Bioethics in Nigeria: Knowledge and Perception During a Capacity-Building Workshop for Biomedical Researchers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Curriculum Vitae
CURRICULUM VITAE A. PERSONAL DATA 1. 1. Name:(Underline Surname) Adetutu Deborah Aina-Pelemo 2. 2. Marital Status Married 3. Postal/Contact Address No. 21a Avenue, Citec Mborah Estate, Jabi District, Abuja-FCT; 4. E-mail address [email protected] Or aina- [email protected]) Skype Name: adetutuaina 5. Mobile Phone No.: +2348038397372; 6. Number and Ages of Children One- (1 year) 7. Name and Address of Spouse Mr. Victor B. Pelemo; 77, Sokoto Road, GLO Office, Gusau, Zamfara, Nigeria 8. Name and Address of Next of Kin Mr. Victor B. Pelemo; 77, Sokoto Road, GLO Office, Gusau, Zamfara, Nigeria 9. Nationality Nigerian 10. State of Origin Osun State B. EDUCATIONAL BACKGROUND 11 Academic Institutions Attended with Dates i) Sharda University 2015 – 2019 ii) University of Ilorin 2012 – 2014 iii) Nigerian Law School 2009 – 2010 iv) Olabisi Onabanjo University 2004 – 2009 v) Federal Government College, Ibillo, 1996 - June 2001 vi) Ola - Oluwa Nur./Pry School, Iju-Itaogboolu, 1989 – 1995 12 Academic and Professional Qualifications i) Doctor of Philosophy, (Ph.D. in Labour Relations & 2019 Industrial Law) ii) Master of Laws (Common Law) 2014 iii) Barrister at Laws (B.L) 2010 iv) Bachelor of Laws (LL.B) Second Class Honours 2009 13 Distinctions, Fellowships and Awards with Dates i) Resource Person: Selection of the best Researched Paper at the 3rd National Conference on Human Rights and Gender Justice. Knowledge Steez, at Indian Law Institute, New Delhi. June 2018 ii) Moot Judge: Preliminary Round on the occasion of 5th National Moot Court Competition of School of Law, IMS Unison University, Dehradum -- India. -

African Journal of Political Science and International Relations Volume 8 Number Number 2 6January, September 2014 2014 ISSN 19961993-08328233
African Journal of Political Science and International Relations Volume 8 Number Number 2 6January, September 2014 2014 ISSN 19961993-08328233 ABOUT AJPSIR The African Journal of Political Science and International Relations (AJPSIR) is published monthly (one volume per year) by Academic Journals. African Journal of Political Science and International Relations (AJPSIR) is an open access journal that publishes rigorous theoretical reasoning and advanced empirical research in all areas of the subjects. We welcome articles or proposals from all perspectives and on all subjects pertaining to Africa, Africa's relationship to the world, public policy, international relations, comparative politics, political methodology, political theory, political history and culture, global political economy, strategy and environment. The journal will also address developments within the discipline. Each issue will normally contain a mixture of peer-reviewed research articles, reviews or essays using a variety of methodologies and approaches. Contact Us Editorial Office: [email protected] Help Desk: [email protected] Website: http://www.academicjournals.org/journal/AJPSIR Submit manuscript online http://ms.academicjournals.me/ Editors Dr. Thomas Kwasi Tieku Dr. Aina, Ayandiji Daniel Faculty of Management and Social Sciences New College, University of Toronto Babcock University, Ilishan – Remo, Ogun State, 45 Willcocks Street, Rm 131, Nigeria. Toronto, Ontario, Canada. Prof. F. J. Kolapo Dr. Mark Davidheiser History Department University of Guelph Nova Southeastern University 3301 College Avenue; SHSS/Maltz Building N1G 2W1Guelph, On Canada Fort Lauderdale, FL 33314 USA. Dr. Nonso Okafo Graduate Program in Criminal Justice Dr. Enayatollah Yazdani Department of Political Science Department of Sociology Norfolk State University Faculty of Administrative Sciences and Economics University of Isfahan Norfolk, Virginia 23504 Isfahan Iran. -
A Report on the Mapping Study of Peace & Security Engagement In
A Report on the Mapping Study of Peace & Security Engagement in African Tertiary Institutions Written by Funmi E. Vogt This project was funded through the support of the Carnegie Corporation About the African Leadership Centre In July 2008, King’s College London through the Conflict, Security and Development group (CSDG), established the African Leadership Centre (ALC). In June 2010, the ALC was officially launched in Nairobi, Kenya, as a joint initiative of King’s College London and the University of Nairobi. The ALC aims to build the next generation of scholars and analysts on peace, security and development. The idea of an African Leadership Centre was conceived to generate innovative ways to address some of the challenges faced on the African continent, by a new generation of “home‐grown” talent. The ALC provides mentoring to the next generation of African leaders and facilitates their participation in national, regional and international efforts to achieve transformative change in Africa, and is guided by the following principles: a) To foster African‐led ideas and processes of change b) To encourage diversity in terms of gender, region, class and beliefs c) To provide the right environment for independent thinking d) Recognition of youth agency e) Pursuit of excellence f) Integrity The African Leadership Centre mentors young Africans with the potential to lead innovative change in their communities, countries and across the continent. The Centre links academia and the real world of policy and practice, and aims to build a network of people who are committed to the issue of Peace and Security on the continent of Africa. -

Peer Reviewed Abstract Submitted to the College of Health Sciences, Osun State University Annual Scientific Conference, June 15-19, 2020
PEER REVIEWED ABSTRACT SUBMITTED TO THE COLLEGE OF HEALTH SCIENCES, OSUN STATE UNIVERSITY ANNUAL SCIENTIFIC CONFERENCE, JUNE 15-19, 2020. ABSTRACT - CHS/2020/01 Assessment of risk factors associated with drug resistant-tuberculosis among patients on dots treatment for tuberculosis in Ibadan, Oyo State *Akinleye, C.A.1, Onabule, A.2, Oyekale, A.O.3, Akindele, M.O.2, Babalola, O.J.4, Olarewaju, S.O.1 1Department of Community Medicine, Osun State University, Osogbo, Nigeria 2Department of Clinical Nursing University College Hospital, Ibadan, Nigeria 3Department of Chemical Pathology Ladoke Akintola University of Technology, Osogbo, Nigeria. 4Oyo state Tuberculosis and leprosy control unit. Ministry of Health. Secretariat, Ibadan, Nigeria *Corresponding author: Dr Callistus Akinleye (E-mail: [email protected]) Introduction: MDR-TB poses a significant challenge to global management of TB. Laboratories in many countries among which include Nigeria are unable to evaluate drug resistance, and clinical predictors of MDR-TB might help target suspected patients. Method: The study was a cross sectional study design. Multistage sampling technique was employed in the selection of 403 tuberculosis patients. Data were analyzed using SPSS version 25. Level of significance was set at P<0.05. Results: Fifty three 53 (13.2%) of the total respondent had MDR-TB compare to national prevalence of 8% which is steeper among males 36(67.9%) (p>0.05). Education and Occupation shows a significant association with MDR-TB, (÷2=24.640, p = 0.007) and (÷2=14.416, p=0.006) respectively, smoking (r=0.074, p<0.05) and alcohol consumption (r=0.083, p>0.05) show no significant association with occurrence MDR-TB. -
Beyondrt Book02.Indb 1 05/12/2016 10:25 Knowing Each Other Project - 11 Jan 2017
RELIGION IN TRANSFORMING AFRICA Knowing Each Other Project - 11 Jan 2017 Beyond Religious Tolerance Beyond ‘an important contribution to the ethnography of religion, peaceful coexistence and communal politics … a very readable and enjoyable book.’ Wale Adebanwi, University of California-Davis ‘a timely and refreshing addition to the growing literature on religious collaboration and coexistence in otherwise religiously divided societies across the world.’ Ebenezer Obadare, University of Kansas Since the end of the Cold War, and especially since 9/11, religion has become an increasingly important factor of personal and group identification. Based on an African case study, this book calls for new ways of thinking about diversity that go ‘beyond religious tolerance’. Focusing on the predominantly Muslim Yoruba town of Ede, the authors challenge the assumption that religious difference automatically leads to conflict: in south-west Nigeria, Muslims, Christians and traditionalists have co-existed largely peacefully since the early twentieth century. In some contexts, Ede’s citizens emphasise the importance and significance of religious difference, and the need for tolerance. But elsewhere they refer to religious boundaries in passing, or even celebrate and transcend religious divisions. Drawing on detailed ethnographic and historical research, survey work, oral histories and poetry by UK- and Nigeria- based researchers, the book examines how Ede’s citizens experience religious difference in their everyday lives. It examines the town’s royal history and relationship with the deity Sàngó, its old Islamic compounds and its Christian institutions, as well as marriage and family life across religious boundaries, to illustrate the multiplicity of religious practices in the life of the town and its citizens and to suggest an alternative approach to religious difference. -
Unai Members List August 2021
UNAI MEMBER LIST Updated 27 August 2021 COUNTRY NAME OF SCHOOL REGION Afghanistan Kateb University Asia and the Pacific Afghanistan Spinghar University Asia and the Pacific Albania Academy of Arts Europe and CIS Albania Epoka University Europe and CIS Albania Polytechnic University of Tirana Europe and CIS Algeria Centre Universitaire d'El Tarf Arab States Algeria Université 8 Mai 1945 Guelma Arab States Algeria Université Ferhat Abbas Arab States Algeria University of Mohamed Boudiaf M’Sila Arab States Antigua and Barbuda American University of Antigua College of Medicine Americas Argentina Facultad de Ciencias Económicas de la Universidad de Buenos Aires Americas Argentina Facultad Regional Buenos Aires Americas Argentina Universidad Abierta Interamericana Americas Argentina Universidad Argentina de la Empresa Americas Argentina Universidad Católica de Salta Americas Argentina Universidad de Congreso Americas Argentina Universidad de La Punta Americas Argentina Universidad del CEMA Americas Argentina Universidad del Salvador Americas Argentina Universidad Nacional de Avellaneda Americas Argentina Universidad Nacional de Cordoba Americas Argentina Universidad Nacional de Cuyo Americas Argentina Universidad Nacional de Jujuy Americas Argentina Universidad Nacional de la Pampa Americas Argentina Universidad Nacional de Mar del Plata Americas Argentina Universidad Nacional de Quilmes Americas Argentina Universidad Nacional de Rosario Americas Argentina Universidad Nacional de Santiago del Estero Americas Argentina Universidad Nacional de -

Research4life Academic Institutions
Research4Life Academic Institutions Filter Summary Country City Institution Name Afghanistan Bamyan Bamyan University Charikar Parwan University Cheghcharan Ghor Institute of Higher Education Ferozkoh Ghor university Gardez Paktia University Ghazni Ghazni University HERAT HERAT UNIVERSITY Herat Institute of Health Sciences Ghalib University Jalalabad Nangarhar University Alfalah University Kabul Afghan Medical College Kabul 06-Mar-2018 3:52 PM Prepared by Payment, HINARI Page 1 of 174 Country City Institution Name Afghanistan Kabul JUNIPER MEDICAL AND DENTAL COLLEGE Government Medical College Kabul University. Faculty of Veterinary Science Aga Khan University Programs in Afghanistan (AKU-PA) Kabul Dental College, Kabul Kabul University. Central Library American University of Afghanistan Agricultural University of Afghanistan Kabul Polytechnic University Kabul Education University Kabul Medical University, Public Health Faculty Cheragh Medical Institute Kateb University Prof. Ghazanfar Institute of Health Sciences Khatam al Nabieen University Kabul Medical University Kandahar Kandahar University Malalay Institute of Higher Education Kapisa Alberoni University khost,city Shaikh Zayed University, Khost 06-Mar-2018 3:52 PM Prepared by Payment, HINARI Page 2 of 174 Country City Institution Name Afghanistan Lashkar Gah Helmand University Logar province Logar University Maidan Shar Community Midwifery School Makassar Hasanuddin University Mazar-e-Sharif Aria Institute of Higher Education, Faculty of Medicine Balkh Medical Faculty Pol-e-Khumri Baghlan University Samangan Samanagan University Sheberghan Jawzjan university Albania Elbasan University "Aleksander Xhuvani" (Elbasan), Faculty of Technical Medical Sciences Korca Fan S. Noli University, School of Nursing Tirana University of Tirana Agricultural University of Tirana 06-Mar-2018 3:52 PM Prepared by Payment, HINARI Page 3 of 174 Country City Institution Name Albania Tirana University of Tirana. -

Africa and the New World Order KISII UNIVERSITY 2014
KISII UNIVERSITY First Annual International Conference on: Africa and the New World Order Organized by Kisii University (KSU) Main Campus, KisiI, Kenya When: July 30th to august 2nd, 2014 DAY 1 DAY2 DAY 3 30THJULY-WEDNESDAY 31ST JULY-THURSDAY 1ST AUGUST-FRIDAY 2014 Message from Convenor of 1st International Annual Interdisciplinary Conference Prof. Maurice Nyamanga Amutabi, PhD Welcome to the KISII UNIVERSITY (KSU) Ladies and gentlemen, I would like to take this opportunity to invite you to the First Annual International Interdisciplinary Conference, taking place at the Kisii University (KSU) from July 30 to August 2, 2014, Kisii, Kenya on behalf of the management of this university, led by our Vice Chancellor John S. Akama. It is a great honour to welcome over 500 of you, to this important conference. This is a major milestone to our University because this is the highest number that Kisii University will be hosting for the first time. We need to applaud the University for this great achievement in th history of this young institution In Things Fall Apart, Chinua Achebe talks about the lizard that jumped from the high iroko tree and said he would praise himself if no one else did. I am excited that many of you have decided to attend this highly acclaimed 1st Annual International Interdisciplinary Conference despite the terror threat in the country. It gives me great pleasure and honour to welcome you all. We have put all necessary plans in place to avert any security threat. We know this year’s conference, like Juan Antonio Samarach often said of the Olympics, “will be the greatest ever!” The Annual Conference We intend to make this conference to be an annual event . -

Internet Addiction, Problematic Smartphone Use and Psychological Health of Nigerian University Undergraduates
International Neuropsychiatric Disease Journal 12(3): 1-13, 2018; Article no.INDJ.46846 ISSN: 2321-7235, NLM ID: 101632319 Internet Addiction, Problematic Smartphone Use and Psychological Health of Nigerian University Undergraduates Bede C. Akpunne1* and Olutope E. Akinnawo1 1Department of Behavioural Studies, College of Management and Social Sciences, Redeemer’s University, Osun State, Nigeria. Authors’ contributions This work was carried out in collaboration between both authors. Both authors read and approved the final manuscript. Article Information DOI: 10.9734/INDJ/2018/v12i330093 Editor(s): (1) Dr. Zhefeng Guo, Department of Neurology, University of California, Los Angeles, USA. Reviewers: (1) K. Ramesh Kumar, K.L.N.University of Health Sciences, India. (2) Victor Moses, Ahmadu Bello University, Nigeria. (3) Noorain Alam, Post Graduate Institute of Medical Education & Research, Chandigarh, India. Complete Peer review History: http://www.sdiarticle3.com/review-history/46846 Received 10 November 2018 Accepted 28 January 2019 Original Research Article Published 26 February 2019 ABSTRACT Aim: This study examined Internet Addiction (IA) and Problematic Smartphone Use (PSU) as predictors of severities of anxiety, depression and psychological distress among university undergraduates in Nigeria. Study Design: Exploratory /Descriptive survey design. Place and Duration of Study: Redeemer’s University Nigeria, between April and August 2018. Methodology: A total of 854 university undergraduates made up of 342 males and 512 females, mean age 20.5 years, were purposively selected from four universities in Osun state, southwestern Nigeria. Internet Addiction Test (IAT), Smartphone Addiction Scale – Short Version (SAS-SV), Beck Anxiety Inventory (BAI), Centre for Epidemiological Studies Depression Scale (CES-D) and General Health Questionnaire (GHQ-12) were used for data collection. -

STRENGTHENING UNIVERSITY-INDUSTRY LINKAGES in AFRICA a Study on Institutional Capacities and Gaps
STRENGTHENING UNIVERSITY-INDUSTRY LINKAGES IN AFRICA A Study on Institutional Capacities and Gaps JOHN SSEBUWUFU, TERALYNN LUDWICK AND MARGAUX BÉLAND Funded by the Canadian Government through CIDA Canadian International Agence canadienne de Development Agency développement international STRENGTHENING UNIVERSITY-INDUSTRY LINKAGES IN AFRICA: A Study on Institutional Capacities and Gaps Prof. John Ssebuwufu Director, Research & Programmes Association of African Universities (AAU) Teralynn Ludwick Research Officer AAU Research and Programmes Department / AUCC Partnership Programmes Margaux Béland Director, Partnership Programmes Association of Universities and Colleges of Canada (AUCC) Currently on secondment to the Canadian Bureau for International Education (CBIE) Strengthening University-Industry Linkages in Africa: A Study of Institutional Capacities and Gaps @ 2012 Association of African Universities (AAU) All rights reserved Printed in Ghana Association of African Universities (AAU) 11 Aviation Road Extension P.O. Box 5744 Accra-North Ghana Tel: +233 (0) 302 774495/761588 Fax: +233 (0) 302 774821 Email: [email protected], [email protected] Web site: http://www.aau.org This study was undertaken by the Association of African Universities (AAU) and the Association of Universities and Colleges of Canada (AUCC) as part of the project, Strengthening Higher Education Stakeholder Relations in Africa (SHESRA). The project is generously funded by Government of Canada through the Canadian International Development Agency (CIDA). The views and opinions -

ADEBIMPE Wasiu Olalekan 2. Email Address
CURRICULUM VITAE A: PERSONAL DATA 1. Name: ADEBIMPE Wasiu Olalekan 2. Email Address : [email protected] 3. Nationality Nigerian 4. State of origin Oyo 5. Senatorial district Oyo West 6. Local Government Area Ido 7. Marital Status : Married 8. Date of assumption of duty 3rd July 2017 9. Rank/status on 1st appointment Reader 10. Present status Reader 11. Grade and Date of last promotion Associate Professor, 1st October 2016 12. Grade and place of last promotion Osun State University Osogbo 13. College/Faculty Health Sciences/ Clinical Sciences 14. Department / Unit Community Medicine/Epidemiology B. EDUCATIONAL BACKGROUND 1. HIGHER EDUCATIONAL INSTITUTIONS ATTENDED WITH DATES i. West African Postgraduate Medical College 2003-2008 ii. University of Benin, Nigeria 2003-2005 iii. University of Lagos, Nigeria 1991-1998 iv. University of Central Nicaragua 2012-2015 1 v. Kwara State University 2017 till date 2. ACADEMIC/PROFESSIONAL QUALIFICATIONS AND DISTINCTIONS OBTAINED WITH DATES i. Fellowship of the West African College of Physicians (FWACP) Community Health- April 2008. ii. Master’s Degree in Public Health (MPH) - University of Benin, February 2005 iii. Bachelor of Medicine, Bachelor of Surgery (MBBS)- University of Lagos, March 1998 iv. PhD in Public Health, University of Central Nicaragua 2015 v. PhD Epidemiology (in view) vi. Fellowship of the African Institute of Public Health 2017 3. OTHER DISTINCTIONS AND AWARDS WITH DATES (a) Scholarship i. Classic magazine scholarship 1995-1997 (b) Fellowship (c) Research grants i. Awarded three TETFund Research grants in 2014//2015/16: Lead/principal researcher in one of the grants ii. Awarded research grants from Center for Reproductive Health Innovation , University of Benin: as a co-investigator (d) National awards i. -

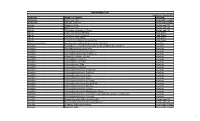
Percentage of Special Needs Students
Percentage of special needs students S/N University % with special needs 1. Abia State University, Uturu 4.00 2. Abubakar Tafawa Balewa University, Bauchi 0.00 3. Achievers University, Owo 0.00 4. Adamawa State University Mubi 0.50 5. Adekunle Ajasin University, Akungba 0.08 6. Adeleke University, Ede 0.03 7. Afe Babalola University, Ado-Ekiti - Ekiti State 8. African University of Science & Technology, Abuja 0.93 9. Ahmadu Bello University, Zaria 0.10 10. Ajayi Crowther University, Ibadan 11. Akwa Ibom State University, Ikot Akpaden 0.00 12. Alex Ekwueme Federal University, Ndufu Alike, Ikwo 0.01 13. Al-Hikmah University, Ilorin 0.00 14. Al-Qalam University, Katsina 0.05 15. Ambrose Alli University, Ekpoma 0.03 16. American University of Nigeria, Yola 0.00 17. Anchor University Ayobo Lagos State 0.44 18. Arthur Javis University Akpoyubo Cross River State 0.00 19. Augustine University 0.00 20. Babcock University, Ilishan-Remo 0.12 21. Bayero University, Kano 0.09 22. Baze University 0.48 23. Bells University of Technology, Ota 1.00 24. Benson Idahosa University, Benin City 0.00 25. Benue State University, Makurdi 0.12 26. Bingham University 0.00 27. Bowen University, Iwo 0.12 28. Caleb University, Lagos 0.15 29. Caritas University, Enugu 0.00 30. Chrisland University 0.00 31. Christopher University Mowe 0.00 32. Clifford University Owerrinta Abia State 0.00 33. Coal City University Enugu State 34. Covenant University Ota 0.00 35. Crawford University Igbesa 0.30 36. Crescent University 0.00 37. Cross River State University of Science &Technology, Calabar 0.00 38.