Evolving Pharmacovigilance Requirements with Novel Vaccines and Vaccine Components
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Hexavalent Dtap/IPV/Hib/Hepb Combination Vaccine: Information for Healthcare Practitioners About the Neonatal Selective
The hexavalent DTaP/IPV/Hib/HepB combination vaccine Information for healthcare practitioners about the neonatal selective immunisation programme for babies at risk of hepatitis B The Hexavalent DTaP/IPV/Hib/HepB combination vaccine: Information for Healthcare Practitioners (selective programme) About Public Health England Public Health England exists to protect and improve the nation’s health and wellbeing, and reduce health inequalities. We do this through world-leading science, research, knowledge and intelligence, advocacy, partnerships and the delivery of specialist public health services. We are an executive agency of the Department of Health and Social Care, and a distinct delivery organisation with operational autonomy. We provide government, local government, the NHS, Parliament, industry and the public with evidence-based professional, scientific and delivery expertise and support. Public Health England Wellington House 133-155 Waterloo Road London SE1 8UG Tel: 020 7654 8000 www.gov.uk/phe Twitter: @PHE_uk Facebook: www.facebook.com/PublicHealthEngland For queries relating to this document, please contact: [email protected] © Crown copyright 2020 You may re-use this information (excluding logos) free of charge in any format or medium, under the terms of the Open Government Licence v3.0. To view this licence, visit OGL. Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned. First published November 2017 This updated version published February -
Download File (Pdf)
2021 FORUM REPORT COVID-19 in Africa one year on: Impact and Prospects MO IBRAHIM FOUNDATION 2021 FORUM REPORT COVID-19 in Africa one year on: Impact and Prospects MO IBRAHIM FOUNDATION Foreword by Mo Ibrahim Notwithstanding these measures, on current projections Founder and Chair of the Mo Ibrahim Africa might not be adequately covered before 2023. Foundation (MIF) Vaccinating Africa is an urgent matter of global security and all the generous commitments made by Africa’s partners must now be delivered. Looking ahead - and inevitably there will be future pandemics - Africa needs to significantly enhance its Over a year ago, the emergence and the spread of COVID-19 homegrown vaccine manufacturing capacity. shook the world and changed life as we knew it. Planes were Africa’s progress towards its development agendas was off grounded, borders were closed, cities were shut down and course even before COVID-19 hit and recent events have people were told to stay at home. Other regions were hit created new setbacks for human development. With very earlier and harder, but Africa has not been spared from the limited access to remote learning, Africa’s youth missed out pandemic and its impact. on seven months of schooling. Women and girls especially The 2021 Ibrahim Forum Report provides a comprehensive are facing increased vulnerabilities, including rising gender- analysis of this impact from the perspectives of health, based violence. society, politics, and economics. Informed by the latest data, The strong economic and social impacts of the pandemic it sets out the challenges exposed by the pandemic and the are likely to create new triggers for instability and insecurity. -

UNICEF Pentavalent-Hexa 2021+ Pre-Tender Industry Consultation
UNICEF Pentavalent-Hexa 2021+ Pre-Tender Industry Consultation 19th SEPTEMBER 2019 1 Presentation Outline 1. Context ▪ Gavi Board decision ▪ Hexa strategic alignment ▪ Value Based Assessment 2. Demand scenarios and assumptions 3. Pentavalent Tender: ▪ Objectives ▪ Scope ▪ Duration ▪ Modality 4. Summary of feedback and response to questionnaire 5. Timelines 1. CONTEXT Gavi Board decision Hexa strategic alignment Value Based Assessment 3 Gavi Board November 2018 – Decisions IPV Post-2020 DTP booster VIS 2018 VIS 2018 + Hexavalent as immunisation option • Approved support for D, T & P vaccines (Td, DTwP, pentavalent) to be used as booster doses beginning in 2021 • Approved support for inactivated poliovirus vaccine (IPV), with country financing arrangements subject to alignment with the final parameter setting for Gavi 5.0 at the June 2019 Board meeting* • Approved in principle support of wP-Hexavalent vaccine, subject to a vaccine being licenced, recommended for use by WHO, WHO pre-qualified and that market attributes support the successful implementation of Hexavalent The development of capacity for standalone IPV remains the main priority for Gavi Alliance as part of the effort to eradicate polio All Gavi Board decisions are “subject to the availability of funding for the 2021-2025 period and alignment with the final parameter setting for Gavi 5.0 at the June 2019 Board meeting.” *Gavi's Board approved IPV co-financing arrangements post-2020 in its June 2019 session 4 Conditions to open a funding window for Hexavalent Condition 1: Hexavalent vaccines that are candidates for Gavi support should achieve IPV immunogenicity targets as per WHO’s SAGE recommendations. Condition 2: Hexavalent vaccines are priced in line with value-based principles. -

Case Studies Controversies in Vaccination
European Review, Vol. 21, No. S1, S56–S61 r 2013 Academia Europæa. The online version of this article is published within an Open Access environment subject to the conditions of the Creative Commons Attribution license ,http://creativecommons.org/licenses/by/3.0/.. doi:10.1017/S1062798713000227 Session 3 – Case Studies Controversies in Vaccination ROMAN PRYMULA University Hospital Hradec Kralove, Sokolska 581, 500 05 Hradec Kralove, Czech Republic. E-mail: [email protected] Infectious diseases still jeopardize human health and even lives. In spite of the variety of advanced treatment methods, prevention is considered to be the most effective way to fight infections, and vaccination, no doubt, is one of the most effective preventive measures in the history of mankind. The vaccine controversy is based on a dispute over morality, ethics, effectiveness, and/or safety. There is no 100% safe or effective vaccine; however, benefits clearly overweigh risks. Ironically, as the numbers of cases of vaccine- preventable infectious diseases are falling, the controversies relating to vaccine safety are growing. Vaccines are generally victims of their own success. Controversies can afflict the positive acceptance of immunization, decrease the coverage and uptake and finally threaten the health of children and adults. The advent of vaccination has proven to be one of the most effective preventive measures in the history of medicine. Vaccines play a significant role in the prevention of debili- tating and, in many cases, life-threatening infectious diseases. Vaccines also provide important benefits in terms of reducing or avoiding costs associated with illness, both direct and indirect. In spite of the absence of any kind of ideal global healthcare system and lack of resources, the World Health Organisation (WHO) and the United Nations Children’s Fund (UNICEF) were able, in 1974, to establish a major global project called the Expanded Programme on Immunization (EPI). -

Immunogenicity and Safety of a Fully Liquid Dtap-IPV-Hep B-PRP-T
ccines & a V f V a o c l c i a n n a Lanata et al., J Vaccines Vaccin 2012, 3:1 r t u i o o n J Journal of Vaccines & Vaccination DOI: 10.4172/2157-7560.1000128 ISSN: 2157-7560 Research Article Open Access Immunogenicity and Safety of a Fully Liquid DTaP-IPV-Hep B-PRP-T Vaccine at 2-4-6 Months of Age in Peru Claudio Lanata1, Betzana Zambrano2, Lucie Ecker1, Isabel Amemiya1, Ana Gil1 and Eduardo Santos Lima3* 1Instituto de Investigación Nutricional, Lima, Peru 2Sanofi Pasteur, Montevideo, Uruguay 3Clinical Development, Sanofi Pasteur, Lyon, France Abstract Objectives: To assess the immunogenicity and safety of a new candidate, fully liquid, hexavalent DTaP-IPV- Hep B-PRP-T vaccine (Hexaxim™, an AcXim family vaccine) compared to a licensed hexavalent DTaP-IPV-Hep B// PRP-T vaccine (Infanrix hexa®) in Peru. Methods: Infants born to HBsAg seronegative mothers and who had not received a hepatitis B vaccine prior to entry into the study were randomized to receive either Hexaxim™ (Group 1) or Infanrix hexa® (Group 2) at 2, 4, 6 months of age. Seroprotection (SP) rate for hepatitis B (anti-HBs antibody concentration ≥10 mIU/mL) was analysed for non-inferiority (Group 1 minus Group 2) 1 month post-primary series. Anti-diphtheria and anti-polyrosil ribitol phosphate (PRP) antibody responses were analysed descriptively. Safety was analysed from parental reports. Results: Seroprotection rate for anti-HBs antibody titers ≥10 mIU/mL was high in both groups (≥99.2%) and non-inferiority was demonstrated (lower bound of the 95% CI for the difference was -4.17, above the pre-defined delta [-10%]). -

Evidence Assessment STRATEGIC ADVISORY GROUP of EXPERTS (SAGE) on IMMUNIZATION Meeting 15 March 2021
Evidence Assessment STRATEGIC ADVISORY GROUP OF EXPERTS (SAGE) ON IMMUNIZATION Meeting 15 March 2021 FOR RECOMMENDATION BY SAGE Prepared by the SAGE Working Group on COVID-19 vaccines EVIDENCE ASSESSMENT: Ad26.COV2.S COVID-19 vaccine Key evidence to inform policy recommendations on the use of Ad26.COV2.S COVID-19 vaccine Evidence retrieval • Based on WHO and Cochrane living mapping and living systematic review of Covid-19 trials (www.covid-nma.com/vaccines) Retrieved evidence Majority of data considered for policy recommendations on Ad26.COV2.S Covid-19 vaccine are published in scientific peer reviewed journals: • Interim Results of a Phase 1–2a Trial of Ad26.COV2.S Covid-19 Vaccine. NEJM. February 2021. DOI: 10.1056/NEJMoa2034201. Jerald Sadoff, Mathieu Le Gars, Georgi Shukarev, et al. • FDA briefing document Janssen Ad26.COV2.S (COVID-19) Vaccine • Ad26 platform literature: Custers et al. Vaccines based on the Ad26 platform; Vaccine 2021 Quality assessment Type of bias Randomization Deviations from Missing outcome Measurement of Selection of the Overall risk of intervention data the outcome reported results bias Working Group Low Low Low Low Low LOW judgment 1 EVIDENCE ASSESSMENT The SAGE Working Group specifically considered the following issues: 1. Trial endpoints used in comparison with other vaccines Saad Omer 2. Evidence on vaccine efficacy in the total population and in different subgroups Cristiana Toscano 3. Evidence of vaccine efficacy against asymptomatic infections, reducing severity, hospitalisations, deaths, and efficacy against virus variants of concern Annelies Wilder-Smith 4. Vaccination after SARS-CoV2 infection. 5. Evidence on vaccine safety in the total population and in different subgroups Sonali Kochhar 6. -

(Nitags) and WHO Immunisation-Related Advisory Committees
Summary of recent issues considered by four national immunisation technical advisory groups (NITAGs) and WHO immunisation-related advisory committees Prepared by the National Centre for Immunisation Research & Surveillance (NCIRS) Period of review: 16/05/2019 to 13/09/2019 Contents 1 Advisory Committee on Immunization Practices (ACIP), USA .......................................................... 3 1.1 ACIP meeting: 26-27 June 2019 ....................................................................................................... 3 1.2 Newly published or updated recommendations ............................................................................... 20 1.2.1 Japanese Encephalitis Vaccine: Recommendations of the Advisory Committee on Immunisation Practices.......................................................................................................................... 20 1.2.2 Human Papillomavirus Vaccination for Adults: Updated Recommendations of the Advisory Committee on Immunization Practice ..................................................................................................... 20 1.2.3 Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2019–20 Influenza Season ............ 21 1.3 New or updated recommendations – not yet published ................................................................... 21 2 Immunisation Advisory Centre (IMAC), New Zealand .................................................................... -

Improving the Regulatory Response to Vaccine Development During a Public Health Emergency
Every Minute Matters: Improving the Regulatory Response to Vaccine Development During a Public Health Emergency RASHMI BORAH* ABSTRACT In recent months, our lives have been turned upside down by the novel coronavirus (COVID-19) emergency. With no cure or vaccine in sight, millions of people have contracted the virus, and the death toll has surpassed that of World War I in a fraction of the time. In fact, the past decade has been marked by a series of highly publicized public health emergencies, including the devastating Ebola and Zika virus global outbreaks. Some of this panic arose from a failure to manufacture and distribute vaccines in a timely fashion. This failure occurred despite having several viable vaccine candidates, adequate funding, and strong public support for the vaccines. This Article explains how these failures are the consequence of a complex network of existing regulatory pathways and insufficient incentives to produce affordable vaccinations during a public health emergency. Fortunately, there are several ways that both the U.S. Patent and Trademark Office and the U.S. Food and Drug Administration can improve and streamline the process of patenting, approving, manufacturing, and distributing a vaccination. The last decade has demonstrated that public health emergencies occur quickly, and affected communities cannot afford the delays and mishaps that characterized the vaccine response to COVID-19, Ebola, and Zika. This Article explores three ways to facilitate the development and distribution of vaccinations during a public health emergency. First, the U.S. Patent and Trademark Office can establish a dedicated public health emergency patent pathway for vaccine technology developed specifically in response to a public health emergency. -

Gavi's Role in Market Shaping and Procurement
CGD NOTE Jun 2019 Gavi’s Role in Market Shaping and Procurement: Progress, Challenges, and Recommendations for an Evolving Approach Janeen Madan Keller, Amanda Glassman INTRODUCTION Market shaping and procurement constitute a core approach to achieve Gavi’s mission to accelerate access to and increase equitable coverage of vaccines.1 Gavi drives lower prices and ensures the supply of high-quality vaccines through a range of tools such as pooling demand with assured funding, of- fering multi-year contracts, and encouraging new suppliers to enter the market, among others.2 Gavi has made notable progress, including securing a sustainable and affordable supply of pentavalent, pneumococcal conjugate (PCV), and rotavirus vaccines;3 expanding and diversifying the manufac- turer base;4 and developing demand forecasts to give manufacturers longer-term market visibility.5 These efforts have no doubt provided benefits to Gavi-supported countries, and they have also had some positive spillovers in Gavi-ineligible countries. Yet several challenges—stemming in part from countries transitioning from Gavi support and an evolving vaccine manufacturer landscape—may impede Gavi’s ability to effectively deliver on its mis- sion in the future. The next five-year strategy (Gavi 5.0) is an opportunity to evolve—and possibly broaden—Gavi’s role in market shaping and procurement. Looking ahead, Gavi will need to more carefully assess the implications of its market shaping strategies beyond Gavi-supported countries— and consider ways to potentially extend its benefits to the entire universe of low- and middle-income 1 See the accompanying note in this series, “Gavi’s Approach to Health Systems Strengthening (HSS): Reforms for Enhanced Effectiveness and Relevance in the 2021-2025 Strategy,” which focuses on delivery platforms to ensure those vaccines reach their target populations—another key pillar of Gavi’s vaccine support. -
Candidate SARS-Cov-2 Vaccines in Advanced Clinical Trials: Key Aspects Compiled by John D
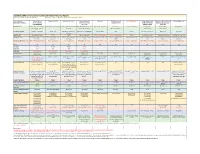
Candidate SARS-CoV-2 Vaccines in Advanced Clinical Trials: Key Aspects Compiled by John D. Grabenstein, RPh, PhD All dates are estimates. All Days are based on first vaccination at Day 0. Vaccine Sponsor Univ. of Oxford ModernaTX USA BioNTech with Pfizer Johnson & Johnson Novavax Sanofi Pasteur with CureVac with Bayer CanSino Biologics with Sinopharm (China National Sinovac Biotech Co. [with Major Partners] (Jenner Institute) (Janssen Vaccines & GlaxoSmithKline Academy of Military Biotec Group) (Beijing IBP, with AstraZeneca Prevention) Medical Sciences Wuhan IBP) Headquarters Oxford, England; Cambridge, Cambridge, Massachusetts Mainz, Germany; New York, New Brunswick, New Jersey Gaithersburg, Maryland Lyon, France; Tübingen, Germany Tianjin, China; Beijing, China; Beijing, China England, Gothenburg, New York (Leiden, Netherlands) Brentford, England Beijing, China Wuhan, China Sweden Product Designator ChAdOx1 or AZD1222 mRNA-1273 BNT162b2, tozinameran, Ad26.COV2.S, JNJ-78436735 NVX-CoV2373 TBA CVnCoV Ad5-nCoV, Convidecia BBIBP-CorV CoronaVac Comirnaty Vaccine Type Adenovirus 63 vector mRNA mRNA Adenovirus 26 vector Subunit (spike) protein Subunit (spike) protein mRNA Adenovirus 5 vector Inactivated whole virus Inactivated whole virus Product Features Chimpanzee adenovirus type Within lipid nanoparticle Within lipid nanoparticle Human adenovirus type 26 Adjuvanted with Matrix-M Adjuvanted with AS03 or Adjuvanted with AS03 Human adenovirus type 5 Adjuvanted with aluminum Adjuvanted with aluminum 63 vector dispersion dispersion vector AF03 -

What Clinicians Need to Know About Johnson & Johnson's Janssen COVID-19 Vaccine
Centers for Disease Control and Prevention Center for Preparedness and Response What Clinicians Need to Know About Johnson & Johnson’s Janssen COVID-19 Vaccine Clinician Outreach and Communication Activity (COCA) Webinar Tuesday, March 2, 2021 To Ask a Question ▪ All participants joining us today are in listen-only mode. ▪ Using the Webinar System – Click the “Q&A” button. – Type your question in the “Q&A” box. – Submit your question. ▪ The video recording of this COCA Call will be posted at https://emergency.cdc.gov/coca/calls/2021/callinfo_030221.asp and available to view on-demand a few hours after the call ends. ▪ If you are a patient, please refer your questions to your healthcare provider. ▪ For media questions, please contact CDC Media Relations at 404-639-3286, or send an email to [email protected]. Today’s Presenters ▪ Sarah Mbaeyi, MD, MPH CDR, U.S. Public Health Service Medical Officer National Center for Immunization and Respiratory Diseases Centers for Disease Control and Prevention ▪ Sara Oliver, MD LCDR, U.S. Public Health Service Co-lead, Advisory Committee for Immunization Practices COVID-19 Vaccines Work Group COVID-19 Response Centers for Disease Control and Prevention ▪ Kathleen Dooling, MD, MPH Medical Officer Co-lead, Advisory Committee for Immunization Practices COVID-19 Vaccines Work Group COVID-19 Response Centers for Disease Control and Prevention ACIP COVID-19 Vaccines What Clinicians Need to Know about Johnson and Johnson’s Janssen COVID-19 vaccine Sara Oliver MD, MSPH Sarah Mbaeyi MD, MPH Kathleen Dooling MD, MPH March 2, 2021 For more information: www.cdc.gov/COVID19 Outline: 1) Safety and efficacy of Janssen COVID-19 vaccines Dr. -
COVID-19 Vaccine Communication Guide Presented By
COVID-19 Vaccine Communication Guide Presented by In collaboration with Table of Contents Purpose ......................................................................................................................................................... 3 What vaccines are available for COVID-19? ................................................................................................... 3 How do the vaccines work? ............................................................................................................................ 3 How many shots will I need? .......................................................................................................................... 4 How effective are the different vaccines? ....................................................................................................... 4 How do we know if the COVID-19 vaccines are safe? ..................................................................................... 4 What are side-effects of the vaccine? ............................................................................................................. 5 Vaccine Hesitancy .......................................................................................................................................... 5 COVID Vaccine Communication Strategies ..................................................................................................... 5 Reflection ................................................................................................................................................................