False Low-Risk Single Nucleotide Polymorphism–Based Noninvasive Prenatal Screening in Pentasomy 49,XXXXY
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

XXXXX Syndrome
XXXXX Syndrome 49,XXXXX (pentasomy X) is a rare sex chromosome aneu- 2. Craniofacial features ploidy. The birth prevalence of pentasomy X is estimated to be a. Microcephaly 1 in 85,000 females. b. Flattened occiput c. Epicanthus d. Upslanting palpebral fissures GENETICS/BASIC DEFECTS e. Ocular hypertelorism 1. Etiology: Three extra X chromosomes are responsible for f. Uncoordinated eye movements the pentasomy X syndrome. g. Flat broad nose 2. Occurrence of a 49,XXXXX complement: secondary to h. Cleft palate sequential non-disjunctions in meiosis I and meiosis II in i. Low-set ears the mother j. Malformed teeth a. Involves the survival of both X chromosomes in a sin- 3. Skeletal abnormalities gle oocytes through both meiotic divisions a. Short neck i. Once between homologous X chromosomes at b. Lax joints the first meiosis c. Multiple dislocations ii. Twice between sister chromatids in both X chro- i. Shoulders mosomes in the secondary oocytes at the second ii. Elbows meiosis iii. Hips b. Followed by the fertilization by a sperm contributing d. Radioulnar synostosis the 5th chromosome X e. Spinal abnormalities 3. Formation of four Barr bodies f. Clinodactyly of the 5th fingers a. Lyon hypothesis g. Lower leg abnormalities i. Inactivation of all X chromosomes but one i. Genu valgus ii. Account for the viability of the X-chromosome ii. Talipes aneuploidies iii. Metatarsus varus b. Inactivation of four X chromosomes resulting in four h. Delayed bone age Barr bodies 4. Congenital heart defects 4. Effect of supernumerary X chromosomes: a direct rela- a. Ventricular septal defect tionship between the number of supernumerary X chro- b. -
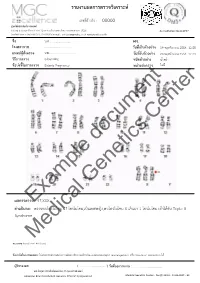
Example Document Medical Genetics Center
รายงานผลการตรวจววเคราะหย เลขทธรออางอนง : 00000 ศผนยยพวนธธศาสตรยการแพทยย 6/6 หมนม 6 ถนนสสขาภนบาล 5 ซอย 32 แขวงออเงนน เขตสายไหม กรสงเทพมหานคร 10220 Accreditation No.4148/57 โทรศกพทย/โทรสาร 086-8861203, 02-7920726 e-mail : [email protected] www.genetics.co.th ชชชอ น.ส............................. HN. ............. โรงพยาบาล .................................... ววนททชเกกบตววอยยาง 19 พฤศจนกายน 2558 12:55 แพทยยผผผสวชงตรวจ นพ.................................... ววนททชรวบตววอยยาง 20 พฤศจนกายน 2558 12:43 ววธทการตรวจ G-banding ชนวดตววอยยาง นนนาครรนา ขผอบยงชทชในการตรวจ Elderly Pregnancy หนยวยสยงตรวจ ไมมมธ Center document Genetics ผลการตรวจExample: 47,XXX คคาอธวบาย : ตรวจพบโครโมโซม 47 โครโมโซม,เปปนเพศหญนง,พบโครโมโซม X เกนนมา 1 โครโมโซม เขอาไดอกกบ Triple X Syndrome Medical หมายเหตธ: Band level 450 band ขผอจคากวดในการทดสอบ: ไมมสามารถตรวจสอบความผนดปกตนขนาดเลลกชนนด submicroscopic rearrangement หรรอ low-level mosaicism ไดอ ผผผรวบรองผล ( .................................. ) ววนททชออกรายงาน : ....................................... นพ.วทรยธทธ ประพวนธยพจนย,พบ.,วว.กธมารเวชศาสตรย American Board of Medical Genetics (Clinical Cytogenetics) Medical Genetics Center : Fo-QP-19/01 : 16-03-2015 : 02 เรียน อ.นพ...................................... ที่นับถือ ตามที่ผลตรวจโครโมโซมจากน ้าคร่้าของ นส........................ (HN .............., Lab no. ..............) พบ โครโมโซม X เกินมา 1 โครโมโซมนั น ความผิดปกติดังกล่าว เข้าได้กับกลุ่มอาการ trisomy X หรือ triple X syndrome ซึ่งเป็นความผิดปกติของโครโมโซมเพศที่พบได้บ่อยในทารกเพศหญิง โดยความผิดปกติของ โครโมโซมแบบนี -
Inside This Issue
Winter 2014 No. 77 Inside this issue Group News | Fundraising | Members’ Letters | One Family Living with Two Different Chromosome Disorders | Bristol Conference 2014 | Unique Leaflets | Christmas Card Order Form Sophie, Unique’s Chair of Trustees Dear Members, In the past month a few things have reminded me of why it is so important to make connections through Unique but also to draw support from other parents around us. I’ve just returned from Unique’s most recent family conference in Bristol where 150 of us parents and carers had a lovely time in workshops, meals and activities, chatting and watching our children milling around together like one big family since – although we had never met before – we have shared so many experiences in common. However in contrast I have also just met a new mum who has just moved to my area from far away with two toddlers, one with a rare joys of the internet, it is becoming easier to meet others with similar, chromosome disorder, who is starting from scratch with no even very rare, chromosome disorders around the world and to find professional, medical or social support. She reminds me of how yourself talking to them in the middle of the night about some lonely I felt when Max was newly diagnosed, when I knew no one interesting things our children share in common (obsession with with a disabled child let alone anyone with a rare chromosome catalogues, anyone?) And of course we also have an enormous disorder. Elsewhere our latest Unique Facebook group, Unique amount in common with so many parents of children with other Russia, is also just starting up – so far it includes just a small special needs or disabilities around us in our own communities who number of members sharing very different experiences to mine here will often be walking the same path as us. -

Female Polysomy-X and Systemic Lupus Erythematosus
Seminars in Arthritis and Rheumatism 43 (2014) 508–512 Contents lists available at ScienceDirect Seminars in Arthritis and Rheumatism journal homepage: www.elsevier.com/locate/semarthrit Female polysomy-X and systemic lupus erythematosus Mordechai Slae, MDa,n, Merav Heshin-Bekenstein, MDb, Ari Simckes, MDb, Gali Heimer, MDb, Dan Engelhard, MDb, Eli M. Eisenstein, MDc a Department of Pediatrics, University of Alberta Hospital, Edmonton, Alberta, Canada b Department of Pediatrics, Hadassah-Hebrew University Hospital at Ein Kerem, Jerusalem, Israel c Department of Pediatrics, Hadassah-Hebrew University Hospital at Mount-Scopus, Jerusalem, Israel article info abstract Objectives: Systemic lupus erythematosus (SLE) occurs more commonly in females than in males. Recent Keywords: evidence suggests that genetic factors transmitted by the X-chromosome may confer increased risk for Gene dosage autoimmune disease in general, and for SLE in particular. It is therefore possible that X-chromosome Lupus genetics polysomy might confer further increased risk for lupus. In addition to describing the clinical and Polysomy-X immunologic features of a young woman with polysomy-X and SLE, we sought to review all other Sex differences published cases associating female or male polysomy-X with SLE or other forms of autoimmunity. SLE Methods: We report a case of a prepubertal girl with polysomy-X and SLE. We performed a systemic X-chromosome literature review for cases of polysomy-X and SLE and summarize previously published cases. In addition, we reviewed reports concerning the possible association between SLE and other connective tissue diseases and male polysomy-X. Results: An 11-year-old girl with tetrasomy-X (48 XXXX karyotype) presented with prolonged fever. -

蝪case Report D
å¡ CASE REPORT D Pentasomy X Mosaic in Two Adult Sisters with Diabetes Mellitus Shigeru Nakano, Atsuko Sasame, Sadahide Azukizawa, Toshikazu Kigoshi, Kenzo Uchida, Hiroaki Takahashi* and Shinpei Morimoto Pentasomy X mosaic in two adult sisters with non-insulin dependent diabetes mellitus is described. The younger sister had schizophrenia, and both were mentally retarded, but no apparent somatic abnormalities were found. Chromosome analyses revealed karyotype 45,X/ 46,XX/47,XXX/48,XXXX/49,XXXXX mosaic with a low frequency of aneuploidy on cultured peripheral lymphocytes and 46,XX on cultured skin fibroblasts in both sisters. The low fre quency of X chromosome aberration may be responsible for the lack of somatic abnormalities and the long life in both sisters. The association of pentasomy X mosaicism and diabetes mellitus (Internalhowever Medicineappears to 31: be 1102-1106,coincidental. 1992) Key words: X chromosome aneuploidy, aged siblings, glucose intolerance Intr oduction her behavior was quiet, shy and timid. Intelligence quotient (IQ) obtained from the results of WAIS-R Pentasomy X and its mosaicism, rare X chromosomal tests was 55, verbal IQ 62 and performance IQ 50. Her constitutions, are generally found in young (neonate to height was 143 cm, weight 38 kg and head circumference childhood) females because of concomitant mental 53cm. Her blood pressure was 98/58mmHg; the pulse and somatic abnormalities; mental retardation and rate was 74 beats/min and regular. She had no apparent mongoloid face, congenital heart disease and various somatic abnormalities (Fig. 1). Her fundus oculi showed skeletal anomalies are associated (1-10). However, preproliferative diabetic retinopathy. -

A New Case of Prenatally Diagnosed Pentasomy X: Review of the Literature
Hindawi Publishing Corporation Case Reports in Obstetrics and Gynecology Volume 2015, Article ID 935202, 5 pages http://dx.doi.org/10.1155/2015/935202 Case Report A New Case of Prenatally Diagnosed Pentasomy X: Review of the Literature Linda Maria Azzurra Pirollo,1 Leila Baghernajad Salehi,2 Simona Sarta,1 Marco Cassone,3 Maria Vittoria Capogna,1 Emilio Piccione,1 Giuseppe Novelli,4 and Adalgisa Pietropolli1 1 Section of Gynecology and Obstetrics, Academic Department of Biomedicine and Prevention and Clinical Department of Surgery, Tor Vergata University Hospital, Viale Oxford 81, 00133 Rome, Italy 2Laboratory of Medical Genetics, Polyclinic of Tor Vergata Foundation, Viale Oxford 81, 00133 Rome, Italy 3Laboratory of Medical Genetics, University of Rome Tor Vergata, Via Montpellier 1, 00133 Rome, Italy 4Genetics Section, Department of Biomedicine and Prevention, University of Rome Tor Vergata, Via Montpellier 1, 00133 Rome, Italy Correspondence should be addressed to Linda Maria Azzurra Pirollo; [email protected] Received 2 December 2014; Revised 13 January 2015; Accepted 14 January 2015 Academic Editor: Olivier Picone Copyright © 2015 Linda Maria Azzurra Pirollo et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Pentasomy X is a rare chromosomal abnormality probably due to a nondisjunction during the meiosis. Only four cases prenatally diagnosed were described until now. Our case is the fifth one prenatally diagnosed at 20 weeks of gestational age in a 39-years- old woman. She underwent invasive prenatal diagnosis for her advanced maternal age without any other known risk factor. -

Help Raise Awareness for Chromosome Disorders
★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ Spring 2015 No. 78 SHINE BRIGHT AND BE UNIQUE ★ ★ Help raise awareness for ★ ★ ★ chromosome disorders ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ CHROMOSOME DISORDER AWARENESS 2015 7th –13th June 2015 ★ ★ ★ ★ ★★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ ★ For more information and ideas, ★ see pages 3 –5 ★ Inside this issue Group News | Fundraising | Members’ Letters | Awareness Week 7th –13th June 2015 | Unique’s Show Garden at Hampton Court Palace | The Compassettes Sophie, Unique’s Chair of Trustees Dear Members, Legacies Have you ever wondered why membership of Unique is free, why we don’t charge to join? I never gave it a thought until I became a trustee of Unique. Since Max’s birth I’ve joined lots of organisations and support groups that have helped in different ways and unlike Unique almost every one of them charges an annual fee. I discovered that at Unique it has always been a basic principle that we are free to join – both for families and for professionals. Why is membership free? We don’t want anyone to miss out on our helpline, on making connections with other families and on our magazine for financial reasons. We don’t charge for downloading the chromosome guides either as we want families and professionals to get immediate unrestricted access to high quality combination of grants from charitable foundations and donations from information. But another reason for not charging is that one of the most members and more and more from the amazing fundraising activities so important and unique (!) things that Unique does is to collect in its many of you do for Unique: those marathons and 10k runs, those cake database life-time information about all our children and their medical sales and dress-down days, and so much more. -

Tetrasomy X in a Child with Multiple Abnormalities: Case Report and Literature Review from China
HK J Paediatr (new series) 2014;19:37-40 Tetrasomy X in a Child with Multiple Abnormalities: Case Report and Literature Review from China WY XIONG, ZY JIANG, CC ZOU Abstract Polysomy of the X chromosome is a very rare disorder, and little information is available in the literature. Tetrasomy X was first reported in 1961 and only approximately 60 cases have been reported. Herein, we reported a 5-year-old girl with tetrasomy X, who presented to our clinics because of "short stature". She was born to a G2P2 mother at 39 weeks of gestation with a birth weight of 3.5 kg. She started walking at 16 months of age, and speaking at 18 months. She had syndactyly in both hands and patent ductus arteriosus (0.7 cm), which were corrected by surgery soon after birth and at 7 months of age, respectively. She also had a history of epilepsy for 3 years with 4 episodes of convulsion but none in the past two years, and depakine was administered till now. She was apt to get pneumonia. She was 105 cm in height and 13 kg in weight, showing a coarse face with ocular hypertelorism and epicanthus. She presented with female external genitalia with Tanner I breast and external genitalia development. Her pelvic ultrasound showed immature uterus and ovarian. Intelligence quotient test revealed low intellectual functioning (IQ: 51). Cytogenetic investigation revealed a karyotype of 48,XXXX. These data showed that in females with intellectual disabilities, abnormal height, microcephaly, skeletal and limb anomalies, and congenital heart defects, 48,XXXX karyotype should be considered although it is an extremely rare entity. -

A New Case of Prenatally Diagnosed Pentasomy X: Review of the Literature
Hindawi Publishing Corporation Case Reports in Obstetrics and Gynecology Volume 2015, Article ID 935202, 5 pages http://dx.doi.org/10.1155/2015/935202 Case Report A New Case of Prenatally Diagnosed Pentasomy X: Review of the Literature Linda Maria Azzurra Pirollo,1 Leila Baghernajad Salehi,2 Simona Sarta,1 Marco Cassone,3 Maria Vittoria Capogna,1 Emilio Piccione,1 Giuseppe Novelli,4 and Adalgisa Pietropolli1 1 Section of Gynecology and Obstetrics, Academic Department of Biomedicine and Prevention and Clinical Department of Surgery, Tor Vergata University Hospital, Viale Oxford 81, 00133 Rome, Italy 2Laboratory of Medical Genetics, Polyclinic of Tor Vergata Foundation, Viale Oxford 81, 00133 Rome, Italy 3Laboratory of Medical Genetics, University of Rome Tor Vergata, Via Montpellier 1, 00133 Rome, Italy 4Genetics Section, Department of Biomedicine and Prevention, University of Rome Tor Vergata, Via Montpellier 1, 00133 Rome, Italy Correspondence should be addressed to Linda Maria Azzurra Pirollo; [email protected] Received 2 December 2014; Revised 13 January 2015; Accepted 14 January 2015 Academic Editor: Olivier Picone Copyright © 2015 Linda Maria Azzurra Pirollo et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Pentasomy X is a rare chromosomal abnormality probably due to a nondisjunction during the meiosis. Only four cases prenatally diagnosed were described until now. Our case is the fifth one prenatally diagnosed at 20 weeks of gestational age in a 39-years- old woman. She underwent invasive prenatal diagnosis for her advanced maternal age without any other known risk factor. -

Abstracts from the 53Rd European Society of Human Genetics (ESHG) Conference: E-Posters
European Journal of Human Genetics (2020) 28:798–1016 https://doi.org/10.1038/s41431-020-00741-5 ABSTRACTS COLLECTION Abstracts from the 53rd European Society of Human Genetics (ESHG) Conference: e-Posters © European Society of Human Genetics 2020. Modified from the conference website and published with permission 2020 Volume 28 | Supplement 1 Virtual Conference June 6-9, 2020 Sponsorship: Publication of this supplement was sponsored by the European Society of Human Genetics. All content was reviewed and approved by the ESHG Scientific Programme Committee, which held full responsibility for the abstract selections. 1234567890();,: 1234567890();,: Disclosure Information: In order to help readers form their own judgments of potential bias in published abstracts, authors are asked to declare any competing financial interests. Contributions of up to EUR 10 000.- (Ten thousand Euros, or equivalent value in kind) per year per company are considered “Modest”. Contributions above EUR 10 000.- per year are considered “Significant”. Presenting authors are indicated with bold typeface in the contributor lists. e-Posters improve the prevention and treatment of congenital malformations. E-P01 Reproductive Genetics/Prenatal Genetics Material and methods: The data from Medical Genetic Center Register was analyzing by the MedCalc 15.8 E-P01.07 program. Epidemiological monitoring of congenital malforma- Results: The incidence rate of congenital malformations tions in Yakutia from 2007 to 2018 over a 12-year period averaged 29.4 cases per 1000 newborns with a standard deviation of 2.9. It’s high A. I. Fedorov1, A. L. Sukhomyasova1,2, A. N. Sleptsov2,1,N. indicator In Russia (>20 ‰). At this period, the average R. -

The Type and Prevalence of Chromosomal Abnormalities in Couples
Journal of Gynecology Obstetrics and Human Reproduction 48 (2019) 521–525 Available online at ScienceDirect www.sciencedirect.com Original Article The type and prevalence of chromosomal abnormalities in couples with recurrent first trimester abortions: A Turkish retrospective study a, b a a Malik Ejder Yildirim *, Savas Karakus , Hande Kucuk Kurtulgan , Burak Baser , a Ilhan Sezgin a Cumhuriyet University, Faculty of Medicine, Department of Medical Genetics, Turkey b Cumhuriyet University, Faculty of Medicine, Department of Obstetrics and Gynecology, Turkey A R T I C L E I N F O A B S T R A C T Article history: Objective: Chromosomal abnormalities are more common in the first trimester abortions. We aimed to Received 8 March 2019 investigate the types and prevalence of chromosomal abnormalities in couples with recurrent first Received in revised form 2 May 2019 trimester miscarriages in Sivas, Turkey. Accepted 7 May 2019 Materials and medhods: Three hundred couples (600 individuals) who had a story of recurrent abortion Available online 11 May 2019 were included in the study. Chromosome analysis was performed after the preparation of lymphocyte culture with the standard method. Karyotype analyses were supported by FISH and aCGH studies. Keywords: Results: Total 26 chromosome abnormalities (8.7%) were found in the couples (19 females and 7 males). Recurrent abortion Fifteen cases (57.7%) were structural anomalies and eleven cases (42.3%) were numerical chromosomal Chromosomal abnormality Heterochromatin aberrations. We detected 5 balanced translocations (33.3%), 4 Robertsonian translocations (26.7%), 3 Satellite inversions (20%), 2 duplications (13.3%) and one deletion (6.7%) among the structural anomalies. -

A Case of 49,XXXXX in Which the Extra X Chromosomes Were Maternal in Origin Y G Cho, D S Kim, H S Lee, S C Cho, S I Choi
1004 CASE REPORT J Clin Pathol: first published as 10.1136/jcp.2004.017475 on 27 August 2004. Downloaded from A case of 49,XXXXX in which the extra X chromosomes were maternal in origin Y G Cho, D S Kim, H S Lee, S C Cho, S I Choi ............................................................................................................................... J Clin Pathol 2004;57:1004–1006. doi: 10.1136/jcp.2004.017475 the manufacturer’s instructions. Data were processed by This report describes an 11 month old female baby with GeneScanTM and GenotyperTM software (Applied Biosystems). features of pentasomy X. A molecular and cytogenetic The most typical features of this infant were muscular evaluation revealed that her karyotype was 49,XXXXX and hypotonia, mental retardation, and mild hydrocephalus as her extra X chromosomes were of maternal origin. She has a result of dilatation of both lateral ventricles. A magnetic muscular hypotonia, mental retardation, a cleft palate, mild resonance imaging scan of the brain was done to hydrocephalus as a result of dilatation of both lateral investigate the brain abnormalities, and showed dilatation ventricles, hyperextensible elbow joints, proximal radioulnar of both lateral ventricles combined with mild leucomalacia synostosis, clinodactyly of the fifth finger, valgus of the feet, in the periventricular area. and small hands and feet. In addition, she has a persistent The general appearance of the patient showed the typical pupillary membrane and congenital chorioretinal atrophy. dysmorphism of pentasomy X (fig 2). Characteristic cranio- The pathogenesis of pentasomy X is not clear at present, but it facial features, such as hypertelorism, a flat broad nose, cleft is thought to be caused by successive maternal non- palate, a persistent pupillary membrane, congenital chorio- dysjunctions.