The Frequency of Rhythm and Conduction Abnormalities and Benefits of 24-Hour Holter Electrocardiogram on Detecting These Abnormalities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Myocarditis and Cardiomyopathy
CE: Tripti; HCO/330310; Total nos of Pages: 6; HCO 330310 REVIEW CURRENT OPINION Myocarditis and cardiomyopathy Jonathan Buggey and Chantal A. ElAmm Purpose of review The aim of this study is to summarize the literature describing the pathogenesis, diagnosis and management of cardiomyopathy related to myocarditis. Recent findings Myocarditis has a variety of causes and a heterogeneous clinical presentation with potentially life- threatening complications. About one-third of patients will develop a dilated cardiomyopathy and the pathogenesis is a multiphase, mutlicompartment process that involves immune activation, including innate immune system triggered proinflammatory cytokines and autoantibodies. In recent years, diagnosis has been aided by advancements in cardiac MRI, and in particular T1 and T2 mapping sequences. In certain clinical situations, endomyocardial biopsy (EMB) should be performed, with consideration of left ventricular sampling, for an accurate diagnosis that may aid treatment and prognostication. Summary Although overall myocarditis accounts for a minority of cardiomyopathy and heart failure presentations, the clinical presentation is variable and the pathophysiology of myocardial damage is unique. Cardiac MRI has significantly improved diagnostic abilities, but endomyocardial biopsy remains the gold standard. However, current treatment strategies are still focused on routine heart failure pharmacotherapies and supportive care or cardiac transplantation/mechanical support for those with end-stage heart failure. Keywords cardiac MRI, cardiomyopathy, endomyocardial biopsy, myocarditis INTRODUCTION prevalence seen in children and young adults aged Myocarditis refers to inflammation of the myocar- 20–30 years [1]. dium and may be caused by infectious agents, systemic diseases, drugs and toxins, with viral infec- CAUSE tions remaining the most common cause in the developed countries [1]. -

Myocarditis, Pericarditis and Other Pericardial Diseases
Heart 2000;84:449–454 Diagnosis is easiest during epidemics of cox- GENERAL CARDIOLOGY sackie infections but diYcult in isolated cases. Heart: first published as 10.1136/heart.84.4.449 on 1 October 2000. Downloaded from These are not seen by cardiologists unless they develop arrhythmia, collapse or suVer chest Myocarditis, pericarditis and other pain, the majority being dealt with in the primary care system. pericardial diseases Acute onset of chest pain is usual and may mimic myocardial infarction or be associated 449 Celia M Oakley with pericarditis. Arrhythmias or conduction Imperial College School of Medicine, Hammersmith Hospital, disturbances may be life threatening despite London, UK only mild focal injury, whereas more wide- spread inflammation is necessary before car- diac dysfunction is suYcient to cause symp- his article discusses the diagnosis and toms. management of myocarditis and peri- Tcarditis (both acute and recurrent), as Investigations well as other pericardial diseases. The ECG may show sinus tachycardia, focal or generalised abnormality, ST segment eleva- tion, fascicular blocks or atrioventricular con- Myocarditis duction disturbances. Although the ECG abnormalities are non-specific, the ECG has Myocarditis is the term used to indicate acute the virtue of drawing attention to the heart and infective, toxic or autoimmune inflammation of leading to echocardiographic and other investi- the heart. Reversible toxic myocarditis occurs gations. Echocardiography may reveal segmen- in diphtheria and sometimes in infective endo- -

Postural Heart Block*
Br Heart J: first published as 10.1136/hrt.44.2.221 on 1 August 1980. Downloaded from Case reports Br Heart J 1980; 44: 221-3 Postural heart block* PETER E SEDA, JOHN H McANULTY, C JOE ANDERSON From the Department of Medicine, University of Oregon Health Sciences Center, Portland, Oregon, USA SUMMARY A patient presented with orthostatic dizziness and syncope caused by postural heart block. When the patient was supine, atrioventricular conduction was normal and he was asymptomatic; when he was standing he developed second degree type II block and symptoms. The left bundle-branch block on his electrocardiogram and intracardiac electrophysiological study findings suggest that this heart block occurred distal to the His bundle. Orthostatic symptoms are usually presumed to be secondary to an inappropriate distribution of intravascular volume or to autonomic nervous system abnormalities. As shown in this patient, these symptoms may be the result of orthostatic heart block. Ambulatory monitoring may be useful in patients with orthostatic neurological symptoms, particularly when conduction abnormalities are present on the electrocardiogram. Orthostatic neurological symptoms usually result minute and regular, and increased to 90 beats a from inadequate cerebral perfusion caused by minute with some irregularity when he was upright. disturbances of the autonomic nervous system,'-3 The carotid pulse was normal, and there were no ineffective or inappropriate shifts in volume carotid bruits. The cardiac impulse was normal. http://heart.bmj.com/ distribution,4 or drugs.5 We report a patient with The second heart sound was paradoxically split. orthostatic dizziness and syncope caused by inter- There was a grade 2/6 apical systolic murmur. -
Currentstateofknowledgeonaetiol
European Heart Journal (2013) 34, 2636–2648 ESC REPORT doi:10.1093/eurheartj/eht210 Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases Downloaded from Alida L. P. Caforio1†*, Sabine Pankuweit2†, Eloisa Arbustini3, Cristina Basso4, Juan Gimeno-Blanes5,StephanB.Felix6,MichaelFu7,TiinaHelio¨ 8, Stephane Heymans9, http://eurheartj.oxfordjournals.org/ Roland Jahns10,KarinKlingel11, Ales Linhart12, Bernhard Maisch2, William McKenna13, Jens Mogensen14, Yigal M. Pinto15,ArsenRistic16, Heinz-Peter Schultheiss17, Hubert Seggewiss18, Luigi Tavazzi19,GaetanoThiene4,AliYilmaz20, Philippe Charron21,andPerryM.Elliott13 1Division of Cardiology, Department of Cardiological Thoracic and Vascular Sciences, University of Padua, Padova, Italy; 2Universita¨tsklinikum Gießen und Marburg GmbH, Standort Marburg, Klinik fu¨r Kardiologie, Marburg, Germany; 3Academic Hospital IRCCS Foundation Policlinico, San Matteo, Pavia, Italy; 4Cardiovascular Pathology, Department of Cardiological Thoracic and Vascular Sciences, University of Padua, Padova, Italy; 5Servicio de Cardiologia, Hospital U. Virgen de Arrixaca Ctra. Murcia-Cartagena s/n, El Palmar, Spain; 6Medizinische Klinik B, University of Greifswald, Greifswald, Germany; 7Department of Medicine, Heart Failure Unit, Sahlgrenska Hospital, University of Go¨teborg, Go¨teborg, Sweden; 8Division of Cardiology, Helsinki University Central Hospital, Heart & Lung Centre, -

Neuropsychiatric Manifestations of Infective Endocarditis: a Study of 95 Patients at Ibadan, Nigeria
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.39.4.325 on 1 April 1976. Downloaded from Journal of Neurology, Neurosurgery, and Psychiatry, 1976, 39, 325-329 Neuropsychiatric manifestations of infective endocarditis: a study of 95 patients at Ibadan, Nigeria 0. BADEMOSI,1 A. 0. FALASE, F. JAIYESIMI, AND A. BADEMOSI From the Departments of Medicine and Paediatrics, University College Hospital, Ibadan, Nigeria SYNOPSIS Thirty-eight percent of patients with infective endocarditis (36 of 95) had neuropsychi- atric manifestations. In 750 (27 of 36), these features were the major presenting picture. Fifteen patients (42%) presented with cerebrovascular lesions and seven (19%) with meningitis. Toxic encephalopathy (12.5%) was not uncommon. Other neurological syndromes seen included psychosis and spinal cord lesions. The mortality was high especially when the infective endocarditis was acute in onset. It is essential to search diligently for an underlying cardiac cause in patients who present with neuropsychiatric symptoms because treatment of the underlying pathology improves prognosis. Although the clinical features of infective endo- criteria: (1) repeated positive blood cultures during a Protected by copyright. carditis are well established, significant changes febrile illness in a patient with known previous have taken place in the pattern of the disease in valvular or congenital heart disease; (2) evidence of the developed countries over the last 20 years peripheral manifestations of infective endocarditis; 1951; Pankey, (3) development of a significant cardiac murmur (Horder, 1909; Cates and Christie, with features of cardiac failure in any patient 1961, 1962; Thompson, 1964; Cooper et al., admitted for an unexplained febrile illness while 1966; British Medical Journal, 1973). -

Lyme Carditis and Sudden Cardiac Death
Health Update August 6, 2018 TO: Health Care Providers FROM: Mark Levine, MD, Commissioner of Health Lyme Carditis and Sudden CardiaC Death – Please Distribute as Appropriate – Laboratory results from the Centers for Disease Control and Prevention (CDC) have confirmed that the recent death of a Franklin County resident was a result of Lyme carditis, a rare complication of Lyme disease. This is the first reported death due to Lyme carditis in Vermont. Between 1985 and 2014 there were nine deaths related to Lyme carditis reported worldwide. The Health Department issued a Health Advisory on December 13, 2013 following a CDC report about sudden cardiac death associated with Lyme carditis. Symptomatic infection of the heart is rare in recognized Lyme disease cases. Approximately 1 percent of reported cases have Lyme carditis, which is usually present with other features of Lyme disease but can be observed independently. It is more common among males than would be expected based on the gender distribution of patients with clinical manifestations of Lyme disease. • Vermont Health Advisory: http://www.healthvermont.gov/dec2013_healthadvisory • CDC report: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6249a1.htm?s_cid=mm6249a1_w The most common cardiac manifestation is atrioventricular block (first, second, or third degree). Symptoms of atrioventricular block include lightheadedness, palpitations, shortness of breath, chest pain and syncope. Some cases might require temporary pacing, although prognosis is excellent with appropriate antibiotic therapy. Lyme disease is endemic in Vermont. Place carditis symptoms in context during the spring, summer and fall seasons. Actions Requested: • If you suspect Lyme disease, treat with antibiotics according to current treatment guidelines: https://www.cdc.gov/lyme/treatment/index.html • Ask all patients with suspected Lyme disease about cardiac symptoms. -

Answer: E) Atrial Fibrillation with Complete Heart Block Teaching Point
Answer: e) Atrial fibrillation with complete heart block Teaching Point: A slow regular ventricular rate in a patient with concurrent atrial fibrillation, as seen in this ECG, is diagnostic of complete heart block. Atrial fibrillation creates a diagnostic dilemma for identifying AV nodal disease or block. Close scrutiny should be placed on R-R intervals to identify patterns or regularity (1). Clinicians should be wary of a regular heart rate in a patient with persistent atrial fibrillation, especially in those using digitalis. If an AV nodal block is identified, it may be transient, and a search for reversible causes is indicated as in all cases of complete heart block prior to pacemaker placement. Electrolyte abnormalities, ischemia, and medications remain the leading reversible causes (2,3). The patient in this case was transferred to the Emergency Department and admitted for further observation. Ischemia was ruled out. Carvedilol was held, and he was diuresed. He continued to demonstrate adequate chronotropic response with exertion. The complete heart block soon resolved, and he was diuresed to euvolemia. Pacemaker placement was deferred given the transient nature of the AV block in the context of recent beta-blocker usage. He was discharged home with continuous heart rhythm monitoring without any further evidence of complete heart block. References: 1. Urbach JR, Grauman JJ, Straus SH. Quantitative Methods for the Recognition of Atrioventricular Junctional Rhythms in Atrial Fibrillation. Circulation. 1969; 39: 803- 817. 2. Kojic EM, Hardarson T, Sigfusson N, Sigvaldason H. The prevalence and prognosis of third-degree atrioventricular conduction block: the Reykjavik study. J Intern Med. -

Long QT Syndrome: an Emerging Role for Inflammation and Immunity
REVIEWS IN MEDICINE published: 27 May 2015 doi: 10.3389/fcvm.2015.00026 Long QT syndrome: an emerging role for inflammation and immunity Pietro Enea Lazzerini*, Pier Leopoldo Capecchi and Franco Laghi-Pasini Department of Medical Sciences, Surgery and Neurosciences, University of Siena, Siena, Italy The long QT syndrome (LQTS), classified as congenital or acquired, is a multi-factorial disorder of myocardial repolarization predisposing to life-threatening ventricular arrhyth- mias, particularly torsades de pointes. In the latest years, inflammation and immunity have been increasingly recognized as novel factors crucially involved in modulating ventricular repolarization. In the present paper, we critically review the available information on this topic, also analyzing putative mechanisms and potential interplays with the other etiologic factors, either acquired or inherited. Accumulating data indicate inflammatory activation as a potential cause of acquired LQTS. The putative underlying mechanisms are complex but essentially cytokine-mediated, including both direct actions on cardiomyocyte ion channels expression and function, and indirect effects resulting from an increased Edited by: central nervous system sympathetic drive on the heart. Autoimmunity represents another Theofilos M. Kolettis, recently arising cause of acquired LQTS. Indeed, increasing evidence demonstrates that University of Ioannina, Greece autoantibodies may affect myocardial electric properties by directly cross-reacting with Reviewed by: Luigi Venetucci, the cardiomyocyte and interfering with specific ion currents as a result of molecular University of Manchester, UK mimicry mechanisms. Intriguingly, recent data suggest that inflammation and immunity Giannis G. Baltogiannis, Cardiovascular Institute, Greece may be also involved in modulating the clinical expression of congenital forms of LQTS, *Correspondence: possibly triggering or enhancing electrical instability in patients who already are genetically Pietro Enea Lazzerini, predisposed to arrhythmias. -

Lyme Carditis Presenting As Atrial Fibrillation Treated Successfully - 08-11-2019 by Dr
Lyme carditis presenting as atrial fibrillation treated successfully - 08-11-2019 by Dr. Daniel Cameron - Daniel Cameron, MD, MPH - http://danielcameronmd.com Lyme carditis presenting as atrial fibrillation treated successfully Sunday, August 11, 2019 http://danielcameronmd.com/lyme-carditis-atrial-fibrillation-treated-successfully/ A case study published in the British Medical Journal features a 23-year-old man with a history of degenerative joint disease who presented with a sudden onset of palpitations. [2] His echocardiogram (ECG) revealed atrial fibrillation (AF) with a mildly dilated left Atrium. The patient did not recall a tick bite or a rash. And, “Although Lyme carditis was on the differential diagnoses list, it was not considered high enough due to the initial rhythm being AF and not [atrioventricular ] AV block,” writes Shabbir and colleagues. The man was treated with metoprolol and released from the hospital after his heart spontaneously reverted back to normal sinus rhythm. However, 4 days later the patient returned to the hospital. “ECG now exhibited atrioventricular (AV) mobitz-II block alternating with intermittent complete heart block (CHB) on telemetry confirmed with ECG,” writes Shabbir. He was tested for Lyme disease and treated empirically with intravenous ceftriaxone. Within 48 hours, his symptoms began to improve. Lyme disease tests came back positive. And 1 month later, after antibiotic therapy, his heart rhythm had returned to normal. The authors' key learning points include: 1. Consider the unusual initial presentation of Lyme disease as atrial fibrillation. 2. Keeping Lyme carditis in the differential diagnoses when someone from a Lyme-endemic area presents as supraventricular arrhythmia (atrial fibrillation/flutter). -

Cardiac Pacing in Incomplete Atrioventricular Block with Atrial Fibrillation
Br Heart J: first published as 10.1136/hrt.35.11.1154 on 1 November 1973. Downloaded from British Heart journal, I973, 35, I154-1I60. Cardiac pacing in incomplete atrioventricular block with atrial fibrillation D. S. Reid, S. J. Jachuck, and C. B. Henderson From the Department of Cardiology, Newcastle General Hospital, Newcastle upon Tyne Three cases with a slow irregular ventricular response to atrialfibrillation, who benefitedfrom cardiac pacing, are described; two had ischaemic heart disease, and one had cardiomyopathy. In thefirst case the slow ventricu- lar response to atrialfibrillation was a result of incomplete atrioventricular nodal block, and in the other two His bundle electrograms demonstrated that the slow ventricular response was due to bilateral bundle-branch block. The association of atrial fibrillation and conduction delays in the atrioventricular node and bundle- branches is discussed. The value of His bundle recordings in the investigation of these cases is shown and the importance of cardiac pacing in treatment is stressed. Cardiac pacing is now a generally accepted method hypotension. Intravenous atropine given before transfer of treatment in patients with complete heart block or had resulted in a paroxysm of ventricular tachycardia. bilateral bundle-branch block who have Adam- On admission there was no evidence of cardiac failure Stokes attacks or a low output to and the blood pressure was I05/50 mmHg. An electro- syndrome leading cardiogram showed atrial fibrillation with an irregular angina or cardiac failure. cardiac is However, pacing ventricular response of 40 to 44 beats a minute and acute now also becoming more widely used in the treat- inferolateral myocardial infarction (Fig. -
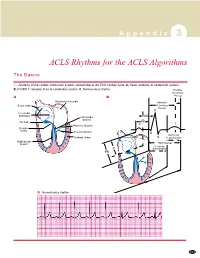
ACLS Rhythms for the ACLS Algorithms
A p p e n d i x 3 ACLS Rhythms for the ACLS Algorithms The Basics 1. Anatomy of the cardiac conduction system: relationship to the ECG cardiac cycle. A, Heart: anatomy of conduction system. B, P-QRS-T complex: lines to conduction system. C, Normal sinus rhythm. Relative Refractory A B Period Bachmann’s bundle Absolute Sinus node Refractory Period R Internodal pathways Left bundle AVN branch AV node PR T Posterior division P Bundle of His Anterior division Q Ventricular Purkinje fibers S Repolarization Right bundle branch QT Interval Ventricular P Depolarization PR C Normal sinus rhythm 253 A p p e n d i x 3 The Cardiac Arrest Rhythms 2. Ventricular Fibrillation/Pulseless Ventricular Tachycardia Pathophysiology ■ Ventricles consist of areas of normal myocardium alternating with areas of ischemic, injured, or infarcted myocardium, leading to chaotic pattern of ventricular depolarization Defining Criteria per ECG ■ Rate/QRS complex: unable to determine; no recognizable P, QRS, or T waves ■ Rhythm: indeterminate; pattern of sharp up (peak) and down (trough) deflections ■ Amplitude: measured from peak-to-trough; often used subjectively to describe VF as fine (peak-to- trough 2 to <5 mm), medium-moderate (5 to <10 mm), coarse (10 to <15 mm), very coarse (>15 mm) Clinical Manifestations ■ Pulse disappears with onset of VF ■ Collapse, unconsciousness ■ Agonal breaths ➔ apnea in <5 min ■ Onset of reversible death Common Etiologies ■ Acute coronary syndromes leading to ischemic areas of myocardium ■ Stable-to-unstable VT, untreated ■ PVCs with -

A Case of Long QT Syndrome
CASE REPORT A case of long QT syndrome: challenges on a bumpy road Peter Magnusson1,2 & Per-Erik Gustafsson2 1Cardiology Research Unit, Department of Medicine, Karolinska Institutet, Stockholm SE-171 76, Sweden 2Centre for Research and Development, Uppsala University/Region Gavleborg,€ Gavle€ SE-801 87, Sweden Correspondence Key Clinical Message Peter Magnusson, Cardiology Research Unit, Department of Medicine, Karolinska Beta-agonist treatment during pregnancy may unmask the diagnosis of long QT Institutet, Karolinska University Hospital/ syndrome. The QT prolongation can result in functional AV block. A history of Solna, SE-171 76 Stockholm, Sweden. Tel: seizure and/or sudden death in a family member should raise suspicion of ven- +46(0)705 089407; Fax: +46(0)26 154255; tricular tachycardia. More than one mutation may coexist. Refusal of beta- E-mail: [email protected] blocker therapy complicates risk stratification. Funding Information Keywords No sources of funding were declared for this Genetic, implantable cardioverter–defibrillator, long QT syndrome, pregnancy, study. premature ventricular complex, risk stratification, sudden cardiac death. Received: 16 December 2016; Revised: 29 March 2017; Accepted: 4 April 2017 Clinical Case Reports 2017; 5(6): 954–960 doi: 10.1002/ccr3.985 Introduction experienced palpitations, and her ECG was abnormal, revealing PVCs, atrioventricular (AV) 2:1 block and QT Long QT syndrome (LQTS) is linked to mutations in the prolongation (520 msec) in precordial lead V5 during ion channels, which can lead to disturbances in ventricu- sinus rhythm at 90 beats per minute (Fig. 1) and rhythm lar repolarization [1]. This condition puts patients at risk strip while walking (Fig.