Lofepramine Phenacemide Maprotiline Phenobarbital Melitracen Phensuximide Mianserin Phenytoin Milnacipran Pregabalin Mirtazapine Primidone Nefazodone Rufinamide Nortriptyline Tiagabine Opipramol Topiramate Paroxetine Trimethadione Phenelzine Valproate Sodium Protriptyline Valproic Acid Sertraline Vigabatrin Tranylcypromine Zonisamide Trazodone Trimipramine Tryptophan Venlafaxine Vilazodone 1 eTable 2. Diagnostic codes used for medical history variables Medical condition Diagnostic codes (ICD-9)a Stroke 431.xx, 433.xx, 434.xx, 436.xx Other cerebrovascular 430.xx, 432.xx, 435.xx, 437.xx, 438.xx disease Brain injury 850.xx-854.xx, 907.0x Hypoxemia 799.02 Infection 001.xx-039.xx -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Homatropine > Printer-Friendly PDF
Published on British Columbia Drug and Poison Information Centre (BC DPIC) ( http://www.dpic.org) Home > Drug Product Listings > Homatropine > Printer-friendly PDF Homatropine Trade Name: Isopto Homatropine Manufacturer/Distributor: Alcon Canada Classification: Mydriatic agent ATC Class: S01FA - Anticholinergic Status: discontinued Presentation: Eye Drops: 2%. DIN: 00000779 Eye Drops: 5%. DIN: 00000787 Comments: May 2016: The product has been discontinued by the company. There are no other suppliers of this medication in Canada. There are other anticholinergic eye drops available (e.g. atropine, cyclopentolate, tropicamide). Keywords: homatropine drug discontinuation Access: public Back to: Please note - this is not a complete list of products available in Canada. For a complete list of drug products marketed in Canada, visit the Health Canada Drug Product Database Status: <Any> ? Search Terms: Apply A (37) | B (20) | C (24) | D (37) | E (40) | F (12) | G (11) | H (9) | I (24) | K (1) | L (26) | M (12) | N (7) | O (12) | P (28) | R (14) | S (27) | T (33) | U (4) | V (13) | W (2) | Z (4) Date Marketed in Common Generic Name Classification Canada Trade Name(s) (yyyy/mm/dd) Estropipate Ogen Apo-digoxin; Digoxin pms-Digoxin; Lanoxin Panoxyl Clear Salicylic acid + Triclosan Acne Cleansing Gel Risedronate + Calcium Actonel APC carbonate Sibutramine Meridia 2010/10/08 Rosiglitazone + Avandaryl 2011/03/31 glimepiride Phosphate Phosphate Effervescent 2017/01/01 Sandoz Metronidazole with Flagystatin nystatin vaginal cream vaginal cream Orajel teething -

Cross Discipline Team Leader Review
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208151Orig1s000 CROSS DISCIPLINE TEAM LEADER REVIEW NDA 208151 William M. Boyd, M.D. Cross Discipline Team Leader Review Other dosage forms of atropine are marketed in the United States. Some of these products have approved new drug applications and others do not. Pupillary dilation and cycloplegia impair visual function. When these actions are necessary for greater than 72 hours either for diagnostic or therapeutic action, there are no pharmacologic alternatives. When maximal cycloplegia is required, there are no therapeutic alternatives. Table of Currently Available Treatments for Proposed Indications Drug Substance Duration Action Subject of an (normal individual) approved ophthalmic application Phenylephrine ~ 4 hours Mydriasis Yes Tropicamide ~ 4 hours Mydriasis & Cycloplegia Yes Cyclopentolate ~ 12 hours Mydriasis & Cycloplegia Yes Scopolamine ~ 72 hours Mydriasis & Cycloplegia No Homatropine ~ 48 hours Mydriasis & Cycloplegia No Atropine ~14 days Mydriasis, Cycloplegia, and in Yes the treatment of amblyopia The Applicant requested a “Pre-IND” meeting with the Division of Transplant and Ophthalmology Products. The meeting took place on February 11, 2013, during which the Agency agreed that a 505(b)(2) application was an acceptable pathway for a new drug application in which the applicant did not have a right to reference studies conducted in support of the drug product. There are numerous literature articles supporting the clinical use of atropine ophthalmic solution. Many of the articles identify a specific brand name product (the current applicant’s unapproved, marketed product). None of the literature articles necessary to support approval specifically identify the listed drug that is a pharmaceutical equivalent to the proposed product (NDA 206289). -

Acute Atropine Intoxication with Psychiatric Symptoms by Herbal Infusion of Pulmonaria Officinalis (Lungwort)
Eur. J. Psychiat. Vol. 21, N.° 2, (93-97) 2007 Keywords: Pulmonaria Officinalis, Herbal reme- dies, Atropine intoxication, Delirium. Acute atropine intoxication with psychiatric symptoms by herbal infusion of Pulmonaria officinalis (Lungwort) Enrique Baca-García, M.D.* Hilario Blasco-Fontecilla, M.D.** Carlos Blanco, M.D.*** Carmen Díaz-Sastre, M.D.**** María Mercedes Pérez-Rodríguez, M.D.**** Jerónimo Sáiz-Ruiz, M.D., Ph.D.****,***** * Psychiatry Department. Fundación Jiménez-Díaz Hospital, Madrid, Spain ** Doctor R. Lafora Hospital, Madrid, Spain *** Columbia College of Physicians and Surgeons. Presbyterian Hospital, New York, USA **** Psychiatry Department. Ramón y Cajal Hospital, Madrid, Spain ***** University of Alcala, Madrid, Spain SPAIN, USA ABSTRACT – Background and objectives: Lungwort infusion is a preparation extracted from Pulmonaria officinalis which is occasionally used as a folk remedy for the common cold. The current report aims to describe acute atropine intoxications with delirium caused by Lungwort infusion in several members of the same family. Methods: Description of three case reports. Search of literature through Medline. Results: Three generations of a same family presented acute and moderately severe atropine intoxications after drinking an infusion prepared with Pulmonaria officinalis. Conclusions: Despite the lack of scientific evidence for its clinical use, medicinal plants continue being widely used. In spite of severe adverse effects reported, the general thought is that herbal remedies are harmless. To our knowledge, this is the first report of acute atropine intoxications with psychiatric symptoms secondary to Pulmonaria offici- nalis in several members of a family. We suspect that the lungwort infusion may have been contaminated with some other substance with atropinic properties.