Ted Freeman and the Battle for the Injured Brain: A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

BROOKLYN ESTUARY PROCESS STUDY (VOLUME I of II) By
BROOKLYN ESTUARY PROCESS STUDY (VOLUME I OF II) by Water Research Laboratory Manly Hydraulics Laboratory The Ecology Lab Coastal and Marine Geosciences The Centre for Research on Ecological Impacts of Coastal Cities Edited by B M Miller and D Van Senden Technical Report 2002/20 June 2002 (Issued October 2003) THE UNIVERSITY OF NEW SOUTH WALES SCHOOL OF CIVIL AND ENVIRONMENTAL ENGINEERING WATER RESEARCH LABORATORY BROOKLYN ESTUARY PROCESS STUDY WRL Technical Report 2002/20 June 2002 by Water Research Laboratory Manly Hydraulics Laboratory The Ecology Lab Coastal and Marine Geosciences The Centre for Research on Ecological Impacts of Coastal Cities Edited by B M Miller D Van Senden (Issued October 2003) - i - Water Research Laboratory School of Civil and Environmental Engineering Technical Report No 2002/20 University of New South Wales ABN 57 195 873 179 Report Status Final King Street Date of Issue October 2003 Manly Vale NSW 2093 Australia Telephone: +61 (2) 9949 4488 WRL Project No. 00758 Facsimile: +61 (2) 9949 4188 Project Manager B M Miller Title BROOKLYN ESTUARY PROCESS STUDY Editor(s) B M Miller, D Van Senden Client Name Hornsby Shire Council Client Address PO Box 37 296 Pacific Highway HORNSBY NSW 1630 Client Contact Jacqui Grove Client Reference Major Involvement by: Brett Miller (WRL), David van Senden (MHL), William Glamore (WRL), Ainslie Fraser (WRL), Matt Chadwick (WRL), Peggy O'Donnell (TEL), Michele Widdowson (MHL), Bronson McPherson (MHL), Sophie Diller (TEL), Charmaine Bennett (TEL), John Hudson (CMG), Theresa Lasiak (CEICC) and Tony Underwood (CEICC). The work reported herein was carried out at the Water Research Laboratory, School of Civil and Environmental Engineering, University of New South Wales, acting on behalf of the client. -

Act Three: Scene One the View from Above
Act Three: The View from Above Scene One The DMR observer in the helicopter was Hal Gregge. He describes what it was like looking down from above: “Anything on a main road is our responsibility, so with a thing like the ferries, the buck stops with us. The helicopter pilot was called Noel and the fellow we were reporting to was Bill McIntyre who was running the workshop at Granville. That was our central workshop - we had all trades and 400 people working there then. We used to support all the ferries from there - they had riggers and people like that and we’d overhaul the ferry engines there. We used to have the patterns to cast the spider wheels, even. It’s all closed down now, though. Bill was organising ground support. He’s retired now. “By the time the helicopter got up to Wisemans, we found noth- ing there. Noel is a very good pilot. He did his training all over the world and has been under fire and everything, so we were able to fly quite low at times when we needed to. We zoomed in around Webbs Creek. There was a set of piers there that they normally tie the ferry to, but of course they were empty. We went around the corner to the piles for the other two ferries, but they’d gone, too. So we just followed the river down at a reasonable height. It wasn’t a bad day on the Tuesday - the flood was well up, but the cloud and rain were gone. -
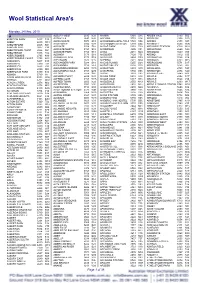
Wool Statistical Area's
Wool Statistical Area's Monday, 24 May, 2010 A ALBURY WEST 2640 N28 ANAMA 5464 S15 ARDEN VALE 5433 S05 ABBETON PARK 5417 S15 ALDAVILLA 2440 N42 ANCONA 3715 V14 ARDGLEN 2338 N20 ABBEY 6280 W18 ALDERSGATE 5070 S18 ANDAMOOKA OPALFIELDS5722 S04 ARDING 2358 N03 ABBOTSFORD 2046 N21 ALDERSYDE 6306 W11 ANDAMOOKA STATION 5720 S04 ARDINGLY 6630 W06 ABBOTSFORD 3067 V30 ALDGATE 5154 S18 ANDAS PARK 5353 S19 ARDJORIE STATION 6728 W01 ABBOTSFORD POINT 2046 N21 ALDGATE NORTH 5154 S18 ANDERSON 3995 V31 ARDLETHAN 2665 N29 ABBOTSHAM 7315 T02 ALDGATE PARK 5154 S18 ANDO 2631 N24 ARDMONA 3629 V09 ABERCROMBIE 2795 N19 ALDINGA 5173 S18 ANDOVER 7120 T05 ARDNO 3312 V20 ABERCROMBIE CAVES 2795 N19 ALDINGA BEACH 5173 S18 ANDREWS 5454 S09 ARDONACHIE 3286 V24 ABERDEEN 5417 S15 ALECTOWN 2870 N15 ANEMBO 2621 N24 ARDROSS 6153 W15 ABERDEEN 7310 T02 ALEXANDER PARK 5039 S18 ANGAS PLAINS 5255 S20 ARDROSSAN 5571 S17 ABERFELDY 3825 V33 ALEXANDRA 3714 V14 ANGAS VALLEY 5238 S25 AREEGRA 3480 V02 ABERFOYLE 2350 N03 ALEXANDRA BRIDGE 6288 W18 ANGASTON 5353 S19 ARGALONG 2720 N27 ABERFOYLE PARK 5159 S18 ALEXANDRA HILLS 4161 Q30 ANGEPENA 5732 S05 ARGENTON 2284 N20 ABINGA 5710 18 ALFORD 5554 S16 ANGIP 3393 V02 ARGENTS HILL 2449 N01 ABROLHOS ISLANDS 6532 W06 ALFORDS POINT 2234 N21 ANGLE PARK 5010 S18 ARGYLE 2852 N17 ABYDOS 6721 W02 ALFRED COVE 6154 W15 ANGLE VALE 5117 S18 ARGYLE 3523 V15 ACACIA CREEK 2476 N02 ALFRED TOWN 2650 N29 ANGLEDALE 2550 N43 ARGYLE 6239 W17 ACACIA PLATEAU 2476 N02 ALFREDTON 3350 V26 ANGLEDOOL 2832 N12 ARGYLE DOWNS STATION6743 W01 ACACIA RIDGE 4110 Q30 ALGEBUCKINA -

Redevelopment of Peat Island and Surrounding Land: Community Meetings Planned Feb 4Th & 25Th
Newsletter of the Brooklyn Community Association, Inc January 2012 Redevelopment of Peat Island and Surrounding Land: Community Meetings Planned Feb 4th & 25th Map of Potential Land Uses from the State Property Authority’s newsletter to the community, February 2011 Two meetings will be held to discuss this important topic. The Brooklyn Community Associa- tion meeting is Saturday, February 4th, 10am to noon, at the Brooklyn Meeting Room. All Brooklyn residents are invited. The purpose is to develop a Brooklyn perspective on the pro- ject for presentation at the next meeting. The second meeting on Saturday, February 25th, 10am to noon is with Matt Kean, MP Hornsby, Barry Douse, General Manager and Simon Furness, Executive Director of the State Property Authority, to listen to our views on the Peat Island and Mooney Redevelopment and how this will affect facilities and infrastructure in Brooklyn. Please consider coming to both. 1 Peat Island Redevelopment: Excerpts of a Letter Sent to Matt Kean, MP Hornsby, 10.07.2011, from the Brooklyn Community Association “On a whole the community is excited by the prospect of a sensitively, well thought out redevelopment of the Peat Island site and the sur- The BCA would like to see genuine community consultation with the rounding areas of Mooney Mooney (hereafter known as Peat island Brooklyn community and also the inclusion of Hornsby Shire Council Redevelopment). The BCA welcomes more residents in our rive com- into this important planning process. munity. Land buffer - required around the oyster industry at the end of The NSW Liberal Government has been a long time espouser of new Kowan Rd in Mooney. -

Hawkesbury Estuary Program 2014 Annual Report
Hawkesbury Estuary Program 2014 Annual Report HORNSBY SHIRE COUNCIL Hawkesbury Estuary Program 2013 - 2014 Annual Report Acknowledgements The Hawkesbury Estuary Program 2013-2014 Annual Report was produced by Dr Ana Rubio and Dr Peter Coad. Assistance with programs and report contributions were provided by staff from Council’s Natural Resources Branch, Planning Division and Infrastructure and Recreation Division. For further information contact: Dr Peter Coad Natural Resources Strategy Manager Environment and Human Services Division Hornsby Shire Council Tel: 02 9847 6766 Fax: 02 9847 6598 Email: [email protected] Web: www.hornsby.nsw.gov.au/estuary Table of Contents TABLE OF CONTENTS ........................................................................................................................................ III TABLE OF FIGURES ........................................................................................................................................... IV EXECUTIVE SUMMARY ...................................................................................................................................... 1 1 HAWKESBURY ESTUARY PROGRAM ..................................................................................................... 4 1.1 APPROACH .................................................................................................................................................... 4 1.2 GOALS ........................................................................................................................................................ -

Hawkesbury River Oyster Shed Pete O’Sullivan Has Owned Oyster Leases on the Hawkesbury River Since 2006, Growing Two Types of Oysters, Sydney Rock and Pacific Oysters
Newsletter of the Brooklyn Community Association Inc May 2018 President’s Report (Next Issue August 2018) Not only do we live in the lucky country, we live in a wonderful community. Did you know that over a quarter of Australians live alone which can result in isolation and increased mental health issues? Here in Brooklyn we have so many opportunities for young and old to get involved, make friends and stay connected. This edition of the Gateway explores the many activities that are happening in our community. We are excited to let you know about new volunteer opportunities - the Brooklyn Community Association now has two new subcommittees. One is the oral history project. We plan to record the stories of the wonderful, interesting people that have made Brooklyn what it is today. We want to ensure that these stories are saved and shared. Our sustainability subcommittee has already met to discuss recycling, and we are looking into renewable energy options for the community. To see the exciting work other communities are doing go to http://www.abc.net.au/news/2018-04-07/people-power:-communities-funding-their-own-wind/9630150. If you are interested in either subcommittee, send an email to [email protected], indicate your subject of interest and we will contact you with more information. Since our last meeting, the committee has been working to ensure the Independent Hearing and Assessment Panel selection process is fair and transparent and we have attended Council meetings to express our views. We will update you at the next meeting. -

Title Planning Proposal 58/2014 Various Lots Mooney
Gov Report Page 1 TITLE PLANNING PROPOSAL 58/2014 VARIOUS LOTS MOONEY MOONEY INCLUDING PEAT ISLAND ZONING OF SURPLUS GOVERNMENT LAND TO FACILITATE ITS DEVELOPMENT FOR A MIX OF RESIDENTIAL, COMMUNITY, RECREATION AND EMPLOYMENT LAND USES. APPLICANT URBIS (IR 18143393) Department: Governance & Planning Service Unit: Sustainable Corporate & City Planning The following item is defined as a planning matter pursuant to the Local Government Act, 1993 & Environmental Planning & Assessment Act, 1979 Disclosure of political donations and gifts - s147 Environmental Planning and Assessment Act (EP&A Act). “A relevant planning application means: (a) a formal request to the Minister, a council or the Director-General to initiate the making of an environmental planning instrument or development control plan in relation to development on a particular site”, i.e. a Planning Proposal. The object of Section 147 is to require the disclosure by a person of relevant political donations or gifts when a relevant planning application is made to Council per s147(4). No disclosure was made by the applicant. Council is initiating the subject Planning Proposal, therefore it is not a ‘relevant planning application’ that requires disclosure per Section 147(4). EXECUTIVE SUMMARY A Planning Proposal has been lodged for 18 properties (Lot 2 DP239249, Lot 10 DP1157280, Lot 11 DP1157280, Lot 4 DP239249, Lot 11 DP863305, Lot 9 DP863305, Lot 7011 DP1057994, Lot 2 DP431999, Lot 12 DP863305,Lot1 DP 597504, Lot 2 DP945014, Lot 1 DP431780, Lot 21 DP836628, Lot 1 DP945014, Lot 1 DP107391, Lot 12 DP1158746, Lot 13 DP1158746, Lot 14 DP1158746) owned by the NSW Government at Mooney Mooney (includes Peat Island) to rezone the land to permit for a mix of residential, community, recreation and employment land uses identified in the Indicative Concept Plan (tabled for Council's information) prepared by the applicant. -

Brooklyn Community Association General Meeting
Newsletter of the Brooklyn Community Association Inc February 2018 (Next Issue May 2018) President’s Report We are looking forward to a great year at the BCA and in our community. We have some new members on the committee, Ingrid Segovia, who is heading up our environment and sustainability subcommittee, Jayne Donnelly who has revamped our website and will be getting us onto a much better looking and efficient mailing program and Brian Scarsbrick. Now that Brian is newly retired he can join us on the committee along with representing Ward A for the Independent Hearing and Assessment Panel (IHAP). It is great news that someone with Brian’s background will be helping to review planning in our Council. After the input from Liz Surrest at our last meeting regarding the burnouts on Pacific Highway and how dangerous the road is, the BCA took up the issue with the Advocate and Matt Kean’s office. Some of you might have read the grim statistics of the stretch of road from Brooklyn to Cowan. In the last five years, there have been 96 accidents with 44 serious injuries and 5 fatalities! Imagine if we added the accidents that happened on the M1 on that same stretch - it might be one of the most dangerous areas for accidents! Both the Brooklyn Masterplan and Peat Island are in holding patterns. We were told that the Councillors would be getting briefed on the Masterplan as we go to press and our Ward Councillors and Mayor are still supporting the Masterplan. Nathan Tilbury will be at the meeting to provide a briefing. -

Brooklyn Community Association General Meeting
Newsletter of the Brooklyn Community Association Inc February 2019 (Next Issue June 2019) President’s Report We hope you can join us for our first meeting for 2019. We have changed the time of our meetings to 3pm to make it easier for families with children in Saturday morning sport to get involved and attend the BCA meetings. We have many items to discuss and would like your input. The BCA committee met with Hornsby Council late last year regarding the Masterplan. Council have decided to conclude the Brooklyn Improvement Masterplan process and are now going forward with their new “placemaking” approach with a focus on achievable improvements using early work completed by the consultants. Even before the official statement, the BCA began work with the Council to activate the Hawkesbury River Arts Cottage for our community. We see the cottage as an important space for connection, creation and discussion. We have had a couple of meetings with Council officers to discuss the renovation and use of the cottage, and we will review the formal proposal we made to the Council at the meeting. NSW State Property arranged a walk around Peat Island on the 10th of February. The zoning plans are now with the Central Coast Council and following zoning approval, will be put up for community consultation. Whilst there have been great improvements to the first plan, we are still concerned that there are plans for 268 dwellings which will put a demand on current infrastructure. And unfortunately, there is not a current study on the cumulated effects on the surrounding communities across the river. -

Technical Report 2003/01 March 2003 D R Cox, W L Peirson and J L
HAWKESBURY NEPEAN ESTUARY SALINE DYNAMICS MODEL CALIBRATION by D R Cox, W L Peirson and J L Davies Technical Report 2003/01 March 2003 THE UNIVERSITY OF NEW SOUTH WALES SCHOOL OF CIVIL AND ENVIRONMENTAL ENGINEERING WATER RESEARCH LABORATORY HAWKESBURY NEPEAN ESTUARY SALINE DYNAMICS MODEL CALIBRATION WRL Technical Report 2003/01 March 2003 by D R Cox, W L Peirson and J L Davies https://doi.org/10.4225/53/58d4a604e8ea6 Water Research Laboratory School of Civil and Environmental Engineering Technical Report No 2003/01 University of New South Wales ABN 57 195 873 179 Report Status Final King Street Date of Issue March 2003 Manly Vale NSW 2093 Australia Telephone: +61 (2) 9949 4488 WRL Project No. 02107 Facsimile: +61 (2) 9949 4188 Project Manager D R Cox Title Hawkesbury Nepean River Saline Dynamics – Model Calibration Author(s) D R Cox, W L Peirson and J L Davies Client Name Hawkesbury Nepean River Management Forum Client Address PO Box 556, Windsor NSW 2756 Client Contact Brian Walters Client Reference The work reported herein was carried out at the Water Research Laboratory, School of Civil and Environmental Engineering, University of New South Wales, acting on behalf of the client. Information published in this report is available for general release only with permission of the Director, Water Research Laboratory, and the client. WRL TECHNICAL REPORT 2003/01 CONTENTS 1. INTRODUCTION 1 2. BACKGROUND 2 2.1 Environmental Flows 2 2.2 The Hawkesbury Nepean River 2 2.2.1 General Characteristics 2 2.2.2 Modifications to the Natural Flow Regime 3 3. -

Brooklyn-Waterway Planning Study
I I BROOKLYN I Waterway Planning Study I I I I I I I I I I I I I I I I NOVEMBER,1988 Public Works Department, N.S.W. Hornsby Shire Council I I I Public Works Department N.S. W. Hornsby Shire Council I I I I I BROOKLYN I W ATERWA Y PLANNING STUDY I I I NOVEMBER 1988 I I I MN. CLARKE Chief Engineer - Public Works Department I R.K. WOODWARD Shire Clerk - Hornsby Shire Council I I I Report No. 88057 ISBN 0730551490 I I I I I FOREWORD The Hawkesbury RIver is an mcreasmgly lITIportant recreational amenity for the Sydney I Metropohtan area and Brooklyn IS one of the few gateways to the Hawkesbury DespIte Brooklyn's close proxirruty to Sydney and the availability of road and rail transport a number of problems have restricted the development potentIal of the Brooklyn area for tOUrIsm I and water based recreatlOn These problems mclude siltatlOn of naVlgatlOn channels, poor public access to foreshores and congestlOn and confuct amongst the waterway and foreshore users I The waterways and foreshore of the Brooklyn area are located wIthin the Hornsby Shire Council, and planning strategies for the reglon between Asquith and Brooklyn are currently under reVIew by the Council. The Public Works Department was requested by Council to assIst m preparing a I planning framework for the Brooklyn waterway This report documents the findings of the "Brooklyn Waterway Plannmg Study" It identifies present actIVItIes, future waterway and land requrrements, factors affecting development and I presents an overall plan wruch the Council could adopt as an approprIate strategy for the future development of Brooklyn The report has been prepared as part of the NSW Waterways Program and jointly funded by the I Public Works Department and Hornsby Shrre Council on a 3.1 basis The assistance of the varIOUS mdivlduals and government authOrItIes lS gratefully acknowledged. -

Hawkesbury River, Pittwater & Sydney by Superyacht
because life's too short for average holidays because life's too short for average holidays Southern KimberleyEXCLUSIVE by Superyacht CRUISE ONLY INCLUSIONS: Stateroom Type AUD Price PP From - One way light plane transfer from Broome to Cygnet Bay to join your yacht Twin Stateroom $12,020 - 6 night YOTSPACE superyacht voyage aboard the Phoenix One from Cygnet Bay to Prince Frederick Harbour 7 King Stateroom $12,020 - All meals onboard prepared by your gourmet chef to a five star standard - All onboard beverages including highHawkesbury quality Australian wines, sparkling, River, Pittwater6 & SydneyVIP King Stateroom by Superyacht$18,797 beers, basic spirits and cocktails - All off ship included excursions and expeditions (excluding helicopter nights Master King Stateroom $18,797 rides/scenic flights) EXCLUSIVEDays Superyacht - All port and government chargesCRUISE ONLY INCLUSIONS: Date Port Stateroom Type ArriveAUD Price PPDepart From - Service of your captain and onboard- 6 night YOTSPACE crew including superyacht chef voyage aboard the Corroboree round trip Double Stateroom $7,179 - Daily service of your cabin from Sydney 2022 nightsCruise Itinerary - One way Mallard Float plane- transferLuxury ensuite from accommodation Prince Frederick with individualHarbour air to conditioning controls 7 VIP Queen Stateroom $10,289 - All meals onboard prepared by your gourmet chef to a five star standard13/06 Broome, W A Flight to Darwin 6 Master King Stateroom - All onboard beverages including high quality Australian wines, sparkling, Cygnet$12,921 Bay - EXCLUSIVE Bonus offer - Bookbeers, this basic departure spirits and date cocktails by 31 July 2021 and receive complimentary port to -airport All off ship transfers included in excursions Darwin andby privateexpeditions car! including where possible:13/06 A Cygnet Bay,Bonus WA Australiaport transfers within 40kmEmbark radius! 2 hour visit to Broken Bay Pearl Farm, Island visits, guided walks etc.