Narcolepsy and Influenza Vaccination—The Inappropriate Awakening of Immunity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Pipeline of Medications to Treat Substance Use Disorders
Pipeline of Medications to Treat Substance Use Disorders Iván D. Montoya, M.D., M.P.H. Clinical Director and Deputy Director Division of Therapeutics and Medical Consequences NIDA • Cocaine Outline • Methamphetamine • Cannabis Past-Year Prevalence Per 1,000 1,000 People Per NSDUH, 2018 Past-Year Prevalence Per 1,000 1,000 People Per NSDUH, 2018 Number of Overdose Deaths CDC, 2018 Molecular Neurobiology of Stimulant Use Disorders Glutamate Enkephalin or Excitatory Input Dynorphin Inhibitory Neuron k Opioid Dopamine Receptors Enkephalin Receptors Inhibitory Dopamine Neuron GABA Neuron Neuron m Opioid REWARD Receptors GABA-A Receptors GABA Inhibitory Feedback GABA Presynaptic Inhibitory Opioid Neuron Receptors (m, d?) Ventral Tegmental Area Nucleus Accumbens (VTA) (NAc) Adapted from Koop, 2016 • 5HT2c Agonist - Lorcaserin (Belviq XR®) • Orexin 1 antagonists Cocaine • EMB-101 (Oxazepam + Metyrapone) • Buprenorphine + Opioid Antagonist – Clinical Studies • Ketamine • Oxytocin • L-Tetrahydropalmatine (L-THP) 5-HT2C Agonist - Lorcaserin • Clinically available • Selective agonist • Modulate mesolimbic dopamine, decreasing dopamine release • FDA-approved for weight loss • Lorcaserin (Belviq®)10 mg bid • Lorcaserin XR (Belviq XR®) 20 mg qd • Schedule IV • Arena Pharmaceuticals - Eisai Inc. Lorcaserin Pre-clinical Studies - Stimulants • Decrease cocaine self-administration and the reinstatement of responding for cocaine (Grottick et al., 2000; Burmeister et al., 2004; Burbassi and Cervo 2008; Cunningham et al., 2011; Manvich et al., 2012; RüediBettschen -

Characterizing Immunogenetic Factors Associated with Influenza Cross- Reactive Responses and Disease Severity
Characterizing immunogenetic factors associated with Influenza cross- reactive responses and disease severity By Dr. Yoav Keynan M.D A Thesis submitted to the Faculty of Graduate Studies of The University of Manitoba in partial fulfilment of the requirements of the degree of DOCTOR OF PHILOSOPHY Department of Medical Microbiology University of Manitoba Winnipeg Copyright © 2013 by Yoav Keynan Acknowledgements: To my committee members: Dr. Coombs, Dr. Aoki, Dr. Soussi-gounni for your patience and invaluable advice, with diverse backgrounds, your input has been instrumental to the completion of this project. To my mentor, Dr. Fowke- for making my decision to migrate to your lab the best career decision I have made; for guiding me in this research project and for being an advocate and supporter along the course of the years. The most important lessons I have learned from you are not limited to science or grant writing, but more importantly, the optimism and positive attitude (sometimes bordering with delusion) that instills belief and motivation. To Dr. Rubinstein- for your advice and mentoring during the combined infectious diseases and PhD training. For the open doors, listening and support along the frequently bifurcating paths. To the Fowke lab team past and present- that make this lab a second home. Special thanks to Steve for your assistance over the past 8 years. To Dr. Plummer, for giving me the initial opportunity to embark on a research career in Winnipeg. To Dr. Ball for your support and collaboration. To the Ball Lab members, for the numerous fruitful discussions. To Dr. Meyers for the numerous projects and continued collaboration. -

Dual Orexin Receptor Antagonist Induces Changes in Core Body
www.nature.com/scientificreports Corrected: Author Correction OPEN Dual orexin receptor antagonist induces changes in core body temperature in rats after exercise Tristan Martin1, Yves Dauvilliers2, Ouma-Chandrou Koumar1, Valentine Bouet1, Thomas Freret1, Stéphane Besnard1, François Dauphin1 & Nicolas Bessot1* Hypothalamic orexin neurons are involved in various physiological functions, including thermoregulation. The orexinergic system has been considered as a potent mediator of the exercise response. The present study describes how the antagonization of the orexinergic system by a dual orexin receptor antagonist (DORA) modifes the thermoregulatory process during exercise. Core Body Temperature (CBT) and Spontaneous Locomotor Activity (SLA) of 12 male Wistar rats were recorded after either oral administration of DORA (30 mg/kg or 60 mg/kg) or placebo solution, both at rest and in exercise conditions with treadmill running. DORA ingestion decreased SLA for 8 hours (p < 0.001) and CBT for 4 hours (p < 0.01). CBT (°C) response was independent of SLA. The CBT level decreased from the beginning to the end of exercise when orexin receptors were antagonized, with a dose-dependent response (39.09 ± 0.36 and 38.88 ± 0.28 for 30 and 60 mg/kg; p < 0.001) compared to placebo (39.29 ± 0.31; p < 0.001). CBT increased during exercise was also blunted after DORA administration, but without dose efects of DORA. In conclusion, our results favor the role of orexin in the thermoregulation under stress related to exercise conditions. Core Body Temperature (CBT) is modulated by heat production and dissipation mechanisms controlled by the hypothalamus. Tis generates patterns of autonomic, endocrine, motor, and behavioral responses to adapt to environmental challenges1. -

Evidence Assessment STRATEGIC ADVISORY GROUP of EXPERTS (SAGE) on IMMUNIZATION Meeting 15 March 2021
Evidence Assessment STRATEGIC ADVISORY GROUP OF EXPERTS (SAGE) ON IMMUNIZATION Meeting 15 March 2021 FOR RECOMMENDATION BY SAGE Prepared by the SAGE Working Group on COVID-19 vaccines EVIDENCE ASSESSMENT: Ad26.COV2.S COVID-19 vaccine Key evidence to inform policy recommendations on the use of Ad26.COV2.S COVID-19 vaccine Evidence retrieval • Based on WHO and Cochrane living mapping and living systematic review of Covid-19 trials (www.covid-nma.com/vaccines) Retrieved evidence Majority of data considered for policy recommendations on Ad26.COV2.S Covid-19 vaccine are published in scientific peer reviewed journals: • Interim Results of a Phase 1–2a Trial of Ad26.COV2.S Covid-19 Vaccine. NEJM. February 2021. DOI: 10.1056/NEJMoa2034201. Jerald Sadoff, Mathieu Le Gars, Georgi Shukarev, et al. • FDA briefing document Janssen Ad26.COV2.S (COVID-19) Vaccine • Ad26 platform literature: Custers et al. Vaccines based on the Ad26 platform; Vaccine 2021 Quality assessment Type of bias Randomization Deviations from Missing outcome Measurement of Selection of the Overall risk of intervention data the outcome reported results bias Working Group Low Low Low Low Low LOW judgment 1 EVIDENCE ASSESSMENT The SAGE Working Group specifically considered the following issues: 1. Trial endpoints used in comparison with other vaccines Saad Omer 2. Evidence on vaccine efficacy in the total population and in different subgroups Cristiana Toscano 3. Evidence of vaccine efficacy against asymptomatic infections, reducing severity, hospitalisations, deaths, and efficacy against virus variants of concern Annelies Wilder-Smith 4. Vaccination after SARS-CoV2 infection. 5. Evidence on vaccine safety in the total population and in different subgroups Sonali Kochhar 6. -

Diverse Functional Autoantibodies in Patients with COVID-19
medRxiv preprint doi: https://doi.org/10.1101/2020.12.10.20247205; this version posted December 11, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Diverse Functional Autoantibodies in Patients with COVID-19 Eric Y. Wang1,*, Tianyang Mao1,*, Jon Klein1,*, Yile Dai1,*, John D. Huck1, Feimei Liu1, Neil S. Zheng1, Ting Zhou1, Benjamin Israelow1, Patrick Wong1, Carolina Lucas1, Julio Silva1, Ji Eun Oh1, Eric Song1, Emily S. Perotti1, Suzanne Fischer1, Melissa Campbell5, John B. Fournier5, Anne L. Wyllie3, Chantal B. F. Vogels3, Isabel M. Ott3, Chaney C. Kalinich3, Mary E. Petrone3, Anne E. Watkins3, Yale IMPACT Team¶, Charles Dela Cruz4, Shelli F. Farhadian5, Wade L. Schulz6,7, Nathan D. Grubaugh3, Albert I. Ko3,5, Akiko Iwasaki1,3,8,#, Aaron M. Ring1,2,# 1 Department of Immunobiology, Yale School of Medicine, New Haven, CT, USA 2 Department of Pharmacology, Yale School of Medicine, New Haven, CT, USA 3 Department of Epidemiology of Microbial Diseases, Yale School of Public Health, New Haven, CT, USA 4 Department of Medicine, Section of Pulmonary and Critical Care Medicine, Yale School of Medicine, New Haven, CT, USA 5 Department of Internal Medicine (Infectious Diseases), Yale School of Medicine, New Haven, CT, USA 6 Department of Laboratory Medicine, Yale School of Medicine, New Haven, CT, USA 7 Center for Outcomes Research and Evaluation, Yale-New Haven Hospital, New Haven, CT, USA 8 Howard Hughes Medical Institute, Chevy Chase, MD, USA * These authors contributed equally to this work ¶ A list of authors and their affiliations appears at the end of the paper # Correspondence: [email protected] (A.M.R.); [email protected] (A.I.) 1 NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. -

Molecular Insights Into the Transmembrane Domain of the Thyrotropin Receptor
Molecular Insights into the Transmembrane Domain of the Thyrotropin Receptor Vanessa Chantreau, Bruck Taddese, Mathilde Munier, Louis Gourdin, Daniel Henrion, Patrice Rodien, Marie Chabbert To cite this version: Vanessa Chantreau, Bruck Taddese, Mathilde Munier, Louis Gourdin, Daniel Henrion, et al.. Molecu- lar Insights into the Transmembrane Domain of the Thyrotropin Receptor. PLoS ONE, Public Library of Science, 2015, 10 (11), pp.e0142250. 10.1371/journal.pone.0142250. hal-02318838 HAL Id: hal-02318838 https://hal.archives-ouvertes.fr/hal-02318838 Submitted on 17 Oct 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. RESEARCH ARTICLE Molecular Insights into the Transmembrane Domain of the Thyrotropin Receptor Vanessa Chantreau1, Bruck Taddese1, Mathilde Munier1, Louis Gourdin1,2, Daniel Henrion1, Patrice Rodien1,2, Marie Chabbert1* 1 UMR CNRS 6214 –INSERM 1083, Laboratory of Integrated Neurovascular and Mitochondrial Biology, University of Angers, Angers, France, 2 Reference Centre for the pathologies of hormonal receptivity, Department of Endocrinology, Centre Hospitalier Universitaire of Angers, Angers, France * [email protected] Abstract The thyrotropin receptor (TSHR) is a G protein-coupled receptor (GPCR) that is member of the leucine-rich repeat subfamily (LGR). -

Neuropeptides Controlling Energy Balance: Orexins and Neuromedins
Neuropeptides Controlling Energy Balance: Orexins and Neuromedins Joshua P. Nixon, Catherine M. Kotz, Colleen M. Novak, Charles J. Billington, and Jennifer A. Teske Contents 1 Brain Orexins and Energy Balance ....................................................... 79 1.1 Orexin............................................................................... 79 2 Orexin and Feeding ....................................................................... 80 3 Orexin and Arousal ....................................................................... 83 J.P. Nixon • J.A. Teske Veterans Affairs Medical Center, Research Service (151), Minneapolis, MN, USA Department of Food Science and Nutrition, University of Minnesota, 1334 Eckles Avenue, St. Paul, MN 55108, USA Minnesota Obesity Center, University of Minnesota, 1334 Eckles Avenue, St. Paul, MN 55108, USA C.M. Kotz (*) Veterans Affairs Medical Center, GRECC (11 G), Minneapolis, MN, USA Veterans Affairs Medical Center, Research Service (151), Minneapolis, MN, USA Department of Food Science and Nutrition, University of Minnesota, 1334 Eckles Avenue, St. Paul, MN 55108, USA Minnesota Obesity Center, University of Minnesota, 1334 Eckles Avenue, St. Paul, MN 55108, USA e-mail: [email protected] C.M. Novak Department of Biological Sciences, Kent State University, Kent, OH, USA C.J. Billington Veterans Affairs Medical Center, Research Service (151), Minneapolis, MN, USA Veterans Affairs Medical Center, Endocrine Unit (111 G), Minneapolis, MN, USA Department of Food Science and Nutrition, University of Minnesota, 1334 Eckles Avenue, St. Paul, MN 55108, USA Minnesota Obesity Center, University of Minnesota, 1334 Eckles Avenue, St. Paul, MN 55108, USA H.-G. Joost (ed.), Appetite Control, Handbook of Experimental Pharmacology 209, 77 DOI 10.1007/978-3-642-24716-3_4, # Springer-Verlag Berlin Heidelberg 2012 78 J.P. Nixon et al. 4 Orexin Actions on Endocrine and Autonomic Systems ................................. 84 5 Orexin, Physical Activity, and Energy Expenditure .................................... -

ESCMID Online Lecture Library © by Author
Albert Osterhaus Head Dept Virology Chairman ESWI CSO Viroclinics-Biosciences BV Library Pandemic flu and the anti-H1N1 vaccine: Lecture a retrospective view. author Onlineby © ESCMID ESCMID conference on the impact of vaccines on Public Health Prague, 2nd April 2011 Human influenza: three appearances Library Seasonal influenza (A: H3N2, H1N1; B) Lecture Avian influenza author (A: H7N7, H5N1…)Online by © PandemicESCMID influenza (A: H1N1, H2N2, H3N2, H1N1…?) INFLUENZA A VIRUS Recent zoonotic transmissions Library Subtype Country Year # Cases # Deaths H7N7 UK Lecture1996 1 0 H5N1 Hongkong 1997 18 6 H9N2 SE-Asia 1999author >2 0 H5N1 HongkongOnlineby 2003 2? 1 H7N7 Netherlands© 2003 89 1 H7N2 USA 2003 1 0 H7N3 Canada 2004 2 0 H5N1ESCMIDSE-Asia/M-East/ 2003-11 .>500 >300* Europe/W-Africa *CFR ~ 60% Library Lecture author Onlineby © ESCMID Confirmed H5N1 avian influenza virus endemic areas (poultry and wild birds) since 2003 Avian influenza A H5N1 virus - HA: Receptor specificity - Library Shinya et al., Nature 440, 2006 Lecture Van Riel et al., Science 2006 author Van Riel et al., Online Am J Pathol 2007 by Van Riel et al., © Am J Pathol 2009 Van Riel et al., ESCMID Am J Pathol 2010 Library Lecture author Onlineby © ESCMID Introduction - Attachment to the upper respiratory tract - Seasonal H3N2 Pandemic H1N1 HPAIV H5N1 Last four pandemics Library Lecture Credit: US National Museum of Health and Medicine author 1918 1957Online 1968 2009 “Spanish Flu” “Asian Flu” by “Hong Kong Flu” © ”Swine Flu” >40 million deaths 1-4 million deaths 1-4million deaths ??? A(H1N1)ESCMIDA(H2N2) A(H3N2) A(H1N1) Library Lecture author Onlineby © ESCMID Air traffic from Mexico ~ 1998 PB2,PA: Triple reassortant ~ 1968 ~ 1998 PB1: LibraryN-America ~ 1918 Classical swine HA, NP, NS: Lecture ~ 1979 NA, MA: authorEurasian swine Eurasia Onlineby A/California/4/2009 © PB2 PB1 The H1N1v flu virus PA Courtesy: Ron Fouchier HA NP ESCMID NA MA NS Library Lecture author Onlineby © ESCMID The Mexican flu virus.. -

Identification of Neuropeptide Receptors Expressed By
RESEARCH ARTICLE Identification of Neuropeptide Receptors Expressed by Melanin-Concentrating Hormone Neurons Gregory S. Parks,1,2 Lien Wang,1 Zhiwei Wang,1 and Olivier Civelli1,2,3* 1Department of Pharmacology, University of California Irvine, Irvine, California 92697 2Department of Developmental and Cell Biology, University of California Irvine, Irvine, California 92697 3Department of Pharmaceutical Sciences, University of California Irvine, Irvine, California 92697 ABSTRACT the MCH system or demonstrated high expression lev- Melanin-concentrating hormone (MCH) is a 19-amino- els in the LH and ZI, were tested to determine whether acid cyclic neuropeptide that acts in rodents via the they are expressed by MCH neurons. Overall, 11 neuro- MCH receptor 1 (MCHR1) to regulate a wide variety of peptide receptors were found to exhibit significant physiological functions. MCH is produced by a distinct colocalization with MCH neurons: nociceptin/orphanin population of neurons located in the lateral hypothala- FQ opioid receptor (NOP), MCHR1, both orexin recep- mus (LH) and zona incerta (ZI), but MCHR1 mRNA is tors (ORX), somatostatin receptors 1 and 2 (SSTR1, widely expressed throughout the brain. The physiologi- SSTR2), kisspeptin recepotor (KissR1), neurotensin cal responses and behaviors regulated by the MCH sys- receptor 1 (NTSR1), neuropeptide S receptor (NPSR), tem have been investigated, but less is known about cholecystokinin receptor A (CCKAR), and the j-opioid how MCH neurons are regulated. The effects of most receptor (KOR). Among these receptors, six have never classical neurotransmitters on MCH neurons have been before been linked to the MCH system. Surprisingly, studied, but those of most neuropeptides are poorly several receptors thought to regulate MCH neurons dis- understood. -

Pre-Existing Immunity Provides a Barrier to Airborne Transmission of Influenza Viruses
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.15.103747; this version posted June 15, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Pre-existing immunity provides a barrier to airborne transmission of influenza viruses Valerie Le Sage1, Jennifer E. Jones1, Karen A. Kormuth1^, William J. Fitzsimmons2, Eric Nturibi1, Gabriella H. Padovani1, Claudia P. Arevalo4, Andrea J. French1, Annika J. Avery1, Richard Manivanh1, Elizabeth E. McGrady1, Amar R. Bhagwat1^, Adam S. Lauring2,3, Scott E. Hensley4, Seema S. Lakdawala1,5* 1 - Department of Microbiology and Molecular Genetics, University of Pittsburgh School of Medicine, Pittsburgh, PA 2 – Division of Infectious Diseases, Department of Internal Medicine, University of Michigan, Ann Arbor, MI 3 – Department of Microbiology and Immunology, University of Michigan, Ann Arbor, MI 4 – Department of Microbiology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA 5 - Center for Vaccine Research, University of Pittsburgh School of Medicine, Pittsburgh, PA 15219 * Send all correspondence to [email protected] ^ Current position - KAK is an Assistant Professor at Bethany College, Bethany, WV and ARB is a Senior Project Engineer at II-VI Aerospace & Defense in Dayton, OH. Abstract Human-to-human transmission of influenza viruses is a serious public health threat, yet the precise role of immunity from previous infections on the susceptibility to airborne viruses is still unknown. Using human seasonal influenza viruses in a ferret model, we examined the roles of exposure duration and heterosubtypic immunity on influenza transmission. We found that airborne transmission of seasonal influenza strains is abrogated in recipient animals with pre-existing non- neutralizing immunity, indicating that transmissibility of a given influenza virus strain should be examined in the context of ferrets that are not immunologically naïve. -

Improving the Regulatory Response to Vaccine Development During a Public Health Emergency
Every Minute Matters: Improving the Regulatory Response to Vaccine Development During a Public Health Emergency RASHMI BORAH* ABSTRACT In recent months, our lives have been turned upside down by the novel coronavirus (COVID-19) emergency. With no cure or vaccine in sight, millions of people have contracted the virus, and the death toll has surpassed that of World War I in a fraction of the time. In fact, the past decade has been marked by a series of highly publicized public health emergencies, including the devastating Ebola and Zika virus global outbreaks. Some of this panic arose from a failure to manufacture and distribute vaccines in a timely fashion. This failure occurred despite having several viable vaccine candidates, adequate funding, and strong public support for the vaccines. This Article explains how these failures are the consequence of a complex network of existing regulatory pathways and insufficient incentives to produce affordable vaccinations during a public health emergency. Fortunately, there are several ways that both the U.S. Patent and Trademark Office and the U.S. Food and Drug Administration can improve and streamline the process of patenting, approving, manufacturing, and distributing a vaccination. The last decade has demonstrated that public health emergencies occur quickly, and affected communities cannot afford the delays and mishaps that characterized the vaccine response to COVID-19, Ebola, and Zika. This Article explores three ways to facilitate the development and distribution of vaccinations during a public health emergency. First, the U.S. Patent and Trademark Office can establish a dedicated public health emergency patent pathway for vaccine technology developed specifically in response to a public health emergency. -
Candidate SARS-Cov-2 Vaccines in Advanced Clinical Trials: Key Aspects Compiled by John D
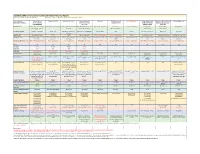
Candidate SARS-CoV-2 Vaccines in Advanced Clinical Trials: Key Aspects Compiled by John D. Grabenstein, RPh, PhD All dates are estimates. All Days are based on first vaccination at Day 0. Vaccine Sponsor Univ. of Oxford ModernaTX USA BioNTech with Pfizer Johnson & Johnson Novavax Sanofi Pasteur with CureVac with Bayer CanSino Biologics with Sinopharm (China National Sinovac Biotech Co. [with Major Partners] (Jenner Institute) (Janssen Vaccines & GlaxoSmithKline Academy of Military Biotec Group) (Beijing IBP, with AstraZeneca Prevention) Medical Sciences Wuhan IBP) Headquarters Oxford, England; Cambridge, Cambridge, Massachusetts Mainz, Germany; New York, New Brunswick, New Jersey Gaithersburg, Maryland Lyon, France; Tübingen, Germany Tianjin, China; Beijing, China; Beijing, China England, Gothenburg, New York (Leiden, Netherlands) Brentford, England Beijing, China Wuhan, China Sweden Product Designator ChAdOx1 or AZD1222 mRNA-1273 BNT162b2, tozinameran, Ad26.COV2.S, JNJ-78436735 NVX-CoV2373 TBA CVnCoV Ad5-nCoV, Convidecia BBIBP-CorV CoronaVac Comirnaty Vaccine Type Adenovirus 63 vector mRNA mRNA Adenovirus 26 vector Subunit (spike) protein Subunit (spike) protein mRNA Adenovirus 5 vector Inactivated whole virus Inactivated whole virus Product Features Chimpanzee adenovirus type Within lipid nanoparticle Within lipid nanoparticle Human adenovirus type 26 Adjuvanted with Matrix-M Adjuvanted with AS03 or Adjuvanted with AS03 Human adenovirus type 5 Adjuvanted with aluminum Adjuvanted with aluminum 63 vector dispersion dispersion vector AF03