The Type and Prevalence of Chromosomal Abnormalities in Couples
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The National Economic Burden of Rare Disease Study February 2021
Acknowledgements This study was sponsored by the EveryLife Foundation for Rare Diseases and made possible through the collaborative efforts of the national rare disease community and key stakeholders. The EveryLife Foundation thanks all those who shared their expertise and insights to provide invaluable input to the study including: the Lewin Group, the EveryLife Community Congress membership, the Technical Advisory Group for this study, leadership from the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH), the Undiagnosed Diseases Network (UDN), the Little Hercules Foundation, the Rare Disease Legislative Advocates (RDLA) Advisory Committee, SmithSolve, and our study funders. Most especially, we thank the members of our rare disease patient and caregiver community who participated in this effort and have helped to transform their lived experience into quantifiable data. LEWIN GROUP PROJECT STAFF Grace Yang, MPA, MA, Vice President Inna Cintina, PhD, Senior Consultant Matt Zhou, BS, Research Consultant Daniel Emont, MPH, Research Consultant Janice Lin, BS, Consultant Samuel Kallman, BA, BS, Research Consultant EVERYLIFE FOUNDATION PROJECT STAFF Annie Kennedy, BS, Chief of Policy and Advocacy Julia Jenkins, BA, Executive Director Jamie Sullivan, MPH, Director of Policy TECHNICAL ADVISORY GROUP Annie Kennedy, BS, Chief of Policy & Advocacy, EveryLife Foundation for Rare Diseases Anne Pariser, MD, Director, Office of Rare Diseases Research, National Center for Advancing Translational Sciences (NCATS), National Institutes of Health Elisabeth M. Oehrlein, PhD, MS, Senior Director, Research and Programs, National Health Council Christina Hartman, Senior Director of Advocacy, The Assistance Fund Kathleen Stratton, National Academies of Science, Engineering and Medicine (NASEM) Steve Silvestri, Director, Government Affairs, Neurocrine Biosciences Inc. -

Klinefelter Syndrome) at 9 Years of Age
17th SSBP International Research Symposium Developmental trajectories of behavioural phenotypes Programme Book 10–13 October 2014 • New York, USA 2 17th International SSBP Research Symposium The Society for the Study 3 of Behavioural Phenotypes 10th – 13th October 2014 The 17th SSBP International Meeting Developmental Trajectories of Behavioural Phenotypes New York, USA 10th – 13th October 2014, New York, USA Contents Contents Welcome ........................................................................................................................................................................................................9 New York Conference Organiser ..............................................................................................................................................10 Scientific Committee ..........................................................................................................................................................................11 4 The SSBP .......................................................................................................................................................................................................12 The SSBP Executive Committee : ...........................................................................................................................................................................12 Meetings of the SSBP ....................................................................................................................................................................................................13 -

Chromosome 18
Chromosome 18 Description Humans normally have 46 chromosomes in each cell, divided into 23 pairs. Two copies of chromosome 18, one copy inherited from each parent, form one of the pairs. Chromosome 18 spans about 78 million DNA building blocks (base pairs) and represents approximately 2.5 percent of the total DNA in cells. Identifying genes on each chromosome is an active area of genetic research. Because researchers use different approaches to predict the number of genes on each chromosome, the estimated number of genes varies. Chromosome 18 likely contains 200 to 300 genes that provide instructions for making proteins. These proteins perform a variety of different roles in the body. Health Conditions Related to Chromosomal Changes The following chromosomal conditions are associated with changes in the structure or number of copies of chromosome 18. Distal 18q deletion syndrome Distal 18q deletion syndrome occurs when a piece of the long (q) arm of chromosome 18 is missing. The term "distal" means that the missing piece (deletion) occurs near one end of the chromosome arm. The signs and symptoms of distal 18q deletion syndrome include delayed development and learning disabilities, short stature, weak muscle tone ( hypotonia), foot abnormalities, and a wide variety of other features. The deletion that causes distal 18q deletion syndrome can occur anywhere between a region called 18q21 and the end of the chromosome. The size of the deletion varies among affected individuals. The signs and symptoms of distal 18q deletion syndrome are thought to be related to the loss of multiple genes from this part of the long arm of chromosome 18. -

First Case Report of Maternal Mosaic Tetrasomy 9P Incidentally Detected on Non-Invasive Prenatal Testing
G C A T T A C G G C A T genes Article First Case Report of Maternal Mosaic Tetrasomy 9p Incidentally Detected on Non-Invasive Prenatal Testing Wendy Shu 1,*, Shirley S. W. Cheng 2 , Shuwen Xue 3, Lin Wai Chan 1, Sung Inda Soong 4, Anita Sik Yau Kan 5 , Sunny Wai Hung Cheung 6 and Kwong Wai Choy 3,* 1 Department of Obstetrics and Gynaecology, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong, China; [email protected] 2 Clinical Genetic Service, Hong Hong Children Hospital, Ngau Tau Kok, Hong Kong, China; [email protected] 3 Department of Obstetrics and Gynaecology, Chinese University of Hong Kong, Hong Kong, China; [email protected] 4 Department of Clinical Oncology, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong, China; [email protected] 5 Prenatal Diagnostic Laboratory, Tsan Yuk Hospital, Sai Ying Pun, Hong Kong, China; [email protected] 6 NIPT Department, NGS Lab, Xcelom Limited, Hong Kong, China; [email protected] * Correspondence: [email protected] (W.S.); [email protected] (K.W.C.); Tel.: +852-25-957-359 (W.S.); +852-35-053-099 (K.W.C.) Abstract: Tetrasomy 9p (ORPHA:3390) is a rare syndrome, hallmarked by growth retardation; psychomotor delay; mild to moderate intellectual disability; and a spectrum of skeletal, cardiac, renal and urogenital defects. Here we present a Chinese female with good past health who conceived her pregnancy naturally. Non-invasive prenatal testing (NIPT) showed multiple chromosomal aberrations were consistently detected in two sampling times, which included elevation in DNA from Citation: Shu, W.; Cheng, S.S.W.; chromosome 9p. -

Aneuploidy and Aneusomy of Chromosome 7 Detected by Fluorescence in Situ Hybridization Are Markers of Poor Prognosis in Prostate Cancer'
[CANCERRESEARCH54,3998-4002,August1, 19941 Advances in Brief Aneuploidy and Aneusomy of Chromosome 7 Detected by Fluorescence in Situ Hybridization Are Markers of Poor Prognosis in Prostate Cancer' Antonio Alcaraz, Satoru Takahashi, James A. Brown, John F. Herath, Erik J- Bergstralh, Jeffrey J. Larson-Keller, Michael M Lieber, and Robert B. Jenkins2 Depart,nent of Urology [A. A., S. T., J. A. B., M. M. U, Laboratory Medicine and Pathology (J. F. H., R. B. fl, and Section of Biostatistics (E. J. B., J. J. L-JCJ, Mayo Clinic and Foundation@ Rochester, Minnesota 55905 Abstract studies on prostate carcinoma samples. Interphase cytogenetic analy sis using FISH to enumerate chromosomes has the potential to over Fluorescence in situ hybridization is a new methodologj@which can be come many of the difficulties associated with traditional cytogenetic used to detect cytogenetic anomalies within interphase tumor cells. We studies. Previous studies from this institution have demonstrated that used this technique to identify nonrandom numeric chromosomal alter ations in tumor specimens from the poorest prognosis patients with path FISH analysis with chromosome enumeration probes is more sensitive ological stages T2N@M,Jand T3NOMOprostate carcinomas. Among 1368 than FCM for detecting aneuploid prostate cancers (4, 5, 7). patients treated by radical prostatectomy, 25 study patients were ascer We designed a case-control study to test the hypothesis that spe tamed who died most quickly from progressive prostate carcinoma within cific, nonrandom cytogenetic changes are present in tumors removed 3 years of diagnosis and surgery. Tumors from 25 control patients who from patients with prostate carcinomas with poorest prognoses . -

General Contribution
24 Abstracts of 37th Annual Meeting A1 A SCREENING METHOD FOR FRAGILE X MUTATION: DETECTION OF THE CGG REPEAT IN FMR-1 GENE BY PCR WITH BIOTIN-LABELED PRIMER. ..Eiji NANBA, Kousaku OHNO and Kenzo TAKESHITA Division of Child Neurology, Institute of Neurological Sciences, Tot- tori University School of Medicine. Yonago We have developed a new polymerase chain reaction(PCR)-based method for detection of the CGG repeat in FMR-1 gene. No specific product from PCR was detected on the gel with ethidium bromide staining, because 7-deaza-2'-dGTP is necessary for amplification of this repeat. Biotin-labeled primer was used for PCR and the product was transferred to a nylon membrane followed the detection of biotin by Smilight kit. The size of PCR product from normal control were slightly various and around 300bp. No PCR product was detected from 3 fragile X male patients in 2 families diagnosed by cytogenetic examination. This method is useful for genetic screen- ing of male mental retardation patients to exclude the fragile X mutation. A2 DNA ANALYSISFOR FRAGILE X SYNDROME Osamu KOSUDA,Utak00GASA, ~.ideynki INH, a~ji K/NAGIJCltI, and Kazumasa ]tIKIJI (SILL Inc., Tokyo) Fragile X syndrome is X-linked disease having the amplification of (CG6)n repeat sequence in the chromsomeXq27.3. We performed Southern blot analysis using three probes recognized repetitive sequence resion. Normal controle showed 5.2Kb with Eco RI digest and 2.7Kb with Eco RI/Bss ttII digest as the germ tines by the Southern blot analysis. However, three cell lines established fro~ unrelated the patients with fragile X showed the abnormal bands between 5.2 and 7.7Kb with Eco RI digest, and between 2.7 and 7.7Kb with Eco aI/Bss HII digest. -

Tetrasomy 9P Syndrome in a Filipino Infant
CASE REPORT Tetrasomy 9p Syndrome in a Filipino Infant Ebner Bon G. Maceda,1,2 Erena S. Kasahara,3 Edsel Allan G. Salonga,2 Myrian R. Dela Cruz2 and Leniza De Castro-Hamoy1,2 1Division of Clinical Genetics, Department of Pediatrics, College of Medicine and Philippine General Hospital, University of the Philippines Manila 2Institute of Human Genetics, National Institutes of Health, University of the Philippines Manila 3Division of Newborn Medicine, Department of Pediatrics, College of Medicine and Philippine General Hospital, University of the Philippines Manila ABSTRACT Tetrasomy 9p syndrome is a rare chromosomal abnormality syndrome whose most common features include hypertelorism, malformed ears, bulbous nose and microretrognathia. These features present as a result of an additional two copies of the short arm of chromosome 9. Here we present a neonate with characteristic facial features of hypertelorism, downslanted palpebral fissure, bulbous nose, small cupped ears, cleft lip and palate, and downturned corners of the mouth. Clinical features were consistent with the cytogenetic analysis of tetrasomy 9p. In general, clinicians are not as familiar with the features of tetrasomy 9p syndrome as that of more common chromosomal abnormalities like trisomies 13, 18, and 21. Hence, this case re-emphasizes the importance of doing the standard karyotyping for patients presenting with multiple congenital anomalies. Also, this is the first reported case of Tetrasomy 9p syndrome in Filipinos. Key Words: Tetrasomy 9p, isochromosome, hypertelorism, bulbous nose INTRODUCTION Tetrasomy 9p is a broad term used to describe the presence of a supernumerary chromosome of the short arm of chromosome 9. In more specific terms, the presence of 2 extra copies of 9p arms can be either isodicentric or pseudodicentric. -

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic -

XXXXX Syndrome
XXXXX Syndrome 49,XXXXX (pentasomy X) is a rare sex chromosome aneu- 2. Craniofacial features ploidy. The birth prevalence of pentasomy X is estimated to be a. Microcephaly 1 in 85,000 females. b. Flattened occiput c. Epicanthus d. Upslanting palpebral fissures GENETICS/BASIC DEFECTS e. Ocular hypertelorism 1. Etiology: Three extra X chromosomes are responsible for f. Uncoordinated eye movements the pentasomy X syndrome. g. Flat broad nose 2. Occurrence of a 49,XXXXX complement: secondary to h. Cleft palate sequential non-disjunctions in meiosis I and meiosis II in i. Low-set ears the mother j. Malformed teeth a. Involves the survival of both X chromosomes in a sin- 3. Skeletal abnormalities gle oocytes through both meiotic divisions a. Short neck i. Once between homologous X chromosomes at b. Lax joints the first meiosis c. Multiple dislocations ii. Twice between sister chromatids in both X chro- i. Shoulders mosomes in the secondary oocytes at the second ii. Elbows meiosis iii. Hips b. Followed by the fertilization by a sperm contributing d. Radioulnar synostosis the 5th chromosome X e. Spinal abnormalities 3. Formation of four Barr bodies f. Clinodactyly of the 5th fingers a. Lyon hypothesis g. Lower leg abnormalities i. Inactivation of all X chromosomes but one i. Genu valgus ii. Account for the viability of the X-chromosome ii. Talipes aneuploidies iii. Metatarsus varus b. Inactivation of four X chromosomes resulting in four h. Delayed bone age Barr bodies 4. Congenital heart defects 4. Effect of supernumerary X chromosomes: a direct rela- a. Ventricular septal defect tionship between the number of supernumerary X chro- b. -

Cytogenetics, Chromosomal Genetics
Cytogenetics Chromosomal Genetics Sophie Dahoun Service de Génétique Médicale, HUG Geneva, Switzerland [email protected] Training Course in Sexual and Reproductive Health Research Geneva 2010 Cytogenetics is the branch of genetics that correlates the structure, number, and behaviour of chromosomes with heredity and diseases Conventional cytogenetics Molecular cytogenetics Molecular Biology I. Karyotype Definition Chromosomal Banding Resolution limits Nomenclature The metaphasic chromosome telomeres p arm q arm G-banded Human Karyotype Tjio & Levan 1956 Karyotype: The characterization of the chromosomal complement of an individual's cell, including number, form, and size of the chromosomes. A photomicrograph of chromosomes arranged according to a standard classification. A chromosome banding pattern is comprised of alternating light and dark stripes, or bands, that appear along its length after being stained with a dye. A unique banding pattern is used to identify each chromosome Chromosome banding techniques and staining Giemsa has become the most commonly used stain in cytogenetic analysis. Most G-banding techniques require pretreating the chromosomes with a proteolytic enzyme such as trypsin. G- banding preferentially stains the regions of DNA that are rich in adenine and thymine. R-banding involves pretreating cells with a hot salt solution that denatures DNA that is rich in adenine and thymine. The chromosomes are then stained with Giemsa. C-banding stains areas of heterochromatin, which are tightly packed and contain -
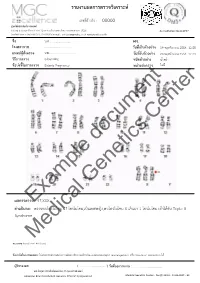
Example Document Medical Genetics Center
รายงานผลการตรวจววเคราะหย เลขทธรออางอนง : 00000 ศผนยยพวนธธศาสตรยการแพทยย 6/6 หมนม 6 ถนนสสขาภนบาล 5 ซอย 32 แขวงออเงนน เขตสายไหม กรสงเทพมหานคร 10220 Accreditation No.4148/57 โทรศกพทย/โทรสาร 086-8861203, 02-7920726 e-mail : [email protected] www.genetics.co.th ชชชอ น.ส............................. HN. ............. โรงพยาบาล .................................... ววนททชเกกบตววอยยาง 19 พฤศจนกายน 2558 12:55 แพทยยผผผสวชงตรวจ นพ.................................... ววนททชรวบตววอยยาง 20 พฤศจนกายน 2558 12:43 ววธทการตรวจ G-banding ชนวดตววอยยาง นนนาครรนา ขผอบยงชทชในการตรวจ Elderly Pregnancy หนยวยสยงตรวจ ไมมมธ Center document Genetics ผลการตรวจExample: 47,XXX คคาอธวบาย : ตรวจพบโครโมโซม 47 โครโมโซม,เปปนเพศหญนง,พบโครโมโซม X เกนนมา 1 โครโมโซม เขอาไดอกกบ Triple X Syndrome Medical หมายเหตธ: Band level 450 band ขผอจคากวดในการทดสอบ: ไมมสามารถตรวจสอบความผนดปกตนขนาดเลลกชนนด submicroscopic rearrangement หรรอ low-level mosaicism ไดอ ผผผรวบรองผล ( .................................. ) ววนททชออกรายงาน : ....................................... นพ.วทรยธทธ ประพวนธยพจนย,พบ.,วว.กธมารเวชศาสตรย American Board of Medical Genetics (Clinical Cytogenetics) Medical Genetics Center : Fo-QP-19/01 : 16-03-2015 : 02 เรียน อ.นพ...................................... ที่นับถือ ตามที่ผลตรวจโครโมโซมจากน ้าคร่้าของ นส........................ (HN .............., Lab no. ..............) พบ โครโมโซม X เกินมา 1 โครโมโซมนั น ความผิดปกติดังกล่าว เข้าได้กับกลุ่มอาการ trisomy X หรือ triple X syndrome ซึ่งเป็นความผิดปกติของโครโมโซมเพศที่พบได้บ่อยในทารกเพศหญิง โดยความผิดปกติของ โครโมโซมแบบนี -
Inside This Issue
Winter 2014 No. 77 Inside this issue Group News | Fundraising | Members’ Letters | One Family Living with Two Different Chromosome Disorders | Bristol Conference 2014 | Unique Leaflets | Christmas Card Order Form Sophie, Unique’s Chair of Trustees Dear Members, In the past month a few things have reminded me of why it is so important to make connections through Unique but also to draw support from other parents around us. I’ve just returned from Unique’s most recent family conference in Bristol where 150 of us parents and carers had a lovely time in workshops, meals and activities, chatting and watching our children milling around together like one big family since – although we had never met before – we have shared so many experiences in common. However in contrast I have also just met a new mum who has just moved to my area from far away with two toddlers, one with a rare joys of the internet, it is becoming easier to meet others with similar, chromosome disorder, who is starting from scratch with no even very rare, chromosome disorders around the world and to find professional, medical or social support. She reminds me of how yourself talking to them in the middle of the night about some lonely I felt when Max was newly diagnosed, when I knew no one interesting things our children share in common (obsession with with a disabled child let alone anyone with a rare chromosome catalogues, anyone?) And of course we also have an enormous disorder. Elsewhere our latest Unique Facebook group, Unique amount in common with so many parents of children with other Russia, is also just starting up – so far it includes just a small special needs or disabilities around us in our own communities who number of members sharing very different experiences to mine here will often be walking the same path as us.