Characterization of Human TRPA1 and TRPV1 Channels in Response to Naturally Occurring Defensive Compounds
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Intestinal Anti-Inflammatory Activity of Terpenes in Experimental Models
molecules Review Intestinal Anti-Inflammatory Activity of Terpenes in Experimental Models (2010–2020): A Review Maria Elaine Araruna 1, Catarina Serafim 1, Edvaldo Alves Júnior 1, Clelia Hiruma-Lima 2, Margareth Diniz 1,3 and Leônia Batista 1,3,* 1 Postgraduate Program in Natural Products and Bioactive Synthetic, Health Sciences Center, Federal University of Paraiba, João Pessoa 58051-900, PB, Brazil; [email protected] (M.E.A.); [email protected] (C.S.); [email protected] (E.A.J.); [email protected] (M.D.) 2 Department of Structural and Functional Biology (Physiology), Institute of Biosciences, São Paulo State University, Botucatu 18618-970, SP, Brazil; [email protected] 3 Department of Pharmacy, Health Sciences Center, Federal University of Paraíba, João Pessoa 58051-900, PB, Brazil * Correspondence: [email protected]; Tel.: +55-83-32167003; Fax: +55-83-32167502 Academic Editors: Maurizio Battino, Jesus Simal-Gandara and Esra Capanoglu Received: 8 September 2020; Accepted: 28 September 2020; Published: 20 November 2020 Abstract: Inflammatory bowel diseases (IBDs) refer to a group of disorders characterized by inflammation in the mucosa of the gastrointestinal tract, which mainly comprises Crohn’s disease (CD) and ulcerative colitis (UC). IBDs are characterized by inflammation of the intestinal mucosa, are highly debilitating, and are without a definitive cure. Their pathogenesis has not yet been fully elucidated; however, it is assumed that genetic, immunological, and environmental factors are involved. People affected by IBDs have relapses, and therapeutic regimens are not always able to keep symptoms in remission over the long term. Natural products emerge as an alternative for the development of new drugs; bioactive compounds are promising in the treatment of several disorders, among them those that affect the gastrointestinal tract, due to their wide structural diversity and biological activities. -
Anza-Borrego Desert State Park Bibliography Compiled and Edited by Jim Dice
Steele/Burnand Anza-Borrego Desert Research Center University of California, Irvine UCI – NATURE and UC Natural Reserve System California State Parks – Colorado Desert District Anza-Borrego Desert State Park & Anza-Borrego Foundation Anza-Borrego Desert State Park Bibliography Compiled and Edited by Jim Dice (revised 1/31/2019) A gaggle of geneticists in Borrego Palm Canyon – 1975. (L-R, Dr. Theodosius Dobzhansky, Dr. Steve Bryant, Dr. Richard Lewontin, Dr. Steve Jones, Dr. TimEDITOR’S Prout. Photo NOTE by Dr. John Moore, courtesy of Steve Jones) Editor’s Note The publications cited in this volume specifically mention and/or discuss Anza-Borrego Desert State Park, locations and/or features known to occur within the present-day boundaries of Anza-Borrego Desert State Park, biological, geological, paleontological or anthropological specimens collected from localities within the present-day boundaries of Anza-Borrego Desert State Park, or events that have occurred within those same boundaries. This compendium is not now, nor will it ever be complete (barring, of course, the end of the Earth or the Park). Many, many people have helped to corral the references contained herein (see below). Any errors of omission and comission are the fault of the editor – who would be grateful to have such errors and omissions pointed out! [[email protected]] ACKNOWLEDGEMENTS As mentioned above, many many people have contributed to building this database of knowledge about Anza-Borrego Desert State Park. A quantum leap was taken somewhere in 2016-17 when Kevin Browne introduced me to Google Scholar – and we were off to the races. Elaine Tulving deserves a special mention for her assistance in dealing with formatting issues, keeping printers working, filing hard copies, ignoring occasional foul language – occasionally falling prey to it herself, and occasionally livening things up with an exclamation of “oh come on now, you just made that word up!” Bob Theriault assisted in many ways and now has a lifetime job, if he wants it, entering these references into Zotero. -
Bilirubin: an Animal Pigment in the Zingiberales and Diverse Angiosperm Orders Cary L
Florida International University FIU Digital Commons FIU Electronic Theses and Dissertations University Graduate School 11-5-2010 Bilirubin: an Animal Pigment in the Zingiberales and Diverse Angiosperm Orders Cary L. Pirone Florida International University, [email protected] DOI: 10.25148/etd.FI10122201 Follow this and additional works at: https://digitalcommons.fiu.edu/etd Part of the Biochemistry Commons, and the Botany Commons Recommended Citation Pirone, Cary L., "Bilirubin: an Animal Pigment in the Zingiberales and Diverse Angiosperm Orders" (2010). FIU Electronic Theses and Dissertations. 336. https://digitalcommons.fiu.edu/etd/336 This work is brought to you for free and open access by the University Graduate School at FIU Digital Commons. It has been accepted for inclusion in FIU Electronic Theses and Dissertations by an authorized administrator of FIU Digital Commons. For more information, please contact [email protected]. FLORIDA INTERNATIONAL UNIVERSITY Miami, Florida BILIRUBIN: AN ANIMAL PIGMENT IN THE ZINGIBERALES AND DIVERSE ANGIOSPERM ORDERS A dissertation submitted in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY in BIOLOGY by Cary Lunsford Pirone 2010 To: Dean Kenneth G. Furton College of Arts and Sciences This dissertation, written by Cary Lunsford Pirone, and entitled Bilirubin: An Animal Pigment in the Zingiberales and Diverse Angiosperm Orders, having been approved in respect to style and intellectual content, is referred to you for judgment. We have read this dissertation and recommend that it be approved. ______________________________________ Bradley C. Bennett ______________________________________ Timothy M. Collins ______________________________________ Maureen A. Donnelly ______________________________________ John. T. Landrum ______________________________________ J. Martin Quirke ______________________________________ David W. Lee, Major Professor Date of Defense: November 5, 2010 The dissertation of Cary Lunsford Pirone is approved. -
2010 Season Summary Index NEW WOFTHE~ Zone 1: Yukon Territory
2010 Season Summary Index NEW WOFTHE~ Zone 1: Yukon Territory ........................................................................................... 3 Alaska ... ........................................ ............................................................... 3 LEPIDOPTERISTS Zone 2: British Columbia .................................................... ........................ ............ 6 Idaho .. ... ....................................... ................................................................ 6 Oregon ........ ... .... ........................ .. .. ............................................................ 10 SOCIETY Volume 53 Supplement Sl Washington ................................................................................................ 14 Zone 3: Arizona ............................................................ .................................... ...... 19 The Lepidopterists' Society is a non-profo California ............... ................................................. .............. .. ................... 2 2 educational and scientific organization. The Nevada ..................................................................... ................................ 28 object of the Society, which was formed in Zone 4: Colorado ................................ ... ............... ... ...... ......................................... 2 9 May 1947 and formally constituted in De Montana .................................................................................................... 51 cember -

Nutritional and Medicinal Properties of Solanaceous Vegetables Shilpa Devi and Arvind Nagar Division of Vegetable Science, IARI, New Delhi, 110012
Shilpa Devi and Arvind Nagar Your full article ( between 500 to 5000 words) - - Do check for grammatical errors or spelling mistakes Nutritional and Medicinal Properties of Solanaceous Vegetables Shilpa Devi and Arvind Nagar Division of vegetable Science, IARI, New Delhi, 110012 Corresponding mail- [email protected] Introduction The family Solanaceae, or nightshades, is an economically important family of flowering plants. The family ranges from annual and perennial herbs to vines, or either shrubs, and trees, including a number of important vegetable crops like tomato, pepper, eggplant, white and red potato, and tomatillo. This family also contains several plants that are considered toxic to humans being such as the weeds jimsonweed, nightshade and mandrake. Many members of the family contain potent alkaloids that are having immense value by considering its nutritional value. The family belongs to the order Solanales, in the asterid group dicotyledons (Magnoliopsida). The solanaceae consists of approximately 98 genera and about 2,700 species, with a great diversity in their habitats, morphology and ecology. Worldwide 53% of children are malnourished and underweight with 40% of them living in India. Solanaceous vegetable crops are important source of vitamin C, A, E, thiamine, niacin, pyridoxine, folacin, minerals and dietry fibres which play a significant role in human nutrition and helps to cope with malnutrition. Nutritional and Medicinal Properties of Tomato Tomatoes are the 2nd highly produced and consumed vegetable in the world today. Tomato is consumed either fresh or in many processed forms like ketchup, canned whole or in pieces, puree, sauce, soup, juice, or sun- dried. Tomato fruits are considered a low energy dense food with unique constituents that may positively affect health. -

Effect of Prebiotic Supplementation on Performance and Health of Dairy Calves: Protocol for a Systematic Review and Meta-Analysis R
Effect of prebiotic supplementation on performance and health of dairy calves: protocol for a systematic review and meta-analysis R. B. Lopes1, E. D. Fausak1, C. Bernal-Córdoba1, N. Silva-del-Río1* 1University of California Davis, US; [email protected] (RBL); [email protected] (EDF); [email protected] (CBC); [email protected] (NSDR) *Corresponding author: Veterinary Medicine Teaching and Research Center, University of California Davis, 18830 Road 112, Tulare, CA, 93274, Phone: 559-688-1731, Fax: 559-686- 4231. Author Contributions: RBL: Assist to develop search strategy and literature search, data screening, extraction, statistical analysis, and protocol and manuscript preparation. EDF: Develop search strategy and literature search, edit protocol. CBC: Data screening, review data extraction, review protocol and manuscript. NSDR: Assist, edit and review protocol and manuscript. Amendments: Any amendments to this protocol will be documented and justified in the final review. Support: This study is financially supported by the California Department of Food and Agriculture (CDFA) and it is part of the Antimicrobial Use and Stewardship (AUS) program. INTRODUCTION Rationale In the dairy industry, the treatment of sick calves is commonly based on the antibiotic use by systematic therapy or addition into the milk (Foutz et al., 2018; Urie et al., 2018). The overuse and misuse of antibiotics contribute to the development of antimicrobial resistance, which is a threat to both animal and human health. Thus, it is fundamental to investigate preventative strategies, such as prebiotics, to reduce the incidence of diseases and consequently the use of antibiotics. According to the International Scientific Association for Probiotics and Prebiotics, prebiotic is a “substrate that is selectively utilized by host microorganisms conferring a health benefit” (Gibson et al., 2017). -

Natural Products (Secondary Metabolites)
Biochemistry & Molecular Biology of Plants, B. Buchanan, W. Gruissem, R. Jones, Eds. © 2000, American Society of Plant Physiologists CHAPTER 24 Natural Products (Secondary Metabolites) Rodney Croteau Toni M. Kutchan Norman G. Lewis CHAPTER OUTLINE Introduction Introduction Natural products have primary ecological functions. 24.1 Terpenoids 24.2 Synthesis of IPP Plants produce a vast and diverse assortment of organic compounds, 24.3 Prenyltransferase and terpene the great majority of which do not appear to participate directly in synthase reactions growth and development. These substances, traditionally referred to 24.4 Modification of terpenoid as secondary metabolites, often are differentially distributed among skeletons limited taxonomic groups within the plant kingdom. Their functions, 24.5 Toward transgenic terpenoid many of which remain unknown, are being elucidated with increas- production ing frequency. The primary metabolites, in contrast, such as phyto- 24.6 Alkaloids sterols, acyl lipids, nucleotides, amino acids, and organic acids, are 24.7 Alkaloid biosynthesis found in all plants and perform metabolic roles that are essential 24.8 Biotechnological application and usually evident. of alkaloid biosynthesis Although noted for the complexity of their chemical structures research and biosynthetic pathways, natural products have been widely per- 24.9 Phenylpropanoid and ceived as biologically insignificant and have historically received lit- phenylpropanoid-acetate tle attention from most plant biologists. Organic chemists, however, pathway metabolites have long been interested in these novel phytochemicals and have 24.10 Phenylpropanoid and investigated their chemical properties extensively since the 1850s. phenylpropanoid-acetate Studies of natural products stimulated development of the separa- biosynthesis tion techniques, spectroscopic approaches to structure elucidation, and synthetic methodologies that now constitute the foundation of 24.11 Biosynthesis of lignans, lignins, contemporary organic chemistry. -

Download Download
Journal of International Society for Food Bioactives Nutraceuticals and Functional Foods Review J. Food Bioact. 2020;10:32–46 Chemistry and biochemistry of dietary carotenoids: bioaccessibility, bioavailability and bioactivities Cheng Yanga,b, Lianfu Zhanga,b and Rong Tsaoc* aState Key Laboratory of Food Science and Technology, Jiangnan University, 1800 Lihu Avenue, Wuxi, Jiangsu, 214122, China bSchool of Food Science and Technology, Jiangnan University, 1800 Lihu Avenue, Wuxi, Jiangsu, 214122, China cGuelph Research and Development Centre, Agriculture and Agri-Food Canada, 93 Stone Road West, Guelph, Ontario N1G 5C9, Canada *Corresponding author: Rong Tsao, Guelph Research and Development Centre, Agriculture and Agri-Food Canada, 93 Stone Road West, Guelph, Ontario N1G 5C9, Canada. Tel: +1 226 217 8180. Fax: +1 226 217 8183. E-mail: [email protected] DOI: 10.31665/JFB.2020.10225 Received: April 10, 2020; Revised received & accepted: June 26, 2020 Citation: Yang, C., Zhang, L., and Tsao, R. (2020). Chemistry and biochemistry of dietary carotenoids: bioaccessibility, bioavailability and bioactivities. J. Food Bioact. 10: 32–46. Abstract Carotenoids are one of the major food bioactives that provide humans with essential vitamins and other critically important nutrients that contribute to the maintenance of human health. This review provides a summary of the most current literature data and information on most recent advances in dietary carotenoids and human health research. Specifically, it addresses the occurrence and distribution of carotenoids in different dietary sources, the effect of food processing and impact of gastrointestinal digestion on the bioaccessibility, bioavailability and bioac- tivities of dietary carotenoids. Emphasis is placed on the antioxidant and anti-inflammatory effects of carotenoids and their optical/geometric isomers and ester forms, and the molecular mechanisms behind these actions. -

Carotene, Lutein, and Zeaxanthin in Eye Health and Disease
antioxidants Review A Mechanistic Review of β-Carotene, Lutein, and Zeaxanthin in Eye Health and Disease Fatima Tuj Johra, Asim Kumar Bepari , Anika Tabassum Bristy and Hasan Mahmud Reza * Department of Pharmaceutical Sciences, School of Health and Life Sciences, North South University, Bashundhara R/A, Dhaka 1229, Bangladesh; [email protected] (F.T.J.); [email protected] (A.K.B.); [email protected] (A.T.B.) * Correspondence: [email protected]; Tel.: +880-255668200 (ext. 1954) Received: 12 September 2020; Accepted: 22 October 2020; Published: 26 October 2020 Abstract: Carotenoids are natural lipid-soluble antioxidants abundantly found as colorful pigments in fruits and vegetables. At least 600 carotenoids occur naturally, although about 20 of them, including β-carotene, α-carotene, lycopene, lutein, zeaxanthin, meso-zeaxanthin, and cryptoxanthin, are detectable in the human blood. They have distinct physiological and pathophysiological functions ranging from fetal development to adult homeostasis. β-carotene is a precursor of vitamin A that essentially functions in many biological processes including vision. The human macula lutea and eye lens are rich in lutein, zeaxanthin, and meso-zeaxanthin, collectively known as macular xanthophylls, which help maintain eye health and prevent ophthalmic diseases. Ocular carotenoids absorb light from the visible region (400–500 nm wavelength), enabling them to protect the retina and lens from potential photochemical damage induced by light exposure. These natural antioxidants also aid in quenching free radicals produced by complex physiological reactions and, consequently, protect the eye from oxidative stress, apoptosis, mitochondrial dysfunction, and inflammation. This review discusses the protective mechanisms of macular xanthophylls in preventing eye diseases such as cataract, age-related macular degeneration, and diabetic retinopathy. -

Epoxidation of Terpenes with Molecular Catalysts in Homogeneous Phase
Technische Universität München Lehrstuhl für Molekulare Katalyse Epoxidation of Terpenes with Molecular Catalysts in Homogeneous Phase Typhène Michel Vollständiger Abdruck der von der Fakultät für Chemie der Technischen Universität München zur Erlangung des akademischen Grades eines Doktors der Naturwissenschaften genehmigten Dissertation. Vorsitzende: Univ. – Prof. Dr. K. Köhler Prüfer der Dissertation: 1. Univ. – Prof. Dr. F. E. Kühn 2. Univ. – Prof. Dr. V. Sieber Die Dissertation wurde am 22.10.2012 bei der Technischen Universität München eigereicht und durch die Fakultät für Chemie am 26.11.2012 angenommen. A mes parents, mon frère, ma sœur et mes amis Toute action naturelle est engendrée par la nature, de la plus courte façon que l’on puisse trouver. Human subtlety… will never devise an invention more beautiful, more simple or more direct than does nature, because in her inventions nothing is lacking, and nothing is superfluous. Leonardo da Vinci Die vorliegende Arbeit entstand in der Zeit von Oktober 2009 bis Oktober 2012 am Anorganisch-chemischen Institute der Technischen Universität München I would like to express my deep gratitude to my academic supervisor Prof. Dr. Fritz E. Kühn For his continuous supervision, encouragement and trust in my work. Acknowledgements I will first address my most sincere thanks to Prof. F. E. Kühn for allowing me to perform my PhD in his groups, for his trust in my research and his advices and to Dr. Mirza Cokoja, for his scientific advices and continuous help during my PhD on correcting my manuscripts. Fraunhofer Institut and Prof. V. Sieber are acknowledged for their financial support. I heartily thank my family: my parents, my sister (Alison) and my brother (Clément) for their continuous love and encouragement throughout my studies and my personal life. -

Functional Foods: Overview Functional Foods: Dietary Fibers, Prebiotics, Probiotics, and Synbiotics Nutrition: Soy-Based Foods
NUTRITION AND FOOD GRAINS Food Grains and Well-Being Contents Functional Foods: Overview Functional Foods: Dietary Fibers, Prebiotics, Probiotics, and Synbiotics Nutrition: Soy-Based Foods Functional Foods: Overview G Bultosa, Botswana College of Agriculture, Gaborone, Botswana; Haramaya University, Dire Dawa, Ethiopia ã 2016 Elsevier Ltd. All rights reserved. Topic Highlights Consumption of an adequately balanced diet is a means of body structure formation, energy generation, and health. More • Functional food concepts/definitions. than 2500 years ago, ‘Let foods be our medicine and medicine • Bioactive compounds. be our foods’ was stated by Hippocrates. This shows that • Chronic diseases and functional foods. consumption of diets with health-promoting effects is not • Gluten-free foods for celiac patients. new. But evidence on the relationship between dietary chem- ical component(s) and health is on evolutionary development as technology and human comprehension advance. Within Learning Objectives such evolution, the concept of functional foods was started in the 1980s as Foods for Specified Health Use (FOSHU) • To achieve understanding on the concepts/definitions of in Japan. Foods, when consumed as a regular diet that supplies functional foods. one or more bioactive components beyond basic nutrients and • To achieve understanding of bioactive compounds used in offer health-promoting effects, are today branded as functional functional foods, grain dietary sources, and potential effects foods. Functional foods are not prescribed drugs, dietary sup- on health. plements, medical foods of therapeutic effects, traditional • To impart processing principles on grain-based functional medicines, or nutraceuticals. Functional foods are distinct foods. from macronutrient and micronutrient supplements targeted to achieve balanced diets and to treat nutrient deficiency syn- dromes. -
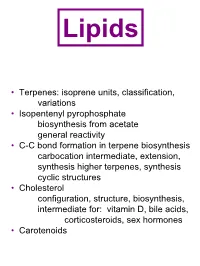
• Terpenes: Isoprene Units, Classification, Variations
Lipids • Terpenes: isoprene units, classification, variations • Isopentenyl pyrophosphate biosynthesis from acetate general reactivity • C-C bond formation in terpene biosynthesis carbocation intermediate, extension, synthesis higher terpenes, synthesis cyclic structures • Cholesterol configuration, structure, biosynthesis, intermediate for: vitamin D, bile acids, corticosteroids, sex hormones • Carotenoids Steroids C D A B H H H HO cholesterol From diet, but can also synthesize from… acetate!! Terpenes: The Isoprene Rule Terpenes and terpenoids are the most important constituents in essential oils Terpenes are built from C5 isoprene units CH3 C CH2 = H2C C H Isoprene (2-methyl-1,3-butadiene) Isoprene units are linked head-to-tail tail head Terpenes are repeating isoprene units Classified according to the number of isoprene units they contain Class # Isoprene units # C atoms Monoterpene 2 10 Sesquiterpene 3 15 Diterpene 4 20 Sesterpene 5 25 Triterpene 6 30 Tetraterpene 8 40 Terpenes may be substituted, cyclic, or linked tail-to-tail OH Farnesol (terpenoid) OH Limonene Menthol (from lemon or orange oil) (from peppermint) OH Selinene Vitamin A (from celery oil) tail tail Squalene (from shark liver oil) Isopentenyl pyrophosphate Isoprenoid compounds are synthesized from acetate!! Early steps are analogous to fatty acid biosynthesis except no ACP O O O + SCoA -O SCoA Acetyl Malonyl coenzyme A coenzyme A O O + CO2 SCoA + CoASH Acetoacetyl coenzyme A O O O + SCoA SCoA Acetoacetyl Acetyl coenzyme A coenzyme A OH O SCoA OH + CoASH O 3-Hydroxy-3-methylglutaryl