ESCMID Online Lecture Library © by Author
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Mix-And-Match of Vaccines Will Definitely Not Cause a Safety Issue”
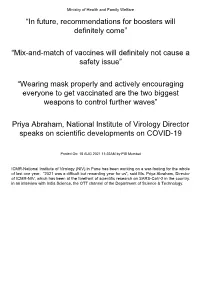
Ministry of Health and Family Welfare “In future, recommendations for boosters will definitely come” “Mix-and-match of vaccines will definitely not cause a safety issue” “Wearing mask properly and actively encouraging everyone to get vaccinated are the two biggest weapons to control further waves” Priya Abraham, National Institute of Virology Director speaks on scientific developments on COVID-19 Posted On: 18 AUG 2021 11:22AM by PIB Mumbai ICMR-National Institute of Virology (NIV) in Pune has been working on a war-footing for the whole of last one year. “2021 was a difficult but rewarding year for us”, said Ms. Priya Abraham, Director of ICMR-NIV, which has been at the forefront of scientific research on SARS-CoV-2 in the country. in an interview with India Science, the OTT channel of the Department of Science & Technology. Giving a quick overview of vaccine development process carried out at the institute which has been at the forefront of scientific research on SARS-CoV-2 in the country, she explained: “We quickly isolated and gave a strain to Bharat Biotech International Limited (BBIL) by the end of April (2020), after which they developed a whole virion-inactivated vaccine in the month of May and gave us back for review. We checked it for its complete inactivation, did its complete characterisation and started pre-clinical trials on hamsters and non-human primates, that is, monkeys. Those are very difficult experiments to do. These were conducted in our highest Bio-Safety Level-4 level containment facilities. In the next phase, we assisted them in the Phase I, II and III clinical trials in areas such as diagnostic aspect and laboratory support”. -

US and International Responses to the Global Spread of Avian
Order Code RL33219 CRS Report for Congress Received through the CRS Web U.S. and International Responses to the Global Spread of Avian Flu: Issues for Congress Updated January 11, 2006 Tiaji Salaam-Blyther and Emma Chanlett-Avery Coordinators Foreign Affairs, Defense, and Trade Division Congressional Research Service ˜ The Library of Congress U.S. and International Responses to the Global Spread of Avian Flu: Issues for Congress Summary One strain of avian influenza currently identified in Asia and Europe is known as Influenza A/H5N1. Although it is a bird flu, it has infected a relatively small number of people — killing around 50% of those infected. Scientists are concerned that H5N1 may cause the next influenza pandemic. Flu pandemics have occurred cyclically, roughly between every 30 and 50 years. Since 1997, when the first human contracted H5N1 in Hong Kong, the virus has resurfaced and spread to more than a dozen countries in Asia and Europe — infecting more than 140 people and killing approximately half. Britain and Taiwan both reported avian flu cases of H5N1 in 2005. In the latter cases, the infected birds were identified as imports, and died in quarantine. A global influenza pandemic could have a number of consequences. Global competition for existing vaccines and treatments could ensue. Some governments might restrict the export of vaccines or other supplies in order to treat their own population. Some countries might face a shortage of vaccines, antiviral medication, or other medical equipment, because of limited global supply. Hospitality and airline industries, and international trade could be negatively impacted. If global travel and trade were to suddenly drop, there could be productivity losses and service disruptions. -

Considerations for Causality Assessment of Neurological And
Occasional essay J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp-2021-326924 on 6 August 2021. Downloaded from Considerations for causality assessment of neurological and neuropsychiatric complications of SARS- CoV-2 vaccines: from cerebral venous sinus thrombosis to functional neurological disorder Matt Butler ,1 Arina Tamborska,2,3 Greta K Wood,2,3 Mark Ellul,4 Rhys H Thomas,5,6 Ian Galea ,7 Sarah Pett,8 Bhagteshwar Singh,3 Tom Solomon,4 Thomas Arthur Pollak,9 Benedict D Michael,2,3 Timothy R Nicholson10 For numbered affiliations see INTRODUCTION More severe potential adverse effects in the open- end of article. The scientific community rapidly responded to label phase of vaccine roll- outs are being collected the COVID-19 pandemic by developing novel through national surveillance systems. In the USA, Correspondence to SARS- CoV-2 vaccines (table 1). As of early June Dr Timothy R Nicholson, King’s roughly 372 adverse events have been reported per College London, London WC2R 2021, an estimated 2 billion doses have been million doses, which is a lower rate than expected 1 2LS, UK; timothy. nicholson@ administered worldwide. Neurological adverse based on the clinical trials.6 kcl. ac. uk events following immunisation (AEFI), such as In the UK, adverse events are reported via the cerebral venous sinus thrombosis and demyelin- MB and AT are joint first Coronavirus Yellow Card reporting website. As of ating episodes, have been reported. In some coun- authors. early June 2021, approximately 250 000 Yellow tries, these have led to the temporary halting of BDM and TRN are joint senior Cards have been submitted, equating to around authors. -

Characterizing Immunogenetic Factors Associated with Influenza Cross- Reactive Responses and Disease Severity
Characterizing immunogenetic factors associated with Influenza cross- reactive responses and disease severity By Dr. Yoav Keynan M.D A Thesis submitted to the Faculty of Graduate Studies of The University of Manitoba in partial fulfilment of the requirements of the degree of DOCTOR OF PHILOSOPHY Department of Medical Microbiology University of Manitoba Winnipeg Copyright © 2013 by Yoav Keynan Acknowledgements: To my committee members: Dr. Coombs, Dr. Aoki, Dr. Soussi-gounni for your patience and invaluable advice, with diverse backgrounds, your input has been instrumental to the completion of this project. To my mentor, Dr. Fowke- for making my decision to migrate to your lab the best career decision I have made; for guiding me in this research project and for being an advocate and supporter along the course of the years. The most important lessons I have learned from you are not limited to science or grant writing, but more importantly, the optimism and positive attitude (sometimes bordering with delusion) that instills belief and motivation. To Dr. Rubinstein- for your advice and mentoring during the combined infectious diseases and PhD training. For the open doors, listening and support along the frequently bifurcating paths. To the Fowke lab team past and present- that make this lab a second home. Special thanks to Steve for your assistance over the past 8 years. To Dr. Plummer, for giving me the initial opportunity to embark on a research career in Winnipeg. To Dr. Ball for your support and collaboration. To the Ball Lab members, for the numerous fruitful discussions. To Dr. Meyers for the numerous projects and continued collaboration. -

1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant
medRxiv preprint doi: https://doi.org/10.1101/2021.05.14.21257248; this version posted May 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. 1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant-Produced Virus-Like Particle 2 Vaccine for Covid-19 in Healthy Adults Aged 18-64 and Older Adults Aged 65 and Older 3 Authors: Philipe Gobeil1, Stéphane Pillet1, Annie Séguin1, Iohann Boulay1, Asif Mahmood1, 4 Donald C Vinh 2, Nathalie Charland1, Philippe Boutet3, François Roman3, Robbert Van Der 5 Most4, Maria de los Angeles Ceregido Perez3, Brian J Ward1,2†, Nathalie Landry1† 6 Affiliations: 1 Medicago Inc., 1020 route de l’Église office 600, Québec, QC, Canada, G1V 7 3V9; 2 Research Institute of the McGill University Health Centre, 1001 Decarie St, Montreal, 8 QC H4A 3J1; 3 GlaxoSmithKline Biologicals SA (Vaccines), Avenue Fleming 20, 1300 Wavre, 9 Belgium; 4 GlaxoSmithKline Biologicals SA (Vaccines), rue de l’Institut 89, 1330 Rixensart, 10 Belgium; † These individuals are equally credited as senior authors. 11 * Corresponding author: Nathalie Landry, 1020 Route de l’Église, Bureau 600, Québec, Qc, 12 Canada, G1V 3V9; Tel. 418 658 9393; Fax. 418 658 6699; [email protected] 13 Abstract 14 The rapid spread of SARS-CoV-2 globally continues to impact humanity on a global scale with 15 rising morbidity and mortality. Despite the development of multiple effective vaccines, new 16 vaccines continue to be required to supply ongoing demand. -

Prevalence and Determinants of Vaccine Hesitancy and Vaccines Recommendation Discrepancies Among General Practitioners in French-Speaking Parts of Belgium
Article Prevalence and Determinants of Vaccine Hesitancy and Vaccines Recommendation Discrepancies among General Practitioners in French-Speaking Parts of Belgium Cathy Gobert 1, Pascal Semaille 2, Thierry Van der Schueren 3 , Pierre Verger 4 and Nicolas Dauby 1,5,6,* 1 Department of Infectious Diseases, CHU Saint-Pierre, Université Libre de Bruxelles (ULB), 1000 Bruxelles, Belgium; [email protected] 2 Department of General Medicine, Université Libre de Bruxelles (ULB), 1070 Bruxelles, Belgium; [email protected] 3 Scientific Society of General Practice, 1060 Bruxelles, Belgium; [email protected] 4 Southeastern Health Regional Observatory (ORS PACA), 13005 Marseille, France; [email protected] 5 School of Public Health, Université Libre de Bruxelles (ULB), 1070 Bruxelles, Belgium 6 Institute for Medical Immunology, Université Libre de Bruxelles (ULB), 1070 Bruxelles, Belgium * Correspondence: [email protected] Abstract: General practitioners (GPs) play a critical role in patient acceptance of vaccination. Vaccine hesitancy (VH) is a growing phenomenon in the general population but also affects GPs. Few data exist on VH among GPs. The objectives of this analysis of a population of GPs in the Belgian Wallonia-Brussels Federation (WBF) were to: (1) determine the prevalence and the features of VH, (2) identify the correlates, and (3) estimate the discrepancy in vaccination’s behaviors between the GPs’ children and the recommendations made to their patients. An online survey was carried out Citation: Gobert, C.; Semaille, P.; Van among the population of general practitioners practicing in the WBF between 7 January and 18 der Schueren, T.; Verger, P.; Dauby, N. March 2020. A hierarchical cluster analysis was carried out based on various dimensions of vaccine Prevalence and Determinants of hesitancy: perception of the risks and the usefulness of vaccines as well as vaccine recommendations Vaccine Hesitancy and Vaccines for their patients. -

Patient Information Leaflet Pandemrix Suspension and Emulsion For
gentamicin sulphate (antibiotic) or sodium Patient Information deoxycholate. Signs of an allergic reaction may Leaflet include itchy skin rash, shortness of breath and swelling of the face or tongue. However, in a pandemic situation, it may be Pandemrix suspension appropriate for you to have the vaccine provided that appropriate medical treatment is immediately and emulsion for available in case of an allergic reaction. emulsion for injection If you are not sure, talk to your doctor or nurse Pandemic influenza vaccine (H1N1) before having this vaccine. (split virion, inactivated, adjuvanted) Talk to your doctor • if you have had any allergic reaction other than For the most up-to-date information a sudden lifethreatening allergic reaction to any please consult the website of the UK ingredient contained in the vaccine, to thiomersal, Medicines and Healthcare products to egg and chicken protein, ovalbumin, Regulatory Agency at: formaldehyde, gentamicin sulphate (antibiotic) or www.mhra.gov.uk/swineflu to sodiumdeoxycholate. (see section 6. Further information). Read all of this leaflet carefully before you receive this vaccine. • if you have a severe infection with a high - Keep this leaflet. You may need to read it again. temperature (over 38°C). If this applies to you - If you have any further questions, ask your then your vaccination will usually be postponed doctor or nurse. until you are feeling better. A minor infection such - If any of the side effects gets serious, or if you as a cold should not be a problem, but your notice any side effects doctor or nurse will advise whether you could still not listed in this leaflet, please tell your doctor. -

Gsk Vaccines in 2010
GSK VACCINES IN 2010 Thomas Breuer, MD, MSc Senior Vice President Head of Global Vaccines Development GSK Biologicals Vaccines business characteristics Few global players and high barriers to entry – Complex manufacturing – Large scale investment Long product life cycles – Complex intellectual property High probability of R&D success – 70% post-POC New technology/novel products Better pricing for newer vaccines – HPV vaccines (Cervarix, Gardasil) – Pneumococcal vaccines (Synflorix, Prevnar-13) Operating margin comparable to pharmaceutical products Heightened awareness New markets 2 Research & development timelines Identify Produce Pre-Clinical Proof of Registration/ Phase I Phase II Phase III File Antigens Antigens Testing Concept Post Marketing Research (inc. Immunology) Pre-Clinical Development (inc. Formulation Science) Clinical Development (inc. Post Marketing Surveillance) Transfer Process to Manufacturing Build Facility x x Up to $10-20M Up to $50-100M $500M - $1B x x x 1-10 yrs 2-3 yrs 2-4 yrs > 1 yr GSK vaccines business 2009 sales £3.7 billion (+30%) +19% CAGR excl. H1N1 Vaccines represent 13% since 2005 of total GSK sales Sale s (£m) 4000 3500 Recent approvals: 3000 US: Cervarix 2500 EU: Synflorix 2000 Pandemic: Pandemrix; Arepanrix 1500 1000 500 0 2005 2006 2007 2008 2009 Increased Emerging Market presence Growth rate is CER 5 GSK vaccines: fastest growing part of GSK in 2009 2009 Sales Share Growth (CER) Respiratory £ 6,977m 25% +5% Consumer £ 4,654m 16% +7% Anti-virals £ 4,150m 15% +12% Vaccines £ 3,706m 13% +30% CV & Urogenital -

Influenza a (H1N1)V: EMEA Status Report
Influenza at the interface between humans and animals Influenza A (H1N1)v: EMEA Status Report John Purves, European Medicines Agency (EMEA) 30 October 2009 1 Overview of presentation z Preparedness activities (2003-2009) z Current activities (April to October 2009) z Current situation - Vaccines 2 Overview of presentation z PreparednessPreparedness activitiesactivities (2003(2003--2009)2009) z Current activities (April to October 2009) z Current situation - Vaccines 3 Highlights of pandemic preparedness activities since 2003 2004 2006/7 - 2 CHMP Guidelines - Assessor training on EMEA pandemic adopted introducing procedures & assessment issues 2009 concept of a core - CHMP recommendations on PV plan as part of - Registration of pandemic dossier (mock the RMP of pandemic vaccines MAAs Celvapan H5N1 up vaccine) - Registration of Focetria H5N1 MAA MAA 2003 2005/6 2007/8 -Extensive - EMEA publishes - Update of antiviral review by CHMP pandemic EMEA pandemic plan - EMEA Pandemic communications plan & preparatory work presentation to SANCO & ECDC at EMEA, with - EMEA Pandemic business continuity planning and industry, since exercise 2003 -Joint EMEA–NCA BCP pandemic workshop - Registration of Pandemrix H5N1 MAA 4 What is a Mock-Up Pandemic Vaccines? z Mock-up vaccine is a vaccine containing viral antigen(s) to which humans are immunologically naïve, e.g. H9N2 / H5N1. z Scientific data with a mock-up vaccine are relevant for the pandemic vaccine: » Manufacturing and quality data » Clinical experience in naïve population » Evaluation of novel concepts prior to a pandemic e.g. use of adjuvants with the objective of increasing available doses, establishment of dosing schedule 5 Mock up strategy Marketing Quality,Quality,Quality, safety,safety,safety, efficacyefficacyefficacy Authorisation CoreCoreCore dossierdossierdossier usingusingusing aaa strainstrainstrain e.g.e.g.e.g. -

Pre-Existing Immunity Provides a Barrier to Airborne Transmission of Influenza Viruses
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.15.103747; this version posted June 15, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Pre-existing immunity provides a barrier to airborne transmission of influenza viruses Valerie Le Sage1, Jennifer E. Jones1, Karen A. Kormuth1^, William J. Fitzsimmons2, Eric Nturibi1, Gabriella H. Padovani1, Claudia P. Arevalo4, Andrea J. French1, Annika J. Avery1, Richard Manivanh1, Elizabeth E. McGrady1, Amar R. Bhagwat1^, Adam S. Lauring2,3, Scott E. Hensley4, Seema S. Lakdawala1,5* 1 - Department of Microbiology and Molecular Genetics, University of Pittsburgh School of Medicine, Pittsburgh, PA 2 – Division of Infectious Diseases, Department of Internal Medicine, University of Michigan, Ann Arbor, MI 3 – Department of Microbiology and Immunology, University of Michigan, Ann Arbor, MI 4 – Department of Microbiology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA 5 - Center for Vaccine Research, University of Pittsburgh School of Medicine, Pittsburgh, PA 15219 * Send all correspondence to [email protected] ^ Current position - KAK is an Assistant Professor at Bethany College, Bethany, WV and ARB is a Senior Project Engineer at II-VI Aerospace & Defense in Dayton, OH. Abstract Human-to-human transmission of influenza viruses is a serious public health threat, yet the precise role of immunity from previous infections on the susceptibility to airborne viruses is still unknown. Using human seasonal influenza viruses in a ferret model, we examined the roles of exposure duration and heterosubtypic immunity on influenza transmission. We found that airborne transmission of seasonal influenza strains is abrogated in recipient animals with pre-existing non- neutralizing immunity, indicating that transmissibility of a given influenza virus strain should be examined in the context of ferrets that are not immunologically naïve. -

Pandemrix, INN-Influenza Vaccine (H1N1)V (Split Virion, Inactivated
EMA/388182/2016 EMEA/H/C/000832 EPAR summary for the public Pandemrix influenza vaccine (H1N1)v (split virion, inactivated, adjuvanted) This document is a summary of the European Public Assessment Report (EPAR) for Pandemrix. It explains how the Committee for Medicinal Products for Human Use (CHMP) assessed the medicine to reach its opinion in favour of granting a marketing authorisation and its recommendations on the conditions of use for Pandemrix. What is Pandemrix? Pandemrix is a vaccine that is given by injection. It contains parts of influenza (flu) viruses that have been inactivated. Pandemrix contains a flu strain called A/California/7/2009 (H1N1)v-like strain (X-179A). What is Pandemrix used for? Pandemrix is a vaccine to protect against flu caused by the A (H1N1)v 2009 virus. It should only be used if the recommended annual seasonal trivalent/quadrivalent influenza vaccine is not available and if immunisation against (H1N1)v is considered necessary. Pandemrix is given according to official recommendations. The vaccine can only be obtained with a prescription. How is Pandemrix used? Pandemrix is given as one dose, injected into the muscle of the shoulder or thigh. A second dose may be given after an interval of at least three weeks. From 10 years of age the dose is 0.5 ml; younger children aged from six months to nine years receive 0.25 ml per dose. How does Pandemrix work? Pandemrix is a vaccine. Vaccines work by ‘teaching’ the immune system (the body’s natural defences) how to defend itself against a disease. Pandemrix contains small amounts of haemagglutinins (proteins 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2016. -

Options for the Use of Human H5N1 Influenza Vaccines and the WHO H5N1 Vaccine Stockpile
Options for the use of human H5N1 influenza vaccines and the WHO H5N1 vaccine stockpile THIRD DRAFT – 02/11/07 WHO SCIENTIFIC CONSULTATION: TECHNICAL CONSIDERATIONS FOR DEVELOPING OPTIONS FOR USE OF HUMAN H5N1 INFLUENZA VACCINES AND A WHO H5N1 VACCINE STOCKPILE GENEVA, 01-03 OCTOBER 2007 GENEVA, 2007 CONTENTS Executive summary ................................................................................................... 3 1. Characteristics of human H5N1 influenza vaccines 1.1: Safety......................................................................................................................... 8 1.2: Immunogenicity....................................................................................................... 10 1.3: Cross-reactivity........................................................................................................ 12 1.4: Degree and duration of protection ........................................................................... 13 1.5: Conclusions and priority areas ................................................................................ 14 2. Options for using human H5N1 influenza vaccines................................ 16 2.1: To protect people at high risk of contracting zoonotic avian H5N1 influenza........ 17 2.2: To “prime” selected groups or whole populations in anticipation of a possible H5N1 influenza pandemic ....................................................................................... 18 2.3: To immunize selected groups or whole populations in anticipation of