11 Mar 13038 HIAP Policy Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

World Bank Document
Document of The World Bank FOR OFFICIAL USE ONLY Public Disclosure Authorized Report No: 3 8 147 - LK PROJECT APPRAISAL DOCUMENT ON A Public Disclosure Authorized PROPOSED CREDIT IN THE AMOUNT OF SDR 21.7 MILLION (US$32 MILLION EQUIVALENT) TO THE DEMOCRATIC SOCIALIST REPUBLIC OF SRI LANKA FOR A PUTTALAM HOUSING PROJECT Public Disclosure Authorized JANUARY 24,2007 Sustainable Development South Asia Region Public Disclosure Authorized This document has a restricted distribution and may be used by recipients only in the performance of their official duties. Its contents may not otherwise be disclosed without World Bank authorization. CURRENCY EQUIVALENTS (Exchange Rate Effective December 13,2006) Currency Unit = Sri Lankan Rupee 108 Rupees (Rs.) = US$1 US$1.50609 = SDR 1 FISCAL YEAR January 1 - December 31 ABBREVIATIONS AND ACRONYMS ADB Asian Development Bank LTF Land Task Force AG Auditor General LTTE Liberation Tigers ofTamil Eelam CAS Country Assistance Strategy NCB National Competitive Bidding CEB Ceylon Electricity Board NGO Non Governmental Organization CFAA Country Financial Accountability Assessment NEIAP North East Irrigated Agriculture Project CQS Selection Cased on Consultants Qualifications NEHRP North East Housing Reconstruction Program CSIA Continuous Social Impact Assessment NPA National Procurement Agency CSP Camp Social Profile NPV Not Present Value CWSSP Community Water Supply and Sanitation NWPEA North Western Provincial Environmental Act Project DMC District Monitoring Committees NWPRD NorthWest Provincial Roads Department -

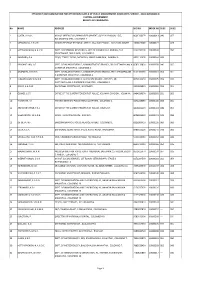
Index No Marks Sex Med Name 2200015 041 F 2200023 040 F 2200031 047 F 2200040 049 M 2200058 046 F 2200066 028 M 2200074 042 F 22
INDEX NO MARKS SEX MED NAME ADDRESS POSTAL ADDRESS 2200015 041 F SIN WASANTHI, M.K. DIVISIONAL SECRETARIAT, THIHAGODA. 2200023 040 F SIN KUMUDINI, E.V.S. DIVISIONAL SECRETARIAT, THIHAGODA. 2200031 047 F SIN WICKRAMASINGHE, W.M.K.P. DIVISIONAL SECRETARY OFFICE, UKUWELA. 2200040 049 M SIN BANDULA, B.G. DIVISIONAL SECRETARIAT, UKUWELA. 2200058 046 F SIN SAMARATHUNGE, S.M.N.R.K. DIVISIONAL SECRETARIAT, UKUWELA. 2200066 028 M SIN ABULASIN, S. DIVISIONAL SECRETARIAT, UKUWELA. 2200074 042 F SIN RANASINGHE, M.G.C. DIVISIONAL SECRETARIAT, UKUWELA. 2200082 040 F SIN MALIMAGE, G.M.P.S. A.G.A. OFFICE, KOLONNAWA. 2200090 044 M SIN PREMALAL, A.A.D.K. DIVISIONAL SECRETARIAT, KOLONNAWA. 2200104 042 F SIN GURUGE, I. DIVISIONAL SECRETARIAT, KOLONNAWA. 2200112 037 F SIN VIOLET, V.D.R. DIVISIONAL SECRETARIAT, KOLONNAWA. 2200120 051 F SIN BANNEHEKA, B.M.W.K. DIVISIONAL SECRETARIAT, ANAMADUWA. 2200139 044 F SIN HERATH, I.M.N.S.K. DISTRICT SECRETARIAT, SAMURDHI OFFICE, KURUNEGALA. 2200147 053 M SIN WIJESOORIYA, K.D.G. DISTRICT SECRETARIAT, KURUNEGALA. 2200155 046 M SIN CHAMINDA, K.M.R. SAMURDHI MANAGER, DIVISIONAL SECRETARIAT, PASSARA. 2200163 055 F SIN HETTIGE, D.H.S.L. DIVISIONAL SECRETARIAT, PASSARA. 2200171 066 F SIN KARUNAWATHI, J.M. DIVISIONAL SECRETARIAT, PASSARA. 2200180 053 F SIN DUNUSINGHE, P.N. DIVISIONAL SECRETARIAT, PASBAGE KORALE, NAWALAPITIYA. 2200198 060 F SIN SAMUDDIKA, W.P.N. DIVISIONAL SECERATARIAT, PASBAGE KORALE, NAWALAPITIYA. 2200201 042 M SIN RANAWEERA, K.S. DIVISIONAL SECRETARIAT, PASBAGE KORALE, NAWALAPITIYA. 2200228 041 F SIN INDRASEELI, K.M.N. DIVISIONAL SECRETARIAT, IMBULPE. 2200236 045 F SIN UDAGALADENIYA, S.M.I. -

Divisional Secretariats Contact Details
Divisional Secretariats Contact Details District Divisional Secretariat Divisional Secretary Assistant Divisional Secretary Life Location Telephone Mobile Code Name E-mail Address Telephone Fax Name Telephone Mobile Number Name Number 5-2 Ampara Ampara Addalaichenai [email protected] Addalaichenai 0672277336 0672279213 J Liyakath Ali 0672055336 0778512717 0672277452 Mr.MAC.Ahamed Naseel 0779805066 Ampara Ampara [email protected] Divisional Secretariat, Dammarathana Road,Indrasarapura,Ampara 0632223435 0632223004 Mr.H.S.N. De Z.Siriwardana 0632223495 0718010121 063-2222351 Vacant Vacant Ampara Sammanthurai [email protected] Sammanthurai 0672260236 0672261124 Mr. S.L.M. Hanifa 0672260236 0716829843 0672260293 Mr.MM.Aseek 0777123453 Ampara Kalmunai (South) [email protected] Divisional Secretariat, Kalmunai 0672229236 0672229380 Mr.M.M.Nazeer 0672229236 0772710361 0672224430 Vacant - Ampara Padiyathalawa [email protected] Divisional Secretariat Padiyathalawa 0632246035 0632246190 R.M.N.Wijayathunga 0632246045 0718480734 0632050856 W.Wimansa Senewirathna 0712508960 Ampara Sainthamarathu [email protected] Main Street Sainthamaruthu 0672221890 0672221890 Mr. I.M.Rikas 0752800852 0672056490 I.M Rikas 0777994493 Ampara Dehiattakandiya [email protected] Divisional Secretariat, Dehiattakandiya. 027-2250167 027-2250197 Mr.R.M.N.C.Hemakumara 027-2250177 0701287125 027-2250081 Mr.S.Partheepan 0714314324 Ampara Navithanvelly [email protected] Divisional secretariat, Navithanveli, Amparai 0672224580 0672223256 MR S.RANGANATHAN 0672223256 0776701027 0672056885 MR N.NAVANEETHARAJAH 0777065410 0718430744/0 Ampara Akkaraipattu [email protected] Main Street, Divisional Secretariat- Akkaraipattu 067 22 77 380 067 22 800 41 M.S.Mohmaed Razzan 067 2277236 765527050 - Mrs. A.K. Roshin Thaj 774659595 Ampara Ninthavur Nintavur Main Street, Nintavur 0672250036 0672250036 Mr. T.M.M. -

Performance Report 2013
Performance Report 2013 (A brief Performance Report of the key section and Provincial officers belongs to the Department Of Archaeology) Planning & Monitoring Section (Planning Division) Department of Archaeology Colombo - 07 Performance Report (2013) - 200 Content Page No. Department of Archaeology (Vision, Mision, Objectives) 201 - 204 Exploration and Documentation section 205 - 210 Excavation Section 211 - 214 Museum Service section 215 - 219 Architectural Conservation Section 220 - 224 Chemical Conservation section 225 - 234 Epigraphy and Numismatic Section 235 - 237 Maintenance section 238 - 244 Promotional section 245 – 249 Accounts section 250 - 251 Administration section 252 - 254 Planning & Monitoring Section 255 - 259 Legal section 260 - 287 Performance Report (2013) - 201 Archeological Department 1. Vision The Vision of the Department of Archaeology is to promote the proper management of Sri Lanka's archaeological heritage. 2. Mission The mission of the Department of Archaeology is function as Sri Lanka's apex institution and chief regulatory body for the management of it's archaeological heritage. 3. Objectives In order to fulfil its mission, the objectives of the Archeological Department are: 1. Development of Resources 1. Human 2. Institutional 3. Protection of the total archaeological heritage of Sri Lanka. 4. Inventorisation of the total Documenting archeological heritage' 1. Archeological places and monuments 2. Movable artifacts 3. Promoting public awareness on archeological heritages' 4. Conservation and maintenance of archeological sites monuments and movable artifacts 5. Researches\ Divisions dedicated for fulfilling aims of Department Academic Section Non academic Section 1. Exploration and Documentation section 2. Accounts section 3. Excavation Section 4. Administration section 5. Museum Service section 6. Planning & Monitoring Section 7. -
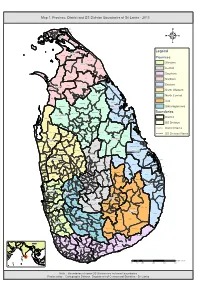
Map 1: Province, District and DS Division Boundaries of Sri Lanka - 2013
Map 1: Province, District and DS Division Boundaries of Sri Lanka - 2013 Vadam aradchi North (P oint Pedro) Valikam am North (Tellipallai) Valikam am S outh- West ( Sandilipay ) Vadam aradchi South-W es t (K araveddy) Valikam am W est (Chankanai) Karainagar Valikam am E ast (K opay) Valikam am S outh ( Uduv il) Jaffna Is land North (K ayts ) Thenm aradchi (Chavak achcheri) Jaffna Nallur Is land S outh (V elanai) Vadam aradchi Eas t Pachc hilaipalli 4 Delft Kandavalai Legend Kilinochchi Poonakary Karac hchi Provinces Puthukk udiyiruppu Mullaitivu Western Thunuk kai Maritim epattu Oddus uddan Central Mannar Town Southern Manthai W es t Manthai E ast Vav uniy a Nor th Welioya Northern Padavi Sr i P ura Madhu Eastern Mannar Vavuniya Padaviya Nanattan Vav uniy a Kuchc haveli North Western Vav uniy a S outh Gom ar ank adawala Kebithigollewa North Central Mus ali Vengalacheddik ulam Uva Morawewa Medawachc hiya Tr inc omalee Town and Gr av ets Mahawilachc hiy a Trincomalee Hor owpothana Sabaragamuwa Tham balagam uwa Ram bewa Kahatagas digiliya Kinniya Muttur Nuwar agam Palatha Central Boundaries Anuradhapura Mihinthale Kanthale Vanathawilluwa Noc hchiyagama District Nuwar agam Palatha E ast Seruv ila Verugal (E achc hilam pattu) Galenbindunuwewa Nac hchaduwa DS Division Thirappane Thalawa Medirigiriya Rajanganay a Colombo Tham buttegam a District Name Karuwalagas wewa Gir ibawa Hingurakgoda Ipalogam a Palugas wewa Kolonnawa Lank apura DS Division Name Welikanda Koralai P attu North (V aharai) Puttalam Galnewa Nawagattegam a Galgam uwa Kekirawa -

5000-Schools-Funded-By-The-Ministry
5000 Schools developed as Child Frendly Schools by funding Rs 500,000.00 by Economic Development Ministry to develop infastructure Province District Name of School Address Education Zone Education Division 1 Western Colombo SRI SANGAMITTA P.V. 62,ANANDA RAJAKARUNA MW.,COL-09 Colombo Borella 2 Western Colombo SUJATHA B.V. KIRIMANDALA MW.,COL-05 Colombo Colombo - South 3 Western Colombo LUMBINI P.V. HAVELOCK TOWN,COL-05. Colombo Colombo - South 4 Western Colombo ST.CLARE'S B.M.V. 1SR CHAPEL LANE,COL-06. Colombo Colombo - South 5 Western Colombo THANNINAYAGAM T.V. LESLEY RANAGALA MW.,COL-08 Colombo Borella 6 Western Colombo SIR BARON JAYATHILAKA V. MALIGAWATTA,COL-10. Colombo Colombo - Central 7 Western Colombo MIHINDU MAWATHA SINHALA V. MIHINDU MAWATHA,COLOMBO 12. Colombo Colombo - Central 8 Western Colombo ROMAN CATHOLIC V. KOTIKAWATTA, MULLERIYAWA NEW TOWN. Sri Jaya' pura Kolonnawa 9 Western Colombo MEETHOTAMULLA SRI RAHULA V. MEETHOTAMULLA, KOLONNAWA. Sri Jaya' pura Kolonnawa 10 Western Colombo KOTUWILA GAMINI V. KOTUWILA, WELLAMPITIYA. Sri Jaya' pura Kolonnawa 11 Western Colombo WERAGODA K.V. KOLONNAWA, WELLAMPITIYA. Sri Jaya' pura Kolonnawa 12 Western Colombo GOTHATUWA M.V. GOTHATUWA, ANGODA. Sri Jaya' pura Kolonnawa 13 Western Colombo VIDYAWARDENA V. WELLAMPITIYA, KOLONNAWA. Sri Jaya' pura Kolonnawa 14 Western Colombo SUGATHADHARMADHARA V. EGODAUYANA, MORATUWA Piliyandala Moratuwa 15 Western Colombo KATUKURUNDA ST MARY'S V. KATUKURUNDA, MORATUWA Piliyandala Moratuwa 16 Western Colombo SRI SADDARMODAYA V. KORALAWELLA MORATUWA Piliyandala Moratuwa 17 Western Colombo SRI NAGASENA V. KORAWELLA, MORATUWA Piliyandala Moratuwa 18 Western Colombo PITIPANA K.V. PITIPANA NORTH, HOMAGAMA. Homagama Homagama 19 Western Colombo DOLAHENA K.V. -

Alawwa Pradeshiya Sabha ------Kurunegala District ------1
Alawwa Pradeshiya Sabha -------------------------------- Kurunegala District ------------------------- 1. Financial Statements ---------------------------- 1.1 Presentation of Financial Statements ------------------------------------------------ Financial Statements for the year under review had been submitted to Audit on 23 March 2016 while Financial Statements relating to the preceding year had been submitted on 30 March 2015. The Auditor General’s Report relating to the year under review was sent to the Secretary of the Sabha on 14 July 2016. 1.2 Qualified Opinion -------------------------- In my opinion, except for the effect of the matters described in paragraph 1.3 of this report, financial statements give a true and fair view of the financial position of the AlawwaPradeshiyaSabha as at 31 December 2015 and its financial performance for the year then ended in accordance with Generally Accepted Accounting Principles. 1.3 Comments on Financial Statements ---------------------------------------------- 1.3.1 Accounting Deficiencies ------------------------------ Value of Trailer bearing No. 46-0524 had not been assessed and accounted. 1.3.2 Non-reconciled Control Accounts -------------------------------------------- Non-reconciliations in a sum of Rs.4,329,523 were observed between the balances relevant to 07 items of accounts existed at the end of the year under review and the balances existed in the subsidiary registers relevant to those. 1.3.3 Lack of Evidence for Audit ------------------------------------ Title deeds had not been obtained for14 blocks of lands valued at Rs.361,400 according to the Register of Fixed Assets. 1.3.4 Non-compliance with Laws, Rules, Regulations etc.. ------------------------------------------------------------------- Following instances of non-compliance with Laws, Rules, and Regulations etc are observed. Reference to Laws, Rules, Non-compliance Regulations etc. (a.) Pradeshiya Sabha Act No. -

Performance Report and Accounts of the District Secretariat
Content No. Chapter Page Number 1 Introduction 1 1.1 Message from the District Secretary/Government Agent 1 1.2 Vision 2 1.3 Mission 2 1.4 Objectives of the District Secretariat 2 1.5 Activities of the District Secretariat 2 1.6 Quality Policy of the District Secretariat 2 1.7 Divisions of the District Secretariat 3 1.8 Information of the District 4 1.9 Divisional Secretariats 4 1.10 District Plan 5 1.11 Organization Chart 6 2 Services provided by the Divisions of the District Secretariat 7 2.1 Administrative Division 7 2.2 District Planning Division 7 2.3 Explosives Division 8 2.4 Media Division 9 2.5 District Divineguma Division 9 2.6 Social Security Division 12 2.7 Measurment & Standard Division 12 2.8 Statistical Division 13 2.9 National Manure Secretariat 15 2.10 Non Government Organization Division 15 2.11 Cultural Division 15 2.12 Buddhist Affairs Division 16 2.13 Social Services Division 18 2.14 Disaster Management Co-ordinating Division 18 2.15 Ceylon Industrial Development Board 18 2.16 Motor Traffic Division 19 2.17 Disaster Relief Division 19 2.18 Internal Audit Division 20 2.19 Engineering Division 21 2.20 Job service centre 25 2.21 Agriculture Division 25 2.22 District Land Use Division 27 2.23 Child Protection Division 27 2.24 Womens‟ Development Division 28 2.25 Land Division 28 2.26 Early Childhood Development Division 29 2.27 Child Rights Division 30 2.28 Investigation Division 30 2.29 Councelling Division 30 2.30 Sports Division 31 2.31 Consumer Affairs Division 31 2.32 Productivity Division 32 2.33 Accounts Division 32 Provision of Annual Estimates 32 Expenditure against Provision 32 General Deposit Account 33 Revenue Account 34 Treasury Imprest Account 34 Provision of Line Ministries and Departments 34 Schedule 02 35 Schedule 03 37 Annual Appropriation Accounts 39 A.C.A - 2 39 A.C.A. -
Gender and Labour Migration A
While IOM endeavours to ensure the accuracy and completeness of the content of this paper, the views, findings, interpretations and conclusions expressed herein are those of the authors and field researchers and do not necessarily reflect the official position of the IOM and their Member States. IOM does not accept any liability for any loss which may arise from the reliance on information contained in this paper. IOM is committed to the principle that humane and orderly migration benefits migrants and society. As an intergovernmental organization, IOM acts with its partners in the international community to: assist in meeting the operational challenges of migration; advance understanding of migration issues; encourage social and economic development through migration; and uphold the human dignity and well-being of migrants. International Organization for Migration 17 route des Morillons 1211 Geneva 19 Switzerland Tel: +41.22.717 91 11 Fax: +41.22.798 61 50 E-mail: [email protected] Internet: http://www.iom.int ISBN 978-92-9068-453-4 © 2009 International Organization for Migration (IOM) All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise without the prior written permission of the publisher. 21_09 Gender Labour Migration in Asia Gender and Labour Migration in Asia Contents Foreword .................................................................................................. 7 Introduction -

An Application to the Travelling Salesman Problem
Operations Research and Applications: An International Journal (ORAJ), Vol.4, No.3/4, November 2017 AN APPLICATION TO THE TRAVELLING SALESMAN PROBLEM Damitha Bandara Management Department, Albany State University, Albany, GA, USA ABSTRACT ABC Appliances (Pvt) Ltd.,one of the leading companies in Sri Lanka has supplied and installed a very large number of air condition units all over the country. The company is currently provides a comprehensive after sales service for its customers. At present the service department is interesting in reducing the cost involving in regular after sale servicers. In this research we proposed a Travelling Salesman Problem (TSP) approach tominimize the cost involving in service tours. We used nearest neighbourhood search algorithm to obtain the solutions to the TSP. Computational examples show that the new service routes obtained using this algorithm will reduce the travelling cost significantly in comparison to existing routs. KEYWORDS Travelling Salesman Problem, Greedy Algorithm, NP Hard, Heuristic, Meta Heuristic, Nearest Neighbour 1. INTRODUCTION ABC Appliances Company (pvt) Ltd., one of the leading companies in Sri Lanka, was established in November 1991 for the purpose of marketing a range of brand products; air conditioners, water pumps, ceiling fans, table and pedestal fans, four-wheel tractors and generators. The company is currently distributing these products island wide through a strong dealer network. The ABC Appliances Company, not only distributing air conditioners and accessories but also provides a comprehensive after sales service for its customers. The company maintains a service department consists of a service manager, three engineers, thirty technicians, five motor vehicles and three motor bicycles to provide after sales for the customers. -
EB PMAS Class 2 2011 2.Pdf
EFFICIENCY BAR EXAMINATION FOR OFFICERS IN CLASS II OF PUBLIC MANAGEMENT ASSISTANT'S SERVICE - 2011(II)2013(2014) CENTRAL GOVERNMENT RESULTS OF CANDIDATES No NAME ADDRESS NIC NO INDEX NO SUB1 SUB2 1 COSTA, K.A.G.C. M/Y OF DEFENCE & URBAN DEVELOPMENT, SUPPLY DIVISION, 15/5, 860170337V 10000013 040 057 BALADAKSHA MW, COLOMBO 3. 2 MEDAGODA, G.R.U.K. INLAND REVENUE REGIONAL OFFICE, 334, GALLE ROAD, KALUTARA SOUTH. 745802338V 10000027 --- 024 3 HETTIARACHCHI, H.A.S.W. DEPT. OF EXTERNAL RESOURCES, M/Y OF FINANCE & PLANNING, THE 823273010V 10000030 --- 050 SECRETARIAT, 3RD FLOOR, COLOMBO 1. 4 BANDARA, P.A. 230/4, TEMPLE ROAD, BATAPOLA, MADELGAMUWA, GAMPAHA. 682113260V 10000044 ABS --- 5 PRASANTHIKA, L.G. DEPT. OF INLAND REVENUE, ADMINISTRATIVE BRANCH, SRI CHITTAMPALAM A 858513383V 10000058 040 055 GARDINER MAWATHA, COLOMBO 2. 6 ATAPATTU, D.M.D.S. DEPT. OF INLAND REVENUE, ADMINISTRATION BRANCH, SRI CHITTAMPALAM 816130069V 10000061 054 051 A GARDINER MAWATHA, COLOMBO 2. 7 KUMARIHAMI, W.M.S.N. DEPT. OF INLAND REVENUE, ACCOUNTS BRANCH, POB 515, SRI 867010025V 10000075 059 070 CHITTAMPALAM A GARDINER MAWATHA, COLOMBO 2. 8 JENAT, A.A.D.M. DIVISIONAL SECRETARIAT, NEGOMBO. 685060892V 10000089 034 051 9 GOMES, J.S.T. OFFICE OF THE SUPERINTENDENT OF POLICE, KELANIYA DIVISION, KELANIYA. 846453857V 10000092 031 052 10 HARSHANI, A.I. FINANCE BRANCH, POLICE HEAD QUARTERS, COLOMBO 1. 827122858V 10000104 064 061 11 ABHAYARATHNE, Y.P.J. OFFICE OF THE SUPERINTENDENT OF POLICE, KELANIYA. 841800117V 10000118 049 057 12 WEERAKOON, W.A.D.B. 140/B, THANAYAM PLACE, INGIRIYA. 802893329V 10000121 049 068 13 DE SILVA, W.I. -

North Western Province Rural Roads – Project 5
Involuntary Resettlement Due Diligence Report August 2014 SRI: Integrated Road Investment Program North Western Province Rural Roads – Project 5 Prepared by Road Development Authority, Ministry of Highways, Ports and Shipping for the Asian Development Bank CURRENCY EQUIVALENTS (as of 14 May 2014) Currency unit – Sri Lanka rupee (SLRe/SLRs) SLRe 1.00 = $ 0.007669 $1.00 = SLR 130.400 ABBREVIATIONS ADB - Asian Development Bank AP - Affected Person API - Affected Property Inventory CBO - Community Based Organization CPs - Community Participants CV - Chief Valuer DRR - Due Diligence Report DS - Divisional Secretariat ESDD - Environmental and Social Development Division FGD - Focus Group Discussion GoSL - Government of Sri Lanka GN - Grama Niladari GND - Grama Niladari Division GPS - Global Positioning System GRC - Grievance Redress Committee GRM - Grievance Redress Mechanism INGO - International Non-Government Organizations iROAD - Integrated Road Investment Program IR - Involuntary Resettlement LAA - Land Acquisition Act MOHPS - Ministry of Highways, Ports and Shipping MOU - Memorandum of Understanding MFF - Multi-tranche Financing Facility NGO - Non-Government Organizations NIRP - National Involuntary Resettlement Policy NWP - North Western Province PCC - Project Coordinating Committee PIU - Project Implementing Unit PRA - Participatory Rural Appraisal PS - Pradeshiya Sabha RDA - Road Development Authority SPS - Safeguards Policy Statement This involuntary resettlement due diligence is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area.