Risk in the Optical Professions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
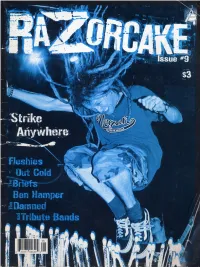
Razorcake Issue #09
PO Box 42129, Los Angeles, CA 90042 www.razorcake.com #9 know I’m supposed to be jaded. I’ve been hanging around girl found out that the show we’d booked in her town was in a punk rock for so long. I’ve seen so many shows. I’ve bar and she and her friends couldn’t get in, she set up a IIwatched so many bands and fads and zines and people second, all-ages show for us in her town. In fact, everywhere come and go. I’m now at that point in my life where a lot of I went, people were taking matters into their own hands. They kids at all-ages shows really are half my age. By all rights, were setting up independent bookstores and info shops and art it’s time for me to start acting like a grumpy old man, declare galleries and zine libraries and makeshift venues. Every town punk rock dead, and start whining about how bands today are I went to inspired me a little more. just second-rate knock-offs of the bands that I grew up loving. hen, I thought about all these books about punk rock Hell, I should be writing stories about “back in the day” for that have been coming out lately, and about all the jaded Spin by now. But, somehow, the requisite feelings of being TTold guys talking about how things were more vital back jaded are eluding me. In fact, I’m downright optimistic. in the day. But I remember a lot of those days and that “How can this be?” you ask. -

Marillion on Leidsekade Live
Leidsekade Live (Hilversum, 21 April 1996) Marillion on Leidsekade Live On 22 April 1996 Marillion did an interview acoustic set that was broadcast on Dutch radio. This is a transcription of that interview plus some photographs Note: all photographs were made by Bart Stringa! Thanks! ... Shouty audience... clapping... Mark Stakenburg: Welcome, Steve Hogarth to Leidsekade Live. You just released a double live album called Made Again. It was recorded in Paris, London and Rotterdam. Why Rotterdam, because it's kind of a difficult hole to get a really good sound, I think. Steve Hogarth: No, that's true, it is a bit of a shed, isn't it, the Ahoy. But there is always an amazing crowd there, it always tends to sell out. And it's nice to capture the atmosphere of the crowd because the difference between recorded studio albums and live albums is the crowd, really. The band are usually worse, you know, live. But you've got a crowd. And that's the whole point of making a live record is to try and capture the way the musicians respond to the crowd. The way that bounces back and to. And Netherlands has always been a precious market for the band. M: You have a hard following here. S: Yes, of course, a very passionate following. So it's the obvious country to come to for us to make a live recording. M: Is it more difficult to perform knowing there is a tape rolling? So that it's going to be an album maybe? S: Yeah, it is actually. -

Pizza & Grinders
POSTAL PATRON www.westbendnews.net VOLUME 11 – ISSUE 32 Good News for Good Communities - Serving Northwest Ohio and Northeast Indiana WEDNESDAY, AUGUST 12, 2015 2015 HARLAN DAYS RAFFLE WINNERS! BROUGHTON REDNECK OAKWOOD GEARS UP FOR THE 2015 ANTWERP SCHOOL JAMBOREE WAS JAMMIN’ HOMECOMING: “OAKWOOD COUNTRY FAIR” REUNION Plans are well underway for Oakwood’s annual La- bor Day Weekend Home- coming and the traditional kick off dinner sponsored by the Event Planners. This dinner and entertain- ment, held in the big tent will provide needed funds for the Cooper Communi- ty Library, a branch of the Paulding County Carnegie library. Guests have come to expect great table settings, Harlan Days grand prize winner, John Alexander of Monro- great food, and entertain- eville with his brand new Chevy Spark. ment at these events and The Harlan Days Com- from Korte – Kent Von Gunt- won’t be disappointed as mittee is happy to announce en Russell Long, 94 years young the Event Planners change the 2015 Harlan Days Raf- 5th – Cherry Hill Golf – Air Force veteran. More pic- things up a little this year fle winners. Again this year, Larry Yoder of Hicksville, tures at westbendnews.net. in keeping with the theme over 2,500 raffle tickets were OH This is the 10th anniver- for the weekend festivities, sold and we were able to give 6th – Gas Trimmer – Ryan sary for the annual Brough- “Oakwood Country Fair”. away the 2015 Chevy Spark! Kennerk ton Redneck Jamboree set Cooper’s famous mar- Planning to send your child to Planning to send yourThe followingchild to are this year’s 7th – $100 A Lily’s Dew right in the center of town. -

MARILLION - Brave
DPRP : COUNTING OUT TIME Back to COT index DPRP main page MARILLION - Brave Staring out over the bridge A million photo flashes from the water down below Dawn light bouncing through the mist Roar of traffic and the crack of police radios When they ask her name Would she please explain She simply chooses to say ... nothing Life after Fish When frontman Fish left the band in 1988, Marillion stood for the difficult task of finding an equal replacement. During the rest of 1988 and the beginning of 1989 they continued song writing with bass-player Pete Trewavas on vocals, while the lyrics for their new compositions came from writer John Helmer, they even played a few gigs in this four-men line-up. During the writing process they were however also holding auditions for new vocalists (among which were Galahad's Stuart Nicholson and Cyan's Nigel Voyle). Eventually their choice fell on the eccentric Steve Hogarth, a fairly unknown singer / songwriter / keyboard player who had previously played in eighties' bands The Europeans and How We Live. The band had realised that their only way forward without Fish would be with a lead singer who would in no way be trying to copy the two-meters- high Scot. But of course the 5'2" Hogarth was not only chosen for his height; his musical abilities would surely add to the Marillion compositions as well. The first post-Fish album Seasons End, was musically a natural follow up to Clutching at Straws, but many fans had to get used to Hogarth's voice, which was entirely different from Fish's. -

CD Times - Marillion
CD Times - Marillion http://www.cdtimes.co.uk/content.php?contentid=4259 Search Go Advanced Homepage Reviews Gig Reviews Features Videos Downloads Forums MySpace Cover Marillion - Somewhere Else | 02-05-2007 15:30 Ratings My strongest memory of Marillion form back in the day, was that I once went to Rating: 5 a bargain Our Price record shop and tried to buy a Marillion album on cassette but accidently bought an album by tranny pop icon Marilyn instead. User Rating: No ratings have been Now this could have been an early sign of dyslexia, or a subconscious display of logged desired tranny gayness or just a mistake...But all I can remmber is that I was mighty annoyed about it at the time! You must be logged in to vote Anyway, 300 years later, Marillion, like every other band, are still going strong, have failed to accept their time has been and gone, and are knocking out music Affiliates CD Specs in search of the love they want and need as creative people.. Type: Please support CD Times CD Album Frankly, I don't blame them for sticking with it. I mean what else can they do? by ordering through our Go to work at Tescos? Set up a garden centre? Sell their guitars and start writing partners Release Date: classical?? April 9th 2007 Number of Discs: Of course not. They are Marillion and they feel they have unfinished business. 1 Besides, they don't want to let the fans down, so here they are with LP number 14 Tracks: 1. -

Rock Album Discography Last Up-Date: September 27Th, 2021
Rock Album Discography Last up-date: September 27th, 2021 Rock Album Discography “Music was my first love, and it will be my last” was the first line of the virteous song “Music” on the album “Rebel”, which was produced by Alan Parson, sung by John Miles, and released I n 1976. From my point of view, there is no other citation, which more properly expresses the emotional impact of music to human beings. People come and go, but music remains forever, since acoustic waves are not bound to matter like monuments, paintings, or sculptures. In contrast, music as sound in general is transmitted by matter vibrations and can be reproduced independent of space and time. In this way, music is able to connect humans from the earliest high cultures to people of our present societies all over the world. Music is indeed a universal language and likely not restricted to our planetary society. The importance of music to the human society is also underlined by the Voyager mission: Both Voyager spacecrafts, which were launched at August 20th and September 05th, 1977, are bound for the stars, now, after their visits to the outer planets of our solar system (mission status: https://voyager.jpl.nasa.gov/mission/status/). They carry a gold- plated copper phonograph record, which comprises 90 minutes of music selected from all cultures next to sounds, spoken messages, and images from our planet Earth. There is rather little hope that any extraterrestrial form of life will ever come along the Voyager spacecrafts. But if this is yet going to happen they are likely able to understand the sound of music from these records at least. -

Marillion.Com " Non Lascia Il Segno
Marillion Scritto da Montag Domenica 01 Novembre 2009 15:18 - Il primo 'nucleo' dei Marillion nasce nel '78 da un'idea del batterista Mick Pointer. Il nome del gruppo è Silm arillion , nome tratto da un libro pubblicato postumo di J.R.R. Tolkien, autore e ispiratore (involontario) di un genere letterario che è il Fantasy . All'inizio i Silmarillion sono una band strumentale, con influenze non definite ma con una propensione ad una musica piuttosto complessa. Ma il gruppo è giovane e, dopo i primi 'disastri' live, chitarrista e tastierista se ne vanno. L'anno successivo, grazie ai soliti e mitici annunci sulle riviste di settore, si unisce al gruppo Ste ve Rothery , un chitarrista affascinato da artisti quali Gilmour, Hackett e Latimer. La sintonia con il resto del gruppo, in special modo con Mick, è totale. Si riesce a trovare un tastierista, Brian Jelliman, e il nome del gruppo viene 'accorciato' a Marillion. Si cominciano a produrre i primi demo di carattere estremamente differente dai Marillion che conosciamo: musica barocca con tinte neoclassiche, inserti di flauto e un'aria bucolica pervade la loro proposta musicale. Si cercano ingaggi per concerti, e dopo vari fiaschi si arriva a suonare persino in una clinica psichiatrica (almeno così narra la leggenda...). Sul finire del '79 una piccola svolta: Doug Irvine (bassista) si cura delle parti cantate! Questa scelta (del canto, cioè) 'sconvolge' la musica dei Marillion. Da brani precedenti, come una fenice, sorge la prima 'canzone' della band, Close (che con Fish diverrà The Web ). Purtroppo, Doug lascia la band e i reduci sono costretti a cercare bassista e cantante. -
Marillion-Edelfan Severin Schneider (3
„NixNutz“ wird Fan-Pub: Britische Rock-Stars adeln Passauer Wirt! Kultband „Marillion“ erklärt Severin Schneiders Kneipe zum weltweit ersten offiziellen Fan-Pub Von Stefan Brandl Passau. Wer die Passauer Kneipe „NixNutz“ in der Innstadt besucht, dem sticht eins sofort ins Auge: Wo man auch hin- blickt, hängt oder steht irgend- was, das mit der Prog-Rock- Kultband „Marillion“ zu tun hat – Vinylscheiben, Poster, Platten- cover, T-Shirts, ja sogar am Passauer Wirt stolz wie Oskar: Marillion-Edelfan Severin Schneider (3. von rechts) bekam von Gtränkekühlschrank wurde der den Kult-Rockern (von links) Mark Kelly (Keyboards), Steve Rothery (Gitarre), Ian Mosley (Schlag- Bierlabel-Schriftzug mit dem zeug), Steve Hogarth (Gesang) und Pete Trewavas (Bass) persönlich das von ihnen signierte Aufdruck des aktuellen „Marilli- neue Kneipen-Schild fürs „NixNutz“ überreicht. Foto: Kühndel on“-Albums „F.E.A.R.“ ersetzt. Wirt Severin Schneider (47) hat allem, was auch nur irgendwie schnell gepackt hat, sind da na- ersten und bis dato einzigen sein „NixNutz“ zur Marillion-Fan- mit Marillion zu tun hat. türlich stets mit dabei. Marillion-Pub von der Band per- zentrale stilisiert. Jetzt haben ihn Klar, dass Severin Schneider Und genau das ist das Phäno- sönlich geadelt wurde, das hätte dafür die britischen Rockstars, im Team des deutschen Fan- men Marillion: zum einen die Severin Schneider fast umge- die 1985 mit dem Song „Kay- clubs „The Web Germany“ mit- opulente Gänsehaut-Musik, zum hauen: Vor ihrem Auftritt am 23. leigh“ einen Welthit und Klassi- wirkt. Dieses versorgt die über anderen aber die große Familie, Juli in Köln holten die fünf Rock- ker des Genres landeten, regel- 1 000 Mitglieder starke Fange- die die Fans untereinander mit stars den Passauer Wirt zu sich recht geadelt: Schneider darf ab meinde u.a. -

Dprp : Cd & Dvd Reviews
DPRP : CD & DVD REVIEWS http://www.dprp.net/reviews/200720.php | Back to Reviews | Back to DPRP Main [A] [B] [C] [D] [E] [F] [G] [H] [I] [J] [K] [L] [M] [N] [O] [P] [Q] [R] [S] [T] [U] [V] [W] [XYZ] [2007] [2006] [2005] [2004] [2003] [Misc] [DVD's] 2007 : VOLUME 20 Previous Volume Next Volume ROUND TABLE REVIEW Country of Origin: UK Format: CD Record Label: Townsend Records Catalogue #: - Year of Release: 2007 Time: 52:27 Info: Marillion Samples: Click here Tracklist: The Other Half (4:24), See It Like A Baby (4:29), Thankyou Whoever You Are (4:42), Most Toys (2:44), Somewhere Else (7:46), A Voice From The Past (6:12), No Such Thing (3:58), The Wound (7:11), The Last Century For Man (5:26), Faith (4:09) Tom De Val's Review Well, after months of the now customary pre-release hype, the new Marillion album is finally upon us. What to expect this time? Looking back at my review of Marbles, it was certainly very favourable, and whilst in hindsight I was perhaps a little over-generous with my rating of a 9.5, I still maintain that it’s a very fine album, and undoubtedly their best since one of their career highlights, Afraid Of Sunlight. So, with the band in a rich vein of form, surely it was a given that the next album would be another excellent effort? Well not necessarily – remember in the three years following Afraid… Marillion produced the rather patchy This Strange Engine and the frankly poor (and definite career lowlight) Radiation. -

Commonwealth of Pennsylvania Legislative
COMMONWEALTH OF PENNSYLVANIA LEGISLATIVE JOURNAL MONDAY, JUNE 29, 2009 SESSION OF 2009 193D OF THE GENERAL ASSEMBLY No. 55 HOUSE OF REPRESENTATIVES SENATE MESSAGE The House convened at 1 p.m., e.d.t. HOUSE AMENDMENTS CONCURRED IN BY SENATE THE SPEAKER (KEITH R. McCALL) PRESIDING The clerk of the Senate, being introduced, informed that the Senate has concurred in the amendments made by the House of PRAYER Representatives to SB 731, PN 1172. HON. RICHARD T. GRUCELA, member of the House of BILL SIGNED BY SPEAKER Representatives, offered the following prayer: Bill numbered and entitled as follows having been prepared Thank you, Mr. Speaker. for presentation to the Governor, and the same being correct, the Good afternoon. title was publicly read as follows: Please bow your heads in prayer, as today we are blessed to reach out in heart and soul to others. The challenges we meet in SB 731, PN 1172 life are more easily overcome when we turn our attention to the needs of family and friends. An Act designating Bushkill Drive, State Route 2019, Northampton County, as the Victor W. Anckaitis Memorial Highway; and Dear God, we pray that You will give perfection to designating a portion of State Route 2017 in Lower Macungie beginners, give intelligence to little ones, give sorrow to the Township, Lehigh County, as the Sgt. Ashly L. Moyer Memorial Road. negligent, and give aid to those who are running their course. We pray that every child has an opportunity to obtain a good Whereupon, the Speaker, in the presence of the House, education and that every adult who is thirsting for knowledge signed the same. -
Let's Get Writing!
Let's Get Writing! LET’S GET WRITING! Virginia Western Community College, Roanoke, Virginia Authors: Kathy Boylan, English Department Elizabeth Browning, English Department Katelyn Burton, Brown Library Kirsten DeVries, English Department Jenifer Kurtz, English Department Editor: Ann Moser, English Department Project Manager: Dale Dulaney, Brown Library Graphic Designer: Kalyca Schultz, Brown Library Peer Reviewers: Sarah Chitwood, English Department Nancy Francisco, Academic Link, Writing Center Janet Little, English Department Annie Woodford, English Department Christine Woods, English Department Publisher: Virginia Western Educational Foundation, Inc. Special Thanks: This book’s title is the suggestion of Eileen Franco, a student in Elizabeth Browning’s ENG 111 class. The cover is the work of Noah Sutphin, a student in ART 247, Painting Technique, created under the super- vision of Professor Sue Steele Thomas. Let's Get Writing! by Virginia Western Community College is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted. Contents Foreword: Why We Created an Open Textbook ix Dale Dulaney Introduction: About Writing and This Book 1 Ann Moser 1. Chapter 1 - Critical Reading 3 Elizabeth Browning 2. Chapter 2 - Rhetorical Analysis 21 Elizabeth Browning 3. Chapter 3 - Argument 34 Kirsten DeVries 4. Chapter 4 - The Writing Process 104 Kathy Boylan 5. Chapter 5 - Rhetorical Modes 128 Jenifer Kurtz 6. Chapter 6 - Finding and Using Outside Sources 181 Katelyn Burton 7. Chapter 7 - How and Why to Cite 197 Katelyn Burton 8. Chapter 8 - Writing Basics: What Makes a Good Sentence? 211 Jenifer Kurtz 9. Chapter 9 - Punctuation 269 Jenifer Kurtz 10. Chapter 10 - Working With Words: Which Word is Right? 290 Jenifer Kurtz Index 329 Foreword: Why We Created an Open Textbook DALE DULANEY This book was created for reasons quite diferent than most of the textbooks you have used so far in your academic career. -

Progwest Orchestra of Strategic Influence
3663 Commercial Way Spring Hill, FL 34606 www.musicnewsnetwork.net END OF SUMMER 2002 ISSUE #102 PAGE #1 From the Editor… Great News for It Bites fans as Matheos (Fates Warning), Hello everyone! Welcome to drummer Bob Dalton told our keyboardist Kevin Moore the ever-tardy issue #102. I’m friends at Silhobbit.com about (Chroma Key, formerly of please to say that life for this the past and future of the Dream Theater) and editor is coming together. band. There will be a double drummer Mike Portnoy Having recently moved back live CD and DVD both taken (Dream Theater, Transatlantic) to Florida, to be closer to my from a concert filmed for the official project name is family. Pease note the new Japanese TV in 1987. OSI. MNN address on the last Tentatively titled, Twice Bitten OSI will release its debut page. should be out in time for Christmas. album, 'Orchestra of Strategic Let me take this time to Influence,' in fall 2002 on assure you that MNN will get There are also plans to start a Inside Out Music. back on schedule from this new It Bites web site. Matheos, Moore and Portnoy point out. are the core of the band, PROGWEST and Moore does most of the Thanks for your patience, and There are still tickets left for lead vocals, but 'Orchestra of continued support. ProgWest 2003 in Claremont Strategic Influence' will also Christine CA. at Mudd Auditorium. This feature special guest year’s event was bumped up vocalists to be announced, to two days (November 9-10) and guest bass guitarist Sean MORSE QUITS PROG so as to include more music.