Assessment the Relationship of Maternal Child Health Accessibility, Infant Mortality and Fertility
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NAME DESIGNATION DEPARTMENT EMAIL ADDRESS Mdez Jbp
NAME DESIGNATION DEPARTMENT EMAIL ADDRESS mdez jbp Managing Director MD EZ Office [email protected] CHIEF GENERAL MANAGER ADB- Shiv Yadav DIRECTORTECHNICAL RGGVY [email protected] Prakash Kawade C.E. C.E. SAGAR REGION [email protected] Praveen Sinha C.E. C.E. JABALPUR REGION [email protected] Santosh Tandan C.E. C.E. REWA REGION [email protected] CHIEF GENERAL MANAGER FEEDER Abhay Bishnoi C.G.M SEPARATION [email protected] CHIEF GENERAL MANAGER ADB- Ashok Dhurway C.G.M RGGVY [email protected] Amar Bahadur Singh C.G.M. HR&A CHIEF GENERAL MANAGER HR&A [email protected] CEJR jabalpur CE mpez [email protected] CErr Rewa CE mpez [email protected] CEsr Sagar CE mpez [email protected] cfo mpez cfo mpez [email protected] cgm ddugjy CGM mpez [email protected] CHIEF GENERAL MANAGER Ajay Sharma CGM RAPDRP [email protected] cgm adb cgmADB mpez [email protected] ed comm cgmcomm mpez [email protected] cgm fs cgmfs mpez [email protected] cgm hr cgmhr mpez [email protected] ed purchase Cgmpurchase mpez [email protected] cgm rapdrp cgmrapdrp mpez [email protected] Vivek Chandra G.M.& Head-IT G.M Head IT [email protected] cgmenfo ENFORCEMENT edenfo mpez [email protected] gm works EDWORKS mpez [email protected] Vipin Dhagat Chief CS&A CHIEF C.S.&A. -

184Aà Ur /2021
4HUTT 192. yaiy zar, HuaT5A R, UA-1, H.UI. 7T - [email protected] tura, fd=t 7 /08/2021 cDHIC184aà uR /2021 H. -00- stta qrd àa I ufRTUT fts 23/8/21 H28/8/21 a 4THTfGra f IT}UTT|H àa BIufAnfat 3 Covid- 19 5U 377 fàyH uNTIPTÍ BRUI TE URTEUT ATCITE 3TufGra fouI GI TET 5. ufRieur À Fafea fet at zqa-iGTBTRI 5 fY DUT [email protected] -IT rt 7 fa. àuR /2021 4UT, iC/7 /08/2021 ufafef: 2. faT Auao, FHT, 4UTT AR HTY| Process Training Program for Principal's Office Batch 10 (23/8/2021-28/8/2021) Subject College Name College Code No. Name Designation Govt. College, 807 Prof. G.S. Gill Assistant Professor English Badamalehra Commerce Govt. College, 807 Dr. Anil Kumar Singh Assistant Professor Badamalehra Govt. College, 807 Pinki Asati Assistant Professor Geography Badamalehra 809 Dr. Meenakshi Norke Assistant Professor EconomicS Govt College Rajnagar Govt College Rajnagar 809 Dr. Pushpa Dubey In Charge Principal Hindi 810 Dr. Pushpa Samvedi Assistant Professor & Hindi Govt.Bapu Degree College Incharge Principal Nowgong 810 Shri Santosh Kumar Rajak Assistant Professor Hindi Govt.Bapu Degree College Nowgong 810 Shri Piyush Kain Assistant Professor English Govt.Bapu Degree College Nowgong 811 Mr. shivam shukla In Charge Principal Economics Govt Naveen College Buxwaha 811 0 Mr. kailash kumar rajak Assistant Professor Hindi Govt Naveen College Buxwaha 811 11 Mr. neeraj kumar Assistant Professor Botany Govt Naveen College Buxwaha Dr. A.K. Khare In Charge Principal Commerce Govt. P.G. College, Panna 901 Dr. P.P. -

Madhya Pradesh Administrative Divisions 2011
MADHYA PRADESH ADMINISTRATIVE DIVISIONS 2011 U T KILOMETRES 40 0 40 80 120 T N Porsa ! ! ! Ater Ambah Gormi Morena ! P Bhind P A ! BHIND MORENA ! Mehgaon! A ! Ron Gohad ! Kailaras Joura Mihona Sabalgarh ! ! P ! ! Gwalior H ! Dabra Seondha ! GWALIOR ! Lahar R Beerpur Vijaypur ! ! Chinour Indergarh Bhitarwar DATIA Bhander ! T SHEOPUR Datia ! Sheopur Pohri P P P ! ! Narwar R Karahal Shivpuri A ! Karera Badoda P SHIVPURI ! S ! N!iwari D D ! ! Pichhore Orchh!a Gaurihar ! D Nowgong E ! Prithvipur Laundi Kolaras ! Chandla Jawa ! D TIKAMGARHPalera ! ! ! ! Teonthar A ! ! Jatara ! ! Maharajpur Khaniyadhana ! Sirmour Bad!arwas Mohangarh P ! Ajaigarh ! Naigarhi S ! ! Majhgawan ! REWA ! ! ! Chhatarpur Rajnagar ! Semaria ! ! Khargapur Birsinghpur Mangawan Hanumana Singoli Bamori Isagarh Chanderi ! CHHATARPUR (Raghurajnagar) ! Guna ! P Baldeogarh P Kotar (Huzur) Maugan!j Shadhora Panna P ! Raipur-Karchuliyan ! Chitrangi ! ASHOKNAGAR Tikamgarh Bijawar ! Rampur P ! J Jawad P ! ! DevendranagarNago!d !Gurh Sihawal ! ! P Baghelan ! Churhat GUNA Bada Malhera ! ! P H NEEMUCH Bhanpura Ashoknagar ! !Gunnor (Gopadbanas) ! I Raghogarh N Ghuwara D ! SATNA I ! ! A P ! Manasa ! Mungaoli PANNA Unchahara !Amarpatan Rampur Naikin Neemuch ! ! ! Amanganj SINGRAULI ! Aron ! Shahgarh Buxwaha ! Pawai SIDHI ! Kumbhraj Bina ! ! Ram!nagar !Majhauli Deosar Jiran Malhargarh Garoth Hatta ! ! Kurwai ! Shahnagar Maihar P ! ! Maksoodanga!rh Malthon Batiyagarh ! MANDSAUR ! ! ! Beohari Singrauli Mandsaur Shamgarh Jirapur ! Chachaura Lateri Sironj Khurai Raipura ! ! ! A ! P ! ! ! ! -

Annual Report 2019-20 1. the Principal's
Annual Report 2019-20 This format outlines the annual reports to be published by all colleges in the Madhya Pradesh st on their websites, by October 31 of each year. Part I is intended as a guide and colleges are free to alter the contents and format as they see fit. Part II, the Appendix (Institutional Performance Data and Financial Reports), is mandatory and colleges are required to report all data as per the attached format and instructions. Important Information – Name of the college – GOVT.P.G.COLLEGE REHLI DISTT- SAGAR Place of the college – TEHSIL REHLI District - SAGAR(M.P.) Division - SAGAR(M.P.) Year of establishment of college - 1983 Name and Contact details( Mail id , Phone ) of Principal – Mr. A.K. JAIN , Name , Post and Contact details of ( mail id, Phone no.) of Reporting In charge – 07585-256253, 9425626991, [email protected] Date of report submission - Part I 1. The Principal’s Report (2 pages)- Highlights the key activities, events, and successes of the past year and briefly describes major new initiatives to be undertaken over the next year. Government P.G. College Rehli, Sagar started its journey in 1983. The college grew out of the efforts of Dr. G.C.Singhai who believed in and promoted education for the local people in the field of higher education. At the time of its inception, UG Arts classes were conducted in the college ,later in 2005, B.Sc /M.A in 4 subjects was started to meet the needs of the weaker and backward Section of the society. -

LIST of DEPLOYED EXPENDITURE OBSERVERS - Madhya Pradesh 18-Mar-2014 7:57 Pm
LIST OF DEPLOYED EXPENDITURE OBSERVERS - Madhya Pradesh 18-Mar-2014 7:57 pm SL.NO OBSERVER NAME AC-NAME &No. SERVICE CADRE YEAR HOME OFFICE DEPLOYED DEPLOYED DEPLOYED DEPLOYED DEPLOYED CODE STATE STATE STATE From To From To G K Pati 1-SHEOPUR 1 R-18600 IC&CES 2008 Orissa Orissa Madhya 19-Mar-2014 17-Apr-2014 15-Jun-2014 22-Jun-2014 [Sheopur],2-VIJAYP UR Pradesh [Sheopur],3-SABALA GADH [Morena],4-JAURA[M orena],5-SUMAOLI[ Morena],7-DIMANI [Morena],6-MORENA [Morena],8-AMBAH [Morena] Gaurav Sinha 9-ATER 2 R-14786 IC&CES 1998 Uttar West Madhya 19-Mar-2014 17-Apr-2014 15-Jun-2014 22-Jun-2014 [Bhind],10-BHIND Pradesh Bengal [Bhind],11-LAHAR Pradesh [Bhind],12-MEHGAO N[Bhind],22-DATIA[D atia],20-SEWDA[Dati a],13-GOHAD [Bhind],21-BHANDE R [Datia] Harkirpal 14-GWALIOR 3 R-18677 IC&CES 2009 Himach Punjab Madhya 19-Mar-2014 17-Apr-2014 15-Jun-2014 22-Jun-2014 Khatana RURAL[Gwalior],16- al GWALIOR EAST Pradesh Pradesh [Gwalior],19-DABAR A [Gwalior],24-POHAR I [Shivpuri],17-GWALI OR SOUTH[Gwalior],15- GWALIOR[Gwalior], 18-BHITRWAR[Gwal ior],23-KARERA [Shivpuri] Page 1 of 9 SL.NO OBSERVER NAME AC-NAME &No. SERVICE CADRE YEAR HOME OFFICE DEPLOYED DEPLOYED DEPLOYED DEPLOYED DEPLOYED CODE STATE STATE STATE From To From To Himanshu Raina 27-KOLARAS 4 R-18678 IC&CES 2009 Uttarakh NCT OF Madhya 19-Mar-2014 17-Apr-2014 15-Jun-2014 22-Jun-2014 [Shivpuri],29-GUNA and Delhi [Guna],33-CHANDE Pradesh RI[Ashok Nagar],25-SHIVPUR I[Shivpuri],34-MUNG AOLI[Ashok Nagar],32-ASHOK NAGAR [Ashok Nagar],26-PICHHO RE[Shivpuri],28-BAM ORI [Guna] Istikhar Baig 36-KHURAI 5 R-18679 -

Madhya Pradesh Size:( 5.5
37th Meeting of the Central Sanctioning cum Monitoring Committee(CSMC) under Pradhan Mantri Awas Yojana - Housing For All rd Urban Development & Housing Department 23 August, 2018 Government of Madhya Pradesh Indicators Current Status (No.) . Cities Approved 378 . Demand Survey Completed 378 . Total Demand 11.52 Lakh . Demand received through Common Service Centre 4,44,606 and Online Application . Cases accepted/rejected 2,07,397 . Whether HFAPoA Submitted Yes, For all 378 Towns . Whether AIP Submitted Yes 10,49,665 Surveyed Data Entries have been entered in PMAY . Whether HFAPoA & AIP entered in MIS MIS . SLTC/CLTC staffs approved vs. placed SLTC:10 vs 10 / CLTC: 454 vs 521 Sanctioning: 2.47 Lakh DUs (Excluding CLSS) . Target of DUs in 2018-19 Completion: 5.00 Lakh DUs As per provision of GoI matching budgetary provisions is . State Budgetary Provision for PMAY (U) in 2018-19 ensured in state budget 2 Indicators Current Status (No.) .Survey entry made (%) 87.60% .Projects approved: 887 .Projects entered (7A/B/C/D) 851 .DUs approved under BLC 3,47,242 (Excluding 35,475 Surrendered DUs) .Beneficiaries attached 3,04,186 .Geo-tagged Points 6,77,539 (No. of Unique Houses Geo-Tagged: 2,56,075) 3 Grounded for Construction / In-Progress EWS Work Verticals Houses Tendered Order Completed Approved Issued Foundation Lintel Roof Total AHP 1,49,645 48,499 1,01,146 58,816 18,643 5,748 83,207 17,939 (Including RAY) BLC (N) 3,47,242 - - 1,24,110 26,775 18,767 1,69,652 97,313 ISSR 2,172 960 - - - - - - CLSS 11,616 - - - - - - 11,616 (Including LIG/MIG) -

Regional Weather Inference and Forecast Morning Meteorological Analysis (Based on 0830 Hrs IST Observations)
Bादेिशक मौसम पूवानुमान केJ Regional Weather Forecasting Centre Bादेिशक मौसम केJ Regional Meteorological Centre भारत मौसम िवBान िवभाग India Meteorological Department नागपुर Nagpur ________________________________________________________________________________________________ Regional Weather Inference And Forecast Saturday, 26 August 2017 Morning Issue Time : 11.30 Hrs. IST Meteorological Analysis (Based on 0830 Hrs IST Observations) Weather Watch :-. Heavy rainfall occurred at isolated places over Madhya Pradesh. Thunderstorm observed at isolated places over Vidarbha, Chhattisgarh and Madhya Pradesh. Very light to moderate rainfall occurred at many places over Vidarbha, Chhattisgarh and Madhya Pradesh. Monsoon Watch :- NIL Inference:- The axis of monsoon trough at mean sea level now passes through Ganganagar, Karnal, Lucknow, Daltonganj and Puri and thence southeastwards to eastcentral Bay of Bengal and extends upto 0.9 Km above mean sea level. A cyclonic circulation upto 4.5 km above mean sea level lies over northwest Bay of Bengal off north Odisha¬West Bengal coasts. Under the influence the above two systems, a low pressure area is likely to form over northwest Bay of Bengal & neighbourhood during next 24 hours. An east-west shear zone runs roughly along Latitude 15°Nbetween 5.8 & 7.6 km above mean sea level. The upper air cyclonic circulation over north Chhattisgarh & neighbourhood now lies over Northeast Madhya Pradesh and neighbourhood between 1.5 & 5.8 km above mean sea level tilting southwestwards with height. The Western disturbance as an upper air cyclonic circulation over north Pakistan & adjoining Jammu & Kashmir now lies over Jammu & Kashmir and neighbourhood between 3.1 km & 5.8 Km above mean sea level. -

Portrait of Population Madhya Pradesh
CENSUS OF INDIA, 1981 A PORTRAIT OF POPULATION MADHYA PRADESH Draft by M. L. SHARMA Deputy Director and M. G. MOHRIL .A ssistant Director DIRECTORATE OF CENSUS OPERATIONS MADHYA PRADESH BHOPAL (iii) ,,' 7f ,,' eI MADHYA PRADESH ADMINISTRATIVE DIVISIONS 1981 . " ,,' ..! DiStRICT HEAOI)UART~RS 'AHSILH(,I,OQUAATERS. t,Whlllll1t MI'IIt Gl dlltrict or tahilidillirl fr'Om tht n~lI\tm d~ ~rag~uQrtm or 1M tahiti IltQdqulrter, It hal bun ~ho\l'rt . wll~,ft bracklls thU1 (BASTAR) (Gira) 0 ..Z ~ ri e , ltuttr ~fiI " 114+16r 4ltlrid $ o",Arta klolotl to Cttio talilil 01 0Il1/t 'Utrltk II J .. Arft klo"ll• .!ttlJQiltlll' t'~lil, I I 3 so· I MADHYA PRADESH COMMUNICATIONS . , . " ,t ,f ~ , A\ \ ~ IOUNDm,SUTE ;8 OISHICI H~~ll SUTE miTAl .. UILVAY, iMAOGAU.f • IIEHEmU. NHMWmH. lOAD, NATlml~I;IIWAY .. STAlE Hr,HvAY KI[OMEHfS 32 0 32 64 96 121160 .Shontr; t~III1I.1 ~Illior dhlii(t. I LJ .iOL:J;o;;;oi . ArlO \,Io~ .. t. {)QIIQ \Qhsil Qt OI\iQ dil\ri,t, " Auo biron" 10 ~O~~oI9~r tQ~,11 (v) J(b)-364 R.G. Illllia/NDl 88 (vii) '''l i .f' z ~ % i til .'\' III 0 4 ...c ti: a:: ..::> G. • 4 ~ ... ~ % c cI 0 I-e 2 4 1&1 S; "/.,I&. k 0 0 0 c c 0 0 0 0 0 $ S $ 4 en ... 8 ~ ... ,.. ~ .. - :J IX ~ ... ... N ~ (J\ .. - . (000100 ~I ) I. Z ~e 0 - :~~ , ~ ""..J ..... 4 ~ ~ A- S 0 ..• a. :> I t ~ '> ~ I -0 Z .... :; -.. ;.~ ...0 ~~~ 0 0 0 0 0 0 0 0 c 0 0 0 0 0 0 0 0 CD S 0 CD ID 04 0 ~ ~ N N N ~ ~ .. -

Local Government Directory
Local Government Directory All Villages of Rehli Subdistrict, SAGAR district, MADHYA PRADESH state S.No. State State Name (In District District Name Sub- Sub-District Village Village Village Name Village Name Census Census Code English) Code (In English) District Name (In Code Version (In Englsih) (In Local) 2001 2011 Code English) Code Code 1 23 MADHYA 425 SAGAR 3451 Rehli 461116 1 Achalpur 01200900 461116 PRADESH 2 23 MADHYA 425 SAGAR 3451 Rehli 461184 1 Akla 01207700 461184 PRADESH 3 23 MADHYA 425 SAGAR 3451 Rehli 461198 1 Ankhi Khera 01209100 461198 PRADESH 4 23 MADHYA 425 SAGAR 3451 Rehli 461185 1 Babupura 01207800 461185 PRADESH 5 23 MADHYA 425 SAGAR 3451 Rehli 461154 1 Badarchuwan 01204700 461154 PRADESH 6 23 MADHYA 425 SAGAR 3451 Rehli 461100 1 Badgaon 01199300 461100 PRADESH 7 23 MADHYA 425 SAGAR 3451 Rehli 461172 1 Bagaspura 01206500 461172 PRADESH 8 23 MADHYA 425 SAGAR 3451 Rehli 461088 1 Bagraon 01198100 461088 PRADESH 9 23 MADHYA 425 SAGAR 3451 Rehli 461128 1 Baidwara 01202100 461128 PRADESH 10 23 MADHYA 425 SAGAR 3451 Rehli 461166 1 Bamurakunj 01205900 461166 PRADESH 11 23 MADHYA 425 SAGAR 3451 Rehli 461094 1 Barkhera 01198700 461094 PRADESH 12 23 MADHYA 425 SAGAR 3451 Rehli 461139 1 Barkhera Jagan 01203200 461139 PRADESH 13 23 MADHYA 425 SAGAR 3451 Rehli 461178 1 Barkheri 01207100 461178 PRADESH Sikandar 14 23 MADHYA 425 SAGAR 3451 Rehli 461199 1 Barkoti 01209200 461199 PRADESH Jun 22, 2019, 2:19 PM S.No. State State Name (In District District Name Sub- Sub-District Village Village Village Name Village Name Census Census -

Journal Volume 16 2020 Final
A DOUBLE BLIND PEER REVIEWED JOURNAL OF APG AND ISPER INDIA INDEXED IN SCOPUS VOLUME 16 ISSN- 0973–3485 OCTOBER 2020 PUNJAB GEOGRAPHER : ISSN- 0973–3485 Volume 16 October 2020 INFRASTRUCTURAL DEVELOPMENT IN BUNDELKHAND REGION: A MICRO-LEVEL ANALYSIS P. K. Sharma Abstract Infrastructure development is one of the driving forces to attain swift economic growth. It plays an important role in the reduction of poverty, improvements in standard of living and leads to sustained development of a region. This study is an attempt to analyse the micro- regional disparities in infrastructural development across 40 blocks of Bundelkhand region of Madhya Pradesh. The study is based on secondary sources of data, obtained from various government agencies for the year, 2011. In order to find out the level of infrastructural development, composite score method has been used by considering 12 variables at the block level. The study reveals widespread micro-regional infrastructural disparity, ranging from highest score of 1.34 for Nowgong block to lowest of -0.95 for Buxwaha block. On the basis of Principal Component Analysis, four dominant factors governing the level of infrastructural development in the region have been identified. These key factors may be addressed on priority basis to enhance the living condition of the people and to reduce micro regional disparities. Keywords: Infrastructure, Bundelkhand, Development, Disparities, Region, Facilities. Introduction condition for the overall development of a In the long path of planned region (Bagchi, 2017). The better infra- development in India, wide spread regional structure provides better living conditions and disparities are still one of the major concerns easy availability of services to the public. -

EXECUTIVE SUMMARY Development of an Integrated MSW Processing and Disposal Facility at Sagar by Saagar MSW Solutions Pvt
Development of an Integrated MSW Processing and Disposal Facility at Sagar by Saagar MSW Solutions Pvt. Ltd. Executive Summary EXECUTIVE SUMMARY Development of an Integrated MSW Processing and Disposal Facility at Sagar by Saagar MSW Solutions Pvt. Ltd. 1. Executive Summary The current Municipal Solid Waste (MSW) management system in Sagar town and ten (10) other surrounding Urban Local Bodies, ULBs (Makronia, Banda, Khurai, Rehli, Grahakota, Bina, Deori, Rahatgarh, Shahgarh and Shahpur) currently does not comply with MSW (Management and Handling) Rules, 2000 and subsequent amendments. Government of Madhya Pradesh (GoMP), realizing the necessity of efficient waste management system, wanted to establish an Integrated MSW processing and Disposal Facility on Public Private Partnership (PPP) basis for management of MSW generated in Sagar Town and 10 other surrounding ULBs. “Saagar MSW Solutions Private Limited (SMSWSPL)” (Project Proponent ) was chosen for establishing an Integrated MSW Processing and Disposal Facility in Sagar town. Currently, Sagar Town along with 10 other ULBs generate an average MSW of 180 TPD. All the 10 participating ULBs are within 75 km radius of Sagar Town. Considering the population projection, the Project Proponent proposes to establish a 350 TPD Integrated MSW Processing and Disposal Facility in Sagar Town with facilities such as Composting/Dry Fermentation (for recovery of organics), Materials Recovery Facility (for recovery of recyclables), Refuse Derived Fuel (RDF) facility for recovery of high calorific value waste, Secured Landfill (for disposal of inerts) and Incinerator for leachate treatment/disposal, RDF disposal, and for animal carcass. The proposed Integrated Waste Management Facility will be established in a land of about 10.50 hectares located within Sagar town. -
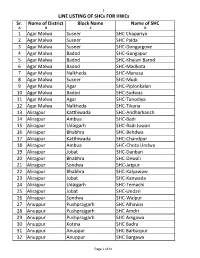
HWC-SHC Allotment List for CCCH
1 LINE LISTING OF SHCs FOR HWCs Sr. Name of District Block Name Name of SHC A B C D 1 Agar Malwa Susner SHC Chapariya 2 Agar Malwa Susner SHC Palda 3 Agar Malwa Susner SHC-Dongargove 4 Agar Malwa Badod SHC-Gangapur 5 Agar Malwa Badod SHC-Khajuri Barod 6 Agar Malwa Badod SHC-Madkota 7 Agar Malwa Nalkheda SHC-Manasa 8 Agar Malwa Susner SHC-Modi 9 Agar Malwa Agar SHC-Piplonkalan 10 Agar Malwa Badod SHC-Sudwas 11 Agar Malwa Agar SHC-Tanodiya 12 Agar Malwa Nalkheda SHC-Tikona 13 Alirajpur Katthiwada SHC-Andharkanch 14 Alirajpur Ambua SHC-Badi 15 Alirajpur Udaigarh SHC-Badi Juwari 16 Alirajpur Bhabhra SHC-Behdwa 17 Alirajpur Katthiwada SHC-Chandpur 18 Alirajpur Ambua SHC-Chota Undwa 19 Alirajpur Jobat SHC-Danbari 20 Alirajpur Bhabhra SHC-Dewali 21 Alirajpur Sondwa SHC-Jetpur 22 Alirajpur Bhabhra SHC-Kalyawaw 23 Alirajpur Jobat SHC-Kanwada 24 Alirajpur Udaigarh SHC-Temachi 25 Alirajpur Jobat SHC-Undari 26 Alirajpur Sondwa SHC-Walpur 27 Anuppur Pushprajgarh SHC Alhawar 28 Anuppur Pushprajgarh SHC Amdri 29 Anuppur Pushprajgarh SHC Amgawa 30 Anuppur Kotma SHC Badra 31 Anuppur Anuppur SHC Barbaspur 32 Anuppur Anuppur SHC Bargawa Page 1 of 41 2 LINE LISTING OF SHCs FOR HWCs Sr. Name of District Block Name Name of SHC 33 Anuppur Jaithari SHC Beend 34 Anuppur Kotma SHC Beiharbandh 35 Anuppur Pushprajgarh SHC Bilaspur 36 Anuppur Kotma SHC Chaka 37 Anuppur Jaithari SHC Choi 38 Anuppur Jaithari SHC Chorbhdhi 39 Anuppur Jaithari SHC Chulha 40 Anuppur Kotma SHC Dhangawa 41 Anuppur Pushprajgarh SHC Gonda 42 Anuppur Jaithari SHC Gorshi 43 Anuppur Anuppur