Study of Methyl Dopa Versus Labetalol in Management of Preeclampsia and Gestational Hypertension
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Adrenergic Antagonist
PHARMACOLOGY Adrenergic antagonist OBJECTIVES: • Describe the different classifications for drugs that can block sympathetic nervous system. •Describe the kinetics, dynamics, uses and side effects of alpha adrenergic drugs. • Identify Difference between selective and non selective alpha blockers. • Know the difference between tamsulosin and other selective alpha receptor blockers. •Identify the different classifications for beta receptors blockers. •Describe the kinetics, dynamics, uses and side effects of beta adrenergic drugs. •Know the preferable drug for diseases as hypertension, glaucoma, arrythmia, myocardial infarction, anxiety, migraine and ect…. • Important. • Extra notes It’s a recall, if you know it you can skip it! Adrenergic receptors Adrenergic receptors Dopaminergic adrenoceptors adrenoceptors α− β− receptors β3 α1 α2 β1 β2 e.g. D1 α1 β2 β1 β3 Post-synaptic excitatory in function (cause inhibitory in function excitatory in In adipose contraction) except in GIT. (cause relaxation) function, present tissue mainly in heart Present mainly in smooth muscles. Contraction of pregnant Relaxation of the uterus ↑ heart rate: ↑ lipolysis uterus. (Delay premature labor) + chronotropic ↑ free fatty effect, Vasoconstriction of skin & Relaxation of skeletal & acids. Tachycardia peripheral blood vessels coronary blood vessels →increased peripheral (vasodilatation) ↑ force of → resistance hypertension. contraction : Relaxation of GIT muscles & urinary bladder’s muscles. + inotropic effect Contraction of GIT sphincter (constipation) & urinary -
Guanfacine Extended Release for ADHD
Out of the Pipeline p Guanfacine extended release for ADHD Floyd R. Sallee, MD, PhD uanfacine extended release (GXR)— Table 1 α Once-daily a selective -2 adrenergic agonist Guanfacine extended release: GFDA-approved for the treatment formulation may of attention-defi cit/hyperactivity disor- Fast facts improve adherence der (ADHD)—has demonstrated effi cacy Brand name: Intuniv and control for inattentive and hyperactive/impulsive Indication: Attention-defi cit/hyperactivity symptoms across disorder symptom domains in 2 large trials lasting® Dowden Health Media a full day 8 and 9 weeks.1,2 GXR’s once-daily formu- Approval date: September 3, 2009 lation may increase adherence and deliver Availability date: November 2009 consistent control of symptomsCopyright across a For personalManufacturer: use Shire only full day (Table 1). Dosing forms: 1-mg, 2-mg, 3-mg, and 4-mg extended-release tablets Recommended dosage: 0.05 to 0.12 mg/kg Clinical implications once daily GXR exhibits enhancement of noradren- ergic pathways through selective direct receptor action in the prefrontal cortex.3 brain believed to play a major role in at- This mechanism of action is different from tentional and organizational functions that that of other FDA-approved ADHD medi- preclinical research has linked to ADHD.3 cations. GXR can be used alone or in com- The postsynaptic α-2A receptor is bination with stimulants or atomoxetine thought to play a central role in the opti- for treating complex ADHD, such as cases mal functioning of the PFC as illustrated accompanied by oppositional features and by the “inverted U hypothesis of PFC ac- emotional dysregulation or characterized tivation.”4 In this model, cyclic adenos- by partial stimulant response. -

The Adrenergic Control of Lower Esophageal Sphincter Function: an EXPERIMENTAL MODEL of DENERVATION SUPERSENSITIVITY
The Adrenergic Control of Lower Esophageal Sphincter Function: AN EXPERIMENTAL MODEL OF DENERVATION SUPERSENSITIVITY Anthony J. DiMarino, Sidney Cohen J Clin Invest. 1973;52(9):2264-2271. https://doi.org/10.1172/JCI107413. To evaluate the adrenergic regulation of lower esophageal sphincter (LES) function, LES pressure, LES relaxation during swallowing, and blood pressure were measured in the anesthetized opossum, Didelphis virginiana, during intravenous administration of alpha and beta adrenergic agonists and antagonists. Studies were done in controls and animals adrenergically denervated with 6-hydroxydopamine. Alpha adrenergic agonists (norepinephrine, phenylephrine) increased LES pressure and blood pressure, whereas a beta adrenergic agonist (isoproterenol) decreased both pressures. Alpha adrenergic antagonism (phentolamine) reduced basal LES pressure by 38.3±3.8% (mean ±SEM) (P < 0.001). Beta adrenergic antagonism (propranolol) had no significant effect on either basal LES pressure or percent of LES relaxation with swallowing. After adrenergic denervation with 6-hydroxydopamine, basal LES pressure was reduced by 22.5±5.3% (P < 0.025) but LES relaxation during swallowing was unaltered. In denervated animals, both LES pressure and blood pressure dose response curves showed characteristics of denervation supersensitivity to alpha but not to beta adrenergic agonists. These studies suggest: (a) a significant portion of basal LES pressure is dependent upon alpha adrenergic stimulation; (b) LES relaxation during swallowing is not an adrenergically mediated response; c( ) the LES pressure response to alpha adrenergic agonists after 6-hydroxydopamine may serve as a model of denervation supersensitivity in the gastrointestinal tract. Find the latest version: https://jci.me/107413/pdf The Adrenergic Control of Lower Esophageal Sphincter Function AN EXPERIMENTAL MODEL OF DENERVATION SUPERSENSITIVITY ANTHoNY J. -

TRANDATE® (Labetalol Hydrochloride) Tablets
NDA 18716/S-026 Page 2 PRODUCT INFORMATION TRANDATE® (labetalol hydrochloride) Tablets DESCRIPTION: Trandate Tablets are adrenergic receptor blocking agents that have both selective alpha1-adrenergic and nonselective beta-adrenergic receptor blocking actions in a single substance. Labetalol hydrochloride (HCl) is a racemate chemically designated as 2-hydroxy-5-[1-hydroxy-2-[(1 methyl-3-phenylpropyl)amino]ethyl]benzamide monohydrochloride, and it has the following structure: Labetalol HCl has the empirical formula C19H24N2O3•HCl and a molecular weight of 364.9. It has two asymmetric centers and therefore exists as a molecular complex of two diastereoisomeric pairs. Dilevalol, the R,R′ stereoisomer, makes up 25% of racemic labetalol. Labetalol HCl is a white or off-white crystalline powder, soluble in water. Trandate Tablets contain 100, 200, or 300 mg of labetalol HCl and are taken orally. The tablets also contain the inactive ingredients corn starch, FD&C Yellow No. 6 (100- and 300-mg tablets only), hydroxypropyl methylcellulose, lactose, magnesium stearate, pregelatinized corn starch, sodium benzoate (200-mg tablet only), talc (100-mg tablet only), and titanium dioxide. CLINICAL PHARMACOLOGY: Labetalol HCl combines both selective, competitive, alpha1-adrenergic blocking and nonselective, competitive, beta-adrenergic blocking activity in a single substance. In man, the ratios of alpha- to beta-blockade have been estimated to be approximately 1:3 and 1:7 following oral and intravenous (IV) administration, respectively. Beta2-agonist activity has been demonstrated in animals with minimal beta1-agonist (ISA) activity detected. In animals, at doses greater than those required for alpha- or beta-adrenergic blockade, a membrane stabilizing effect has been demonstrated. -

Pain Management Opioid Safety a Quick Reference Guide (2014)
Pain Management Opioid Safety A Quick Reference Guide (2014) VA Academic Detailing Service Real Provider Resources Real Patient Results Your Partner in Enhancing Veteran Health Outcomes VA Academic Detailing Service Email Group: [email protected] VA Academic Detailing Service SharePoint Site: https://vaww.portal2.va.gov/sites/ad Opioids: A Practical Guide for Clinicians Example Risk Assessment Tool: Opioid Risk Tool (ORT)1 Item Score if Female Item Score if Male Alcohol 1 3 1. Family history of substance abuse Illegal drugs 2 3 Prescription drugs 4 4 Alcohol 3 3 2. Personal history of substance abuse Illegal drugs 4 4 Prescription drugs 5 5 3. Age (mark box if 16–45) 1 1 4. History of preadolescent sexual abuse 3 0 Attention deficit disorder obsessive compulsive disorder 2 2 5. Psychological disease Bipolar Schizophrenia Depression 1 1 Total Risk Category: 0–3 Low Risk of aberrant behaviors; 4–7 Moderate Risk of aberrant behaviors; ≥8 High Risk of aberrant behaviors Assess risk of aberrant behaviors before initiating opioid medications; the ORT or other rating tools can assist with this process but can overestimate risk thus should not be used as only reason to decline opioid prescription. 1 Opioids Risk Classification10-11 Risk Condition/Situation • Diagnosis with concordant physical exam, medical imaging, laboratory findings • High levels of pain acceptance and active coping strategies Low • Well motivated patient willing to participate in multimodal treatment plan (no moderate to high risk • Attempting to function -
New Zealand Data Sheet 1. Product Name
NEW ZEALAND DATA SHEET 1. PRODUCT NAME Norvir 100 mg tablets. 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each film-coated tablet contains 100 mg ritonavir. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM White film-coated oval tablets debossed with the corporate Abbott "A" logo and the Abbott-Code “NK”. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications NORVIR is indicated for use in combination with appropriate antiretroviral agents or as monotherapy if combination therapy is inappropriate, for the treatment of HIV-1 infection in adults and children aged 12 years and older. For persons with advanced HIV disease, the indication for ritonavir is based on the results for one study that showed a reduction in both mortality and AIDS defining clinical events for patients who received ritonavir. Median duration of follow-up in this study was 6 months. The clinical benefit from ritonavir for longer periods of treatment is unknown. For persons with less advanced disease, the indication is based on changes in surrogate markers in controlled trials of up to 16 weeks duration (see section 5.1 Pharmacodynamic properties). 4.2 Dose and method of administration General Dosing Guidelines Prescribers should consult the full product information and clinical study information of protease inhibitors if they are co-administered with a reduced dose of ritonavir. The recommended dose of NORVIR is 600 mg (six tablets) twice daily by mouth, and should be given with food. NORVIR tablets should be swallowed whole and not chewed, broken or crushed. NORVIR DS 29 April 2020 Page 1 of 37 Version 35 Paediatric population Ritonavir has not been studied in patients below the age of 12 years; hence the safety and efficacy of ritonavir in children below the age of 12 have not been established. -

The Importance of Serotonergic and Adrenergic Receptors for the Induction and Expression of One-Trial Cocaine-Induced Behavioral Sensitization" (2016)
California State University, San Bernardino CSUSB ScholarWorks Electronic Theses, Projects, and Dissertations Office of aduateGr Studies 12-2016 THE IMPORTANCE OF SEROTONERGIC AND ADRENERGIC RECEPTORS FOR THE INDUCTION AND EXPRESSION OF ONE- TRIAL COCAINE-INDUCED BEHAVIORAL SENSITIZATION Krista N. Rudberg California State University - San Bernardino Follow this and additional works at: https://scholarworks.lib.csusb.edu/etd Part of the Biological Psychology Commons, and the Pharmacology Commons Recommended Citation Rudberg, Krista N., "THE IMPORTANCE OF SEROTONERGIC AND ADRENERGIC RECEPTORS FOR THE INDUCTION AND EXPRESSION OF ONE-TRIAL COCAINE-INDUCED BEHAVIORAL SENSITIZATION" (2016). Electronic Theses, Projects, and Dissertations. 420. https://scholarworks.lib.csusb.edu/etd/420 This Thesis is brought to you for free and open access by the Office of aduateGr Studies at CSUSB ScholarWorks. It has been accepted for inclusion in Electronic Theses, Projects, and Dissertations by an authorized administrator of CSUSB ScholarWorks. For more information, please contact [email protected]. THE IMPORTANCE OF SEROTONERGIC AND ADRENERGIC RECEPTORS FOR THE INDUCTION AND EXPRESSION OF ONE-TRIAL COCAINE- INDUCED BEHAVIORAL SENSITIZATION A Thesis Presented to the Faculty of California State University, San Bernardino In Partial Fulfillment of the Requirements for the Degree Master of Arts in General/Experimental Psychology by Krista Nicole Rudberg December 2016 THE IMPORTANCE OF SEROTONERGIC AND ADRENERGIC RECEPTORS FOR THE INDUCTION AND EXPRESSION OF ONE-TRIAL COCAINE- INDUCED BEHAVIORAL SENSITIZATION A Thesis Presented to the Faculty of California State University, San Bernardino by Krista Nicole Rudberg December 2016 Approved by: Sanders McDougall, Committee Chair, Psychology Cynthia Crawford, Committee Member Matthew Riggs, Committee Member © 2016 Krista Nicole Rudberg ABSTRACT Addiction is a complex process in which behavioral sensitization may be an important component. -

Adrenoceptors Regulating Cholinergic Activity in the Guinea-Pig Ileum 1978) G.M
- + ! ,' Br. J. Pharmac. (1978), 64, 293-300. F'(O t.,," e reab- ,ellular PHARMACOLOGICAL CHARACTERIZATION OF THE PRESYNAPTIC _-ADRENOCEPTORS REGULATING CHOLINERGIC ACTIVITY IN THE GUINEA-PIG ILEUM 1978) G.M. Departmentof Pharmacology,Allen and HzmburysResearchLimited, Ware, Hertfordshire,SG12 ODJ I The presynaptic ct-adrenoceptors located on the terminals of the cholinergic nerves of the guinea- pig myenteric plexus have been characterized according to their sensitivities to at-adrenoceptor agonists and antagonists. 2 Electrical stimulation of the cholinergic nerves supplying the longitudinal muscle of the guinea-pig ! ileum caused a twitch response. Clonidine caused a concentration-dependent inhibition of the twitch i response; the maximum inhibition obtained was 80 to 95_o of the twitch response. Oxymetazoline and xylazine were qualitatively similar to clonidine but were about 5 times less potent. Phenylephrine and methoxamine also inhibited the twitch response but were at least 10,000 times less potent than clonidine. 3 The twitch-inhibitory effects of clonidine, oxymetazoline and xylazine, but not those of phenyl- ephrine or methoxamine, were reversed by piperoxan (0.3 to 1.0 lag/ml). 4 Lysergic acid diethylamide (LSD) inhibited the twitch response, but also increased the basal tone of the ileum. Mepyramine prevented the increase in tone but did not affect the inhibitory action of LSD. Piperoxan or phentolamine only partially antagonized the inhibitory effect of LSD. 5 Phentolamine, yohimbine, piperoxan and tolazoline were potent, competitive antagonists of the inhibitory effect of clonidine with pA2 values of 8.51, 7.78, 7.64 and 6.57 respectively. 6 Thymoxamine was a weak antagonist of clonidine; it also antagonized the twitch-inhibitory effect of morphine. -

Urine Drug Testing – Ordering and Interpretation The
URINE DRUG TESTING – ORDERING AND INTERPRETATION Created by: Dr. Daniel Berland, M.D. THE TESTS Enzyme linked immunoassay (EIA) kits • Screening test for illicit substances amphetamine/methamphetamine, (marijuana, PCP, cocaine, “opiates” (morphine/codeine) • Inexpensive, fast, point of care or lab • Detects class of substance, not specific medication • Will be negative for hydrocodone, hydromorphone, oxycodone, methadone, buprenorphine, benzodiazepines (particularly clonazepam) unless specific test kit for those meds is in use. Ask your lab! • High false positive rates caused by numerous prescribed or OTC meds Gas chromatography/Mass Spectroscopy (GCMS) • More expensive, labor intensive • Confirming test identifies specific meds and their metabolites. Use to confirm patient is taking prescribed meds and not taking non-prescribed meds • High sensitivity, but you must tell the lab what you seek (patient is taking) • False positives still occur ** Human Urine: T ~98 deg; > 90 deg for 15 min. pH 4.5-8; SG 1.002-1.03. Ur Cr > 20 mg/dL ** WHAT TO ORDER • Test for illicit drug use: EIA • Test to confirm taking prescribed meds: GCMS (EIA is OK if your lab runs the test for each med – they usually do not – ask!) • Test to check for use of non-prescribed medication: GCMS POSSIBLE OUTCOMES OF TESTING • Presence of illicit substance: Use by patient; false result related to prescribed or OTC med exposure • Presence of non-prescribed medication: Illicit use by patient; false positive testing – cross-reaction or possible known metabolite (e.g., morphine -

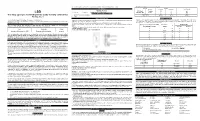
Management of Postnatal Hypertension - Top Tips
Management of postnatal hypertension - top tips FOLLOW UP PLAN Follow up Hypertensive disorder Chronic Gestational Pre - Severe pre- hypertension hypertension eclampsia eclampsia/ Mild/ HELLP/ Moderate Eclampsia Initial follow up Community midwife and general practitioner BP frequency At least once 3- At least once Every 1-2 days for 2 wks 5 days post 3-5 days post as above birth then as birth clinically Then as indicated clinically indicated Acceptable BP Aim BP should be <150/100 mmHg. BP <140/90 If not on antihypertensives commence if BP≥ 150/100 Suitable Labetalol, nifedipine, enalapril, atenolol, antihypertensives AVOID DIURETICS STOP METHYLDOPA WITHIN 2 DAYS OF DELIVERY When to reduce/ NA If BP<130/80 If BP<130/80 reduce stop If not seen reduce antihypertensive before needs If BP < 140/ If BP <140/ 90 consider GP review at 90 consider reducing 2wks post birth reducing Convert back to If not seen prepregnancy before needs antihypertensive GP review at as indicated 2wks post birth 6 weeks GP/ pre GP GP Hospital cons follow up pregnancy care clinic team POSTNATAL REVIEW AT POSTNATAL REVIEW 6-8 weeks after birth Offer medical review Offer specialist assessment if antihypertensives still needed Rpt Plt, transaminases, creatinine if indicated Carry out urine dipstick test If proteinuria still ≥ 1+ offer further review at 3 months to assess kidney function – consider offering renal referral. Give advice re: recurrence risks – see table below: Advise women to maintain BMI 18.5-24.9 kg/m2 H.Yeeles/S. Rutter July 14 Management of postnatal -
(LSD) Test Dip Card (Urine) • Specimen Collection Container % Agreement 98.8% 99
frozen and stored below -20°C. Frozen specimens should be thawed and mixed before testing. GC/MS. The following results were tabulated: Method GC/MS MATERIALS Total Results Results Positive Negative Materials Provided LSD Rapid Positive 79 1 80 LSD • Test device • Desiccants • Package insert • Urine cups Test Dip card Negative 1 99 100 Materials Required But Not Provided Total Results 80 100 180 One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) • Specimen collection container % Agreement 98.8% 99. % 98.9% • Timer Package Insert DIRECTIONS FOR USE Analytical Sensitivity This Instruction Sheet is for testing of Lysergic acid diethylamide. Allow the test device, and urine specimen to come to room temperature [15-30°C (59-86°F)] prior to testing. A drug-free urine pool was spiked with LSD at the following concentrations: 0 ng/mL, -50%cutoff, -25%cutoff, cutoff, A rapid, one step test for the qualitative detection of Lysergic acid diethylamide and its metabolites in human urine. 1) Remove the test device from the foil pouch. +25%cutoff and +50%cutoff. The result demonstrates >99% accuracy at 50% above and 50% below the cut-off For forensic use only. 2) Remove the cap from the test device. Label the device with patient or control identifications. concentration. The data are summarized below: INTENDED USE 3) Immerse the absorbent tip into the urine sample for 10-15 seconds. Urine sample should not touch the plastic Lysergic acid diethylamide (LSD) Percent of Visual Result The One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) is a lateral flow chromatographic device. -

F3-Adrenergic Antagonist (Receptors/Cyclic AMP/Aminobenzylpropranolol/Iodohydroxybenzylpindolol/Isoproterenol) WESLEY L
Proc. Natl. Acad. Sci. USA Vol. 76, No. 12, pp. 6401-6405, December 1979 Cell Biology Quantitative relationship between 3-adrenergic receptor number and physiologic responses as studied with a long-lasting f3-adrenergic antagonist (receptors/cyclic AMP/aminobenzylpropranolol/iodohydroxybenzylpindolol/isoproterenol) WESLEY L. TERASAKI, JOEL LINDEN, AND GARY BROOKER* Department of Pharmacology, School of Medicine, University of Virginia, Charlottesville, Virginia 22908 Communicated by Paul Greengard, August 20, 1979 ABSTRACT The aminobenzyl analog of propranolol, atrium when f3-adrenergic receptor number is selectively de- 1- (p-amino-a,a-dimethylphenethylamino)-3(1-naphthoxy)2- creased. To investigate this problem, a new propanol, was synthesized and found tobe a potent B-adrenergic f3-adrenergic blocking agent. The fl-adrenergic receptors of cultured rat C6 blocking agent, 1-(p-amino-a,a-dimethylphenethylamino- glioma cells (2B clone) as assessed by [' 51]iodohydroxybenzyl- 3-(1-naphthoxy)-2-propanol (aminobenzylpropranolol), was pindolol binding were decreased 50 and >95% afterpretreat- synthesized. It was found to be a selective agent for the elimi- ment with 8 nM and 1 ,M aminobenzylpropranolol, respec- nation of cellular /3-adrenergic receptors. tively. Unlike propranolol, aminobenzylpropranolol displayed a prolonged blockade of receptors that was maintained during several hours of washing. [121s]Iodohydroxybenzylpindolol MATERIALS AND METHODS saturation binding experiments in cells exposed to aminoben- Tissue Culture. C6 rat glioma cells, 2B subclone (7), were zylpropranolol and subsequently washed indicated that the compound effectively diminished receptor number with no grown in monolayer cultures as described (1) in 16-mm plastic change in the affinity of the remaining receptors for iodohy- cluster dishes. In all experiments, the cells were changed from droxybenzylpindolol.