TUBA1A Families Say
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Transcriptomic Analysis of Human Brain Microvascular Endothelial
www.nature.com/scientificreports OPEN Transcriptomic analysis of human brain microvascular endothelial cells exposed to laminin binding protein (adhesion lipoprotein) and Streptococcus pneumoniae Irene Jiménez‑Munguía1, Zuzana Tomečková1, Evelína Mochnáčová1, Katarína Bhide1, Petra Majerová2 & Mangesh Bhide1,2* Streptococcus pneumoniae invades the CNS and triggers a strong cellular response. To date, signaling events that occur in the human brain microvascular endothelial cells (hBMECs), in response to pneumococci or its surface adhesins are not mapped comprehensively. We evaluated the response of hBMECs to the adhesion lipoprotein (a laminin binding protein—Lbp) or live pneumococci. Lbp is a surface adhesin recently identifed as a potential ligand, which binds to the hBMECs. Transcriptomic analysis was performed by RNA‑seq of three independent biological replicates and validated with qRT‑PCR using 11 genes. In total 350 diferentially expressed genes (DEGs) were identifed after infection with S. pneumoniae, whereas 443 DEGs when challenged with Lbp. Total 231 DEGs were common in both treatments. Integrative functional analysis revealed participation of DEGs in cytokine, chemokine, TNF signaling pathways and phagosome formation. Moreover, Lbp induced cell senescence and breakdown, and remodeling of ECM. This is the frst report which maps complete picture of cell signaling events in the hBMECs triggered against S. pneumoniae and Lbp. The data obtained here could contribute in a better understanding of the invasion of pneumococci across BBB and underscores role of Lbp adhesin in evoking the gene expression in neurovascular unit. Streptococcus pneumoniae (also known as pneumococcus) is a life-threatening pathogen responsible for high morbidity and mortality rates worldwide1. It can cross the blood–brain barrier (BBB) and cause meningitis, commonly known as pneumococcal meningitis, a rare but life-threatening medical emergency. -

Supplementary Materials
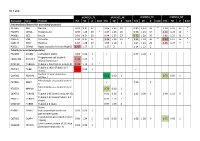
1 Supplementary Materials: Supplemental Figure 1. Gene expression profiles of kidneys in the Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice. (A) A heat map of microarray data show the genes that significantly changed up to 2 fold compared between Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice (N=4 mice per group; p<0.05). Data show in log2 (sample/wild-type). 2 Supplemental Figure 2. Sting signaling is essential for immuno-phenotypes of the Fcgr2b-/-lupus mice. (A-C) Flow cytometry analysis of splenocytes isolated from wild-type, Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice at the age of 6-7 months (N= 13-14 per group). Data shown in the percentage of (A) CD4+ ICOS+ cells, (B) B220+ I-Ab+ cells and (C) CD138+ cells. Data show as mean ± SEM (*p < 0.05, **p<0.01 and ***p<0.001). 3 Supplemental Figure 3. Phenotypes of Sting activated dendritic cells. (A) Representative of western blot analysis from immunoprecipitation with Sting of Fcgr2b-/- mice (N= 4). The band was shown in STING protein of activated BMDC with DMXAA at 0, 3 and 6 hr. and phosphorylation of STING at Ser357. (B) Mass spectra of phosphorylation of STING at Ser357 of activated BMDC from Fcgr2b-/- mice after stimulated with DMXAA for 3 hour and followed by immunoprecipitation with STING. (C) Sting-activated BMDC were co-cultured with LYN inhibitor PP2 and analyzed by flow cytometry, which showed the mean fluorescence intensity (MFI) of IAb expressing DC (N = 3 mice per group). 4 Supplemental Table 1. Lists of up and down of regulated proteins Accession No. -

Cytoplasmic Mrna Decay Represses RNA Polymerase II Transcription
RESEARCH ARTICLE Cytoplasmic mRNA decay represses RNA polymerase II transcription during early apoptosis Christopher Duncan-Lewis1, Ella Hartenian1, Valeria King1, Britt A Glaunsinger1,2,3* 1Department of Molecular and Cell Biology; University of California, Berkeley, Berkeley, United States; 2Department of Plant and Microbial Biology; University of California, Berkeley, Berkeley, United States; 3Howard Hughes Medical Institute, Berkeley, Berkeley, United States Abstract RNA abundance is generally sensitive to perturbations in decay and synthesis rates, but crosstalk between RNA polymerase II transcription and cytoplasmic mRNA degradation often leads to compensatory changes in gene expression. Here, we reveal that widespread mRNA decay during early apoptosis represses RNAPII transcription, indicative of positive (rather than compensatory) feedback. This repression requires active cytoplasmic mRNA degradation, which leads to impaired recruitment of components of the transcription preinitiation complex to promoter DNA. Importin a/b-mediated nuclear import is critical for this feedback signaling, suggesting that proteins translocating between the cytoplasm and nucleus connect mRNA decay to transcription. We also show that an analogous pathway activated by viral nucleases similarly depends on nuclear protein import. Collectively, these data demonstrate that accelerated mRNA decay leads to the repression of mRNA transcription, thereby amplifying the shutdown of gene expression. This highlights a conserved gene regulatory mechanism by which cells respond to threats. *For correspondence: [email protected] Competing interests: The authors declare that no Introduction competing interests exist. Gene expression is often depicted as a unidirectional flow of discrete stages: DNA is first transcribed Funding: See page 18 by RNA polymerase II (RNAPII) into messenger RNA (mRNA), which is processed and exported to Received: 28 April 2020 the cytoplasm where it is translated and then degraded. -

Alpha Tubulin (TUBA1A) Chicken Polyclonal Antibody Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for TA306750 alpha Tubulin (TUBA1A) Chicken Polyclonal Antibody Product data: Product Type: Primary Antibodies Applications: WB Recommended Dilution: WB: 0.5 - 1 ug/mL Reactivity: Human, Mouse, Rat Host: Chicken Isotype: IgY Clonality: Polyclonal Immunogen: Tubulin antibody was raised against a 16 amino acid peptide near the amino terminus of human Tubulin. Formulation: PBS containing 0.02% sodium azide. Concentration: 1ug/ul Purification: Affinity chromatography purified via peptide column Conjugation: Unconjugated Storage: Store at -20°C as received. Stability: Stable for 12 months from date of receipt. Gene Name: tubulin alpha 1a Database Link: NP_006000 Entrez Gene 22142 MouseEntrez Gene 64158 RatEntrez Gene 7846 Human Q71U36 This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 2 alpha Tubulin (TUBA1A) Chicken Polyclonal Antibody – TA306750 Background: Alpha-tubulin belongs to the tubulin superfamily, which is composed of six distinct families. Along with beta-tubulins, alpha-tubulins are the major components of microtubules. These microtubules are involved in a wide variety of cellular activities ranging from mitosis and transport events to cell movement and the maintenance of cell shape. Alpha- and beta- tubulin dimers are assembled to 13 protofilaments that form a microtubule of 22-nm diameter. Tyrosine ligase adds a C-terminal tyrosine to monomeric alpha-tubulin. -
S1 Table Protein
S1 Table dFSHD12_TE dFSHD12_NE aFSHD51_TE aFSHD51_NE Accession Gene Protein H/L SD # bold H/L SD # bold H/L SD # bold H/L SD # bold Intermediate filament (or associated proteins) P17661 DES Desmin 0.91 N.D. 37 1.06 1.35 19 0.89 1,13 33 * 1.20 1.21 17 * P02545 LMNA Prelamin-A/C 0.90 1.25 30 * 1.07 1.26 20 0.96 1.23 34 1.21 1.24 19 * P48681 NES Nestin 0.91 N.D. 60 0.94 1.25 27 0.72 1.20 50 * 0.89 1.27 31 * P08670 VIM Vimentin 1.04 N.D. 35 1.24 1.24 14 * 1.21 1.18 36 * 1.39 1.17 16 * Q15149 PLEC Plectin-1 1.10 1.28 19 1.05 1.10 3 1.07 1.23 26 1.25 1.27 7 * P02511 CRYAB Alpha-crystallin B chain (HspB5) 1.47 1.17 2 1.17 2 1.14 1.12 2 Tubulin (or associated proteins) P62158 CALM1 Calmodulin (CaM) 0.83 0.00 1 0.93 0.00 1 Programmed cell death 6- Q8WUM4 PDCD6IP 1.34 0.00 1 interacting protein Q71U36 TUBA1A Tubulin α-1A chain (α-tubulin 3) 1.44 1.12 3 * Tubulin β chain (Tubulin β-5 P07437 TUBB 1.52 0.00 1 chain) Nuclear mitotic apparatus Q14980 NUMA1 0.68 0.00 1 0.75 0.00 1 protein 1 Microtubule-associated protein P27816 MAP4 1.10 1 4 Microtubule-associated protein P78559 MAP1A 0.76 0.00 1 1A Q6PEY2 TUBA3E Tubulin α-3E chain (α-tubulin 3E) 0.91 0.00 1 1.12 0.00 1 0.98 1.12 3 Tubulin β-2C chain (Tubulin β-2 P68371 TUBB2C 0.93 1.13 7 chain) Q3ZCM7 TUBB8 Tubulin β-8 chain 0.97 1.09 4 Serine P34897 SHMT2 hydroxymethyltransferase 0.93 0.00 1 (serine methylase) Cytoskeleton-associated protein Q07065 CKAP4 0.98 1.24 5 0.96 0.00 1 1.08 1.28 6 0.75 0.00 1 4 (p63) Centrosomal protein of 135 kDa Q66GS9 CEP135 0.84 0.00 1 (Centrosomal protein 4) Pre-B cell leukemia transcription Q96AQ6 PBXIP1 0.74 0.00 1 0.80 1 factor-interacting protein 1 T-complex protein 1 subunit P17897 TCP1 0.84 0.00 1 alpha (CCT-alpha) Cytoplasmic dynein Q13409 DYNC1I2 1.01 0.00 1 intermediate chain 2 (DH IC-2) Dynein heavy chain 3 (Dnahc3- Q8TD57 DNAH3 b) Microtubule-actin cross- linking Q9UPN3 MACF1 factor 1 (Trabeculin-alpha) Actin (or associated including myofibril-associated porteins) P60709 ACTB Actin, cytoplasmic 1 (β-actin) 1.11 N.D. -

Conditional Gene Expression and Lineage Tracing of Tuba1a Expressing Cells During Zebrafish Development and Retina Regeneration
RESEARCH ARTICLE Conditional Gene Expression and Lineage Tracing of tuba1a Expressing Cells During Zebrafish Development and Retina Regeneration Rajesh Ramachandran,1 Aaron Reifler,1,2 Jack M. Parent,2,3 and Daniel Goldman1,2,4* 1Molecular and Behavioral Neuroscience Institute, University of Michigan, Ann Arbor, Michigan 48109 2Neuroscience Program, University of Michigan, Ann Arbor, Michigan 48109 3Department of Neurology, University of Michigan, Ann Arbor, Michigan 48109 4Department of Biological Chemistry, University of Michigan, Ann Arbor, Michigan 48109 ABSTRACT During development, recombination revealed transient The tuba1a gene encodes a neural-specific a-tubulin tuba1a expression in not only neural progenitors but isoform whose expression is restricted to the develop- also cells that contribute to skeletal muscle, heart, and ing and regenerating nervous system. By using zebra- intestine. In the adult, recombination revealed tuba1a fish as a model system for studying CNS regeneration, expression in brain, olfactory neurons, and sensory cells we recently showed that retinal injury induces tuba1a of the lateral line, but not in the retina. After retinal gene expression in Mu¨ller glia that reentered the cell injury, recombination showed tuba1a expression in cycle. However, because of the transient nature of Mu¨ller glia that had reentered the cell cycle, and line- tuba1a gene expression during development and regen- age tracing indicated that these cells are responsible eration, it was not possible to trace the lineage of the for regenerating retinal neurons and glia. These results tuba1a-expressing cells with a reporter directly under suggest that tuba1a-expressing progenitors contribute the control of the tuba1a promoter. To overcome this to multiple cell lineages during development and that limitation, we generated tuba1a:CreERT2 and b-actin2: tuba1a-expressing Mu¨ller glia are retinal progenitors in loxP-mCherrry-loxP-GFP double transgenic fish that the adult. -

Genomics of Inherited Bone Marrow Failure and Myelodysplasia Michael
Genomics of inherited bone marrow failure and myelodysplasia Michael Yu Zhang A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Washington 2015 Reading Committee: Mary-Claire King, Chair Akiko Shimamura Marshall Horwitz Program Authorized to Offer Degree: Molecular and Cellular Biology 1 ©Copyright 2015 Michael Yu Zhang 2 University of Washington ABSTRACT Genomics of inherited bone marrow failure and myelodysplasia Michael Yu Zhang Chair of the Supervisory Committee: Professor Mary-Claire King Department of Medicine (Medical Genetics) and Genome Sciences Bone marrow failure and myelodysplastic syndromes (BMF/MDS) are disorders of impaired blood cell production with increased leukemia risk. BMF/MDS may be acquired or inherited, a distinction critical for treatment selection. Currently, diagnosis of these inherited syndromes is based on clinical history, family history, and laboratory studies, which directs the ordering of genetic tests on a gene-by-gene basis. However, despite extensive clinical workup and serial genetic testing, many cases remain unexplained. We sought to define the genetic etiology and pathophysiology of unclassified bone marrow failure and myelodysplastic syndromes. First, to determine the extent to which patients remained undiagnosed due to atypical or cryptic presentations of known inherited BMF/MDS, we developed a massively-parallel, next- generation DNA sequencing assay to simultaneously screen for mutations in 85 BMF/MDS genes. Querying 71 pediatric and adult patients with unclassified BMF/MDS using this assay revealed 8 (11%) patients with constitutional, pathogenic mutations in GATA2 , RUNX1 , DKC1 , or LIG4 . All eight patients lacked classic features or laboratory findings for their syndromes. -

Tuba1a Microtubules Establish the Foundations for Neuronal
TUBA1A MICROTUBULES ESTABLISH THE FOUNDATIONS FOR NEURONAL FUNCTION by GEORGIA CHRISTINE BUSCAGLIA B.S., Syracuse University, 2014 A thesis submitted to the Faculty of the Graduate School of the University of Colorado in partial fulfillment of the requirements for the degree of Doctor of Philosophy Neuroscience Program 2020 This thesis for the Doctor of Philosophy degree by Georgia Christine Buscaglia has been approved for the Neuroscience Program by Abigail Person, Chair Jeffrey Moore Santos Franco Lee Niswander Matthew Kennedy Wendy Macklin Emily Bates, Advisor Date: May 22, 2020 ii Buscaglia, Georgia Christine (PhD., Neuroscience Program) Tuba1a Microtubules Establish the Foundations for Neuronal Function Thesis directed by Associate Professor Emily Bates ABSTRACT Developing neurons undergo dramatic morphological changes to appropriately migrate and extend axons to make synaptic connections. The microtubule cytoskeleton, made of a/b- tubulin dimers, drives neurite outgrowth, promotes neuronal growth cone responses, and facilitates intracellular transport of critical cargoes during neurodevelopment and in adulthood. The mechanisms by which neurons regulate microtubule network assembly and organization to respond appropriately to external cues are largely unknown. Cells express different a- and b-tubulin genes, or isotypes, providing one potential level of microtubule regulation. TUBA1A is the most abundant a-tubulin isotype in the developing brain and mutations to TUBA1A in humans cause severe brain malformations. The role of TUBA1A in the adult brain is largely unknown. We use a loss-of-function mutation to Tuba1a, Tuba1aN102D, to investigate requirements for Tuba1a in developing and adult neurons. Tuba1aND substitution reduced the amount of Tuba1a protein and prevented incorporation of Tuba1a into cellular microtubule polymers. -

Organelle Markers
Novus-lu-2945 Antibodies for Organelle Markers Centrioles Mitochondria (PCNT, TUBG1, NIN) (CYCS, SDHB, COX4, HSP60) Microvilli (ALP, GGT) Microtubules (TUBA1A, MAP4) Endosomes (EEA1, Tfr, CD63) Nucleolus (FBL, Nop1p) Cell Membrane (CDH1, CDH2, CD44) Nucleus Golgi Apparatus (LSD1, Histones H2, H3 & H4) (GOLM1, 58k Golgi, TGN38) Endoplasmic Reticulum Lysosomes (PDI, CALR, KDEL) (CTSD, LAMP-2, LIMP-II) Learn more | novusbio.com Learn more | novusbio.com INTRODUCTION Eukaryotic cellular components are organized into membrane-bound compartments called organelles. These structurally complex compartments serve specific biological roles and are crucial for proper cellular function. For example, mitochondria carry out cellular respiration, while lysosomes function in cellular digestion to break down biomolecules. The specialized function of each organelle is determined by the unique proteins they contain. Organelle-specific proteins can function as markers to identify organelles in cell biology immunoassays, as well as act as a tool to explore the subcellular localization of novel proteins. By immunostaining for the protein of interest along with an organelle marker, their co-localization confirms the subcellular localization of the target protein. In addition, organelle markers can be used in Western blot analysis to confirm the purity of various fractions in experiments involving cellular fractionation. Learn more | novusbio.com Learn more | novusbio.com Gold Standard Organelle Markers Centrioles Mitochondria (PCNT, TUBG1, NIN) (CYCS, SDHB, COX4, HSP60) Microvilli (ALP, GGT) Microtubules (TUBA1A, MAP4) Endosomes (EEA1, Tfr, CD63) Nucleolus (FBL, Nop1p) Cell Membrane (CDH1, CDH2, CD44) Nucleus Golgi Apparatus (LSD1, Histones H2, H3 & H4) (GOLM1, 58k Golgi, TGN38) Endoplasmic Reticulum Lysosomes (PDI, CALR, KDEL) (CTSD, LAMP-2, LIMP-II) Novus Biologicals offers extensively validated, high quality antibodies for various organelle markers. -

Cytoskeletal Proteins in Neurological Disorders
cells Review Much More Than a Scaffold: Cytoskeletal Proteins in Neurological Disorders Diana C. Muñoz-Lasso 1 , Carlos Romá-Mateo 2,3,4, Federico V. Pallardó 2,3,4 and Pilar Gonzalez-Cabo 2,3,4,* 1 Department of Oncogenomics, Academic Medical Center, 1105 AZ Amsterdam, The Netherlands; [email protected] 2 Department of Physiology, Faculty of Medicine and Dentistry. University of Valencia-INCLIVA, 46010 Valencia, Spain; [email protected] (C.R.-M.); [email protected] (F.V.P.) 3 CIBER de Enfermedades Raras (CIBERER), 46010 Valencia, Spain 4 Associated Unit for Rare Diseases INCLIVA-CIPF, 46010 Valencia, Spain * Correspondence: [email protected]; Tel.: +34-963-395-036 Received: 10 December 2019; Accepted: 29 January 2020; Published: 4 February 2020 Abstract: Recent observations related to the structure of the cytoskeleton in neurons and novel cytoskeletal abnormalities involved in the pathophysiology of some neurological diseases are changing our view on the function of the cytoskeletal proteins in the nervous system. These efforts allow a better understanding of the molecular mechanisms underlying neurological diseases and allow us to see beyond our current knowledge for the development of new treatments. The neuronal cytoskeleton can be described as an organelle formed by the three-dimensional lattice of the three main families of filaments: actin filaments, microtubules, and neurofilaments. This organelle organizes well-defined structures within neurons (cell bodies and axons), which allow their proper development and function through life. Here, we will provide an overview of both the basic and novel concepts related to those cytoskeletal proteins, which are emerging as potential targets in the study of the pathophysiological mechanisms underlying neurological disorders. -

It Was Hypothesized That Hybrid Synthetic/Adenoviral Nanoparticles
Electronic Supplementary Material (ESI) for Nanoscale. This journal is © The Royal Society of Chemistry 2020 SUPPORTING INFORMATION Lana Papafilippou,a Andrew Claxton,b Paul Dark,b,c Kostas Kostarelos*a,d and Marilena Hadjidemetriou*a aNanomedicine Lab, Faculty of Biology, Medicine & Health, AV Hill Building, The University of Manchester, Manchester, M13 9PT, UK bCentre for Acute Care Trauma, Manchester Academic Health Science Centre, Health Innovation Manchester, Division of Critical Care, Salford Royal NHS Foundation Trust, Greater Manchester, UK cDivision of Infection, Immunity and Respiratory Medicine, Faculty of Biology, Medicine & Health, AV Hill Building, The University of Manchester, Manchester, M13 9PT, UK. d Catalan Institute of Nanoscience and Nanotechnology (ICN2), Campus UAB, Bellaterra, 08193 Barcelona, Spain. _______________________________________ * Correspondence should be addressed to: [email protected],uk; [email protected] 1 Supporting Figure 1 Figure S1: Physicochemical characterization of corona-coated Amphotericin B-intercalated liposomes (AmBisome®). Mean hydrodynamic diameter (nm) and ζ-potential (mV) distributions are depicted for corona-coated liposomal formulation AmBisome® recovered post-incubation with human plasma from 12 healthy volunteers, 7 SIRS patients and 12 sepsis patients. 2 Supporting Figure 2 Figure S2: Proteomic analysis of corona profiles. (A) Heatmap of normalized abundance values of all corona proteins identified in healthy controls, SIRS patients and sepsis patients, as identified by LC-MS/MS (Progenesis QI). Protein columns are sorted according to the abundance values (from highest to lowest) of the first sample. The list of proteins shown in the heatmap, their respective accession numbers and their mean normalized abundance values are shown in Table S5; (B) Volcano plot represents the potential protein biomarkers differentially abundant between healthy donors and sepsis patients (n=135) identified in corona samples. -

Role of Gigaxonin in the Regulation of Intermediate Filaments: a Study Using Giant Axonal Neuropathy Patient-Derived Induced Pluripotent Stem Cell-Motor Neurons
Role of Gigaxonin in the Regulation of Intermediate Filaments: a Study Using Giant Axonal Neuropathy Patient-Derived Induced Pluripotent Stem Cell-Motor Neurons Bethany Johnson-Kerner Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy under the Executive Committee of the Graduate School of Arts and Sciences COLUMBIA UNIVERSITY 2013 © 2012 Bethany Johnson-Kerner All rights reserved Abstract Role of Gigaxonin in the Regulation of Intermediate Filaments: a Study Using Giant Axonal Neuropathy Patient-Derived Induced Pluripotent Stem Cell-Motor Neurons Bethany Johnson-Kerner Patients with giant axonal neuropathy (GAN) exhibit loss of motor and sensory function and typically live for less than 30 years. GAN is caused by autosomal recessive mutations leading to low levels of gigaxonin, a ubiquitously-expressed cytoplasmic protein whose cellular roles are poorly understood. GAN pathology is characterized by aggregates of intermediate filaments (IFs) in multiple tissues. Disorganization of the neuronal intermediate filament (nIF) network is a feature of several neurodegenerative disorders, including amyotrophic lateral sclerosis, Parkinson’s disease and axonal Charcot-Marie-Tooth disease. In GAN such changes are often striking: peripheral nerve biopsies show enlarged axons with accumulations of neurofilaments; so called “giant axons.” Interestingly, IFs also accumulate in other cell types in patients. These include desmin in muscle fibers, GFAP (glial fibrillary acidic protein) in astrocytes, and vimentin in multiple cell types including primary cultures of biopsied fibroblasts. These findings suggest that gigaxonin may be a master regulator of IFs, and understanding its function(s) could shed light on GAN as well as the numerous other diseases in which IFs accumulate.