Thoracoscopy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Point of the Needle. Occult Pneumothorax: a Review P Gilligan, D Hegarty, T B Hassan
293 CASE REPORTS Emerg Med J: first published as 10.1136/emj.20.3.296 on 1 May 2003. Downloaded from The point of the needle. Occult pneumothorax: a review P Gilligan, D Hegarty, T B Hassan ............................................................................................................................. Emerg Med J 2003;20:293–296 maximal resonance, which was the left sixth intercostal space The case of a patient with an unusual medical condition in the anterior axillary line. Some 300 ml of air was aspirated and an occult pneumothorax is presented. The evidence from the left hemithorax and the patient clinically improved. for management of occult pneumothorax particularly in The chest radiograph revealed bilateral infiltrates and under- patients with underlying lung disease is reviewed and solu- lying cystic and bullous disease but failed to reveal evidence of tions to the acute clinical problems that may arise are a pneumothorax (fig 1). A chest radiograph performed after suggested. the needle decompression also failed to show a pneumotho- rax. Computed tomography (CT) of the thorax revealed an anterior pneumothorax (fig 2). This was drained under CT guidance by the placement of a chest drain catheter. 27 year old man with histiocytosis X presented to the During the patient’s in hospital stay his chest drain was emergency department with left posterior chest wall removed as his chest radiograph showed no evidence of Apain and marked dyspnoea. The patient previously had residual pneumothorax. The patient became markedly dysp- recurrent pneumothoraces, eight on the right and two on the noeic within 24 hours. Because of the clinical impression of left. He had undergone pleurodesis of the right lung. -

Thoracoscopy for Spontaneous Pneumothorax
Journal of Clinical Medicine Review Thoracoscopy for Spontaneous Pneumothorax José M. Porcel 1,2,3,* and Pyng Lee 4 1 Pleural Medicine Unit, Department of Internal Medicine, Hospital Universitari Arnau de Vilanova, 25198 Lleida, Spain 2 Institut de Recerca Biomèdica de Lleida Fundació Dr. Pifarré, IRBLleida, 25198 Lleida, Spain 3 School of Medicine, Universitat de Lleida, 25008 Lleida, Spain 4 Division of Respiratory and Critical Care Medicine, The National University Hospital, Singapore 119228, Singapore; [email protected] * Correspondence: [email protected] Abstract: Video-assisted thoracic surgery (VATS) is the treatment of choice for recurrence preven- tion in patients with spontaneous pneumothorax (SP). Although the optimal surgical technique is uncertain, bullous resection using staplers in combination with mechanical pleurodesis, chemical pleurodesis and/or staple line coverage is usually undertaken. Currently, patient satisfaction, post- operative pain and other perioperative parameters have significantly improved with advancements in thoracoscopic technology, which include uniportal, needlescopic and nonintubated VATS variants. Ipsilateral recurrences after VATS occur in less than 5% of patients, in which case a redo-VATS is a feasible therapeutical option. Randomized controlled trials are urgently needed to shed light on the best definitive management of SP. Keywords: thoracoscopy; VATS; spontaneous pneumothorax; bullectomy; pleurodesis Citation: Porcel, J.M.; Lee, P. Thoracoscopy for Spontaneous 1. Introduction Pneumothorax. J. Clin. Med. 2021, 10, Pneumothorax can occur spontaneously or because of trauma or procedural compli- 3835. https://doi.org/10.3390/ cation. Spontaneous pneumothoraces (SP) are divided into primary (PSP) and secondary jcm10173835 (SSP). PSP occurs in someone without a known underlying lung disease, whereas SPP appears as a complication of an underlying lung disease, such as chronic obstructive pul- Academic Editors: Paola Ciriaco and Robert Hallifax monary disease, lung cancer, interstitial lung disease, or tuberculosis. -

Nonintubated Thoracoscopic Surgery Using Regional Anesthesia and Vagal Block and Targeted Sedation
Original Article Nonintubated thoracoscopic surgery using regional anesthesia and vagal block and targeted sedation Ke-Cheng Chen1,2, Ya-Jung Cheng3, Ming-Hui Hung3, Yu-Ding Tseng1, Jin-Shing Chen1,2 1Department of Surgery, National Taiwan University Hospital Yun-Lin Branch, Yun-Lin County, Taiwan; 2Division of Thoracic Surgery, Department of Surgery, National Taiwan University Hospital and National Taiwan University College of Medicine, Taipei, Taiwan; 3Department of Anesthesiology, National Taiwan University Hospital and National Taiwan University College of Medicine, Taipei, Taiwan Corresponding to: Dr. Jin-Shing Chen. Department of Surgery, National Taiwan University Hospital, No. 7, Chung Shan South Road, Taipei, Taiwan. Email: [email protected]. Objective: Thoracoscopic surgery without endotracheal intubation is a novel technique for diagnosis and treatment of thoracic diseases. This study reported the experience of nonintubated thoracoscopic surgery in a tertiary medical center in Taiwan. Methods: From August 2009 through August 2013, 446 consecutive patients with lung or pleural diseases were treated by nonintubated thoracoscopic surgery. Regional anesthesia was achieved by thoracic epidural anesthesia or internal intercostal blockade. Targeted sedation was performed with propofol infusion to achieve a bispectral index value between 40 and 60. The demographic data and clinical outcomes were evaluated by retrospective chart review. Results: Thoracic epidural anesthesia was used in 290 patients (65.0%) while internal intercostal blockade was used in 156 patients (35.0%). The final diagnosis were primary lung cancer in 263 patients (59.0%), metastatic lung cancer in 38 (8.5%), benign lung tumor in 140 (31.4%), and pneumothorax in 5 (1.1%). The median anesthetic induction time was 30 minutes by thoracic epidural anesthesia and was 10 minutes by internal intercostal blockade. -
The Method of Medical Thoracoscopy 2Nd Edition
® THE METHOD OF MEDICAL THORACOSCOPY 2nd Edition Ralf HEINE Jan Hendrik BARTELS Christian WEISS THE METHOD OF MEDICAL THORACOSCOPY 2nd Edition Ralf HEINE, MD Jan Hendrik BARTELS, MD Christian WEISS Medical Clinic III – Pneumonology, Hematology-Oncology and Palliative Medicine Hospital of St. Elisabeth and St. Barbara Halle (Saale), Germany 4 The Method of Medical Thoracoscopy Cover image: The Method of Medical Thoracoscopy Andreas Heine 2nd Edition Ralf Heine, MD Jan Hendrik Bartels, MD Christian Weiss Medical Clinic III – Pneumonology, Hematology-Oncology and Palliative Medicine, Hospital of St. Elisabeth and St. Barbara, Halle (Saale), Germany Correspondence address of the author: Dr. med. Ralf Heine Facharzt für Innere Medizin, Pneumologie Important notes: und Notfallmedizin Medical knowledge is ever changing. As new research and clinical Chefarzt der Medizinischen Klinik III – Pneumologie, experience broaden our knowledge, changes in treat ment and therapy Häma tologie-Onkologie und Palliativmedizin may be required. The authors and editors of the material herein Krankenhaus St. Elisabeth und St. Barbara, Halle/Saale have consulted sources believed to be reliable in their efforts to provide information that is complete and in accord with the Mauerstr. 5 standards accept ed at the time of publication. However, in view of 06110 Halle/Saale, Germany the possibili ty of human error by the authors, editors, or publisher, or changes in medical knowledge, neither the authors, editors, All rights reserved. publisher, nor any other party who has been involved in the prepara- nd | st tion of this booklet, warrants that the information contained herein is 2 edition 1 edition 2007 in every respect accurate or complete, and they are not responsible © 2015 GmbH for any errors or omissions or for the results obtained from use of P.O. -
Answer Key Chapter 1
Instructor's Guide AC210610: Basic CPT/HCPCS Exercises Page 1 of 101 Answer Key Chapter 1 Introduction to Clinical Coding 1.1: Self-Assessment Exercise 1. The patient is seen as an outpatient for a bilateral mammogram. CPT Code: 77055-50 Note that the description for code 77055 is for a unilateral (one side) mammogram. 77056 is the correct code for a bilateral mammogram. Use of modifier -50 for bilateral is not appropriate when CPT code descriptions differentiate between unilateral and bilateral. 2. Physician performs a closed manipulation of a medial malleolus fracture—left ankle. CPT Code: 27766-LT The code represents an open treatment of the fracture, but the physician performed a closed manipulation. Correct code: 27762-LT 3. Surgeon performs a cystourethroscopy with dilation of a urethral stricture. CPT Code: 52341 The documentation states that it was a urethral stricture, but the CPT code identifies treatment of ureteral stricture. Correct code: 52281 4. The operative report states that the physician performed Strabismus surgery, requiring resection of the medial rectus muscle. CPT Code: 67314 The CPT code selection is for resection of one vertical muscle, but the medial rectus muscle is horizontal. Correct code: 67311 5. The chiropractor documents that he performed osteopathic manipulation on the neck and back (lumbar/thoracic). CPT Code: 98925 Note in the paragraph before code 98925, the body regions are identified. The neck would be the cervical region; the thoracic and lumbar regions are identified separately. Therefore, three body regions are identified. Correct code: 98926 Instructor's Guide AC210610: Basic CPT/HCPCS Exercises Page 2 of 101 6. -

Endoscopy Matrix
Endoscopy Matrix CPT Description of Endoscopy Diagnostic Therapeutic Code (Surgical) 31231 Nasal endoscopy, diagnostic, unilateral or bilateral (separate procedure) X 31233 Nasal/sinus endoscopy, diagnostic with maxillary sinusoscopy (via X inferior meatus or canine fossa puncture) 31235 Nasal/sinus endoscopy, diagnostic with sphenoid sinusoscopy (via X puncture of sphenoidal face or cannulation of ostium) 31237 Nasal/sinus endoscopy, surgical; with biopsy, polypectomy or X debridement (separate procedure) 31238 Nasal/sinus endoscopy, surgical; with control of hemorrhage X 31239 Nasal/sinus endoscopy, surgical; with dacryocystorhinostomy X 31240 Nasal/sinus endoscopy, surgical; with concha bullosa resection X 31241 Nasal/sinus endoscopy, surgical; with ligation of sphenopalatine artery X 31253 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including frontal sinus exploration, with removal of tissue from frontal sinus, when performed 31254 Nasal/sinus endoscopy, surgical; with ethmoidectomy, partial (anterior) X 31255 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior 31256 Nasal/sinus endoscopy, surgical; with maxillary antrostomy X 31257 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy 31259 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy, with removal of tissue from the sphenoid sinus 31267 Nasal/sinus endoscopy, surgical; with removal of -

Local Anaesthetic Thoracoscopy Information for Patients
Oxford Centre for Respiratory Medicine Local Anaesthetic Thoracoscopy Information for patients Provisional appointment date and time……...............................…. Important information about your thoracoscopy • Do not eat or drink anything for 6 hours before your procedure. You can take any medicines you need to have with a sip of water up until 2 hours before your procedure. • Tell your doctor about all the medication you take and any medical conditions you have. • Tell us if you are on any blood thinning or diabetes medications – these are normally stopped before your procedure. It is important that you continue to take any other medications (including those for high blood pressure). • Bring enough belongings for a five night stay in hospital – please do not bring in any valuables. • If your doctor tells you that you are likely to go home the same day, please arrange for someone to bring you in and take you home from the thoracoscopy. You should also not be alone overnight after your thoracoscopy. For 24 hours after the thoracoscopy you cannot drive, return to work, operate machinery, drink alcohol, sign legal documents or be responsible for small children. • Contact your doctor if you are short of breath or having increasing chest pain. Page 2 What is a thoracoscopy? A thoracoscopy is an examination of the pleural cavity (the space between your lung and chest wall) with a special camera called a thoracoscope. This allows us to learn more about your illness and the cause of the fluid or air in your chest. Lining of lung (lined by pleural membranes) Lung Ribs Fluid (pleural effusion) or air (pneumothorax) in the pleural space/cavity around the lung Inside of chest wall (lined by pleural membranes) During the thoracoscopy, the doctor can also take small samples (called biopsies) from the pleural membranes on the inside of your chest and drain any fluid that has collected there. -
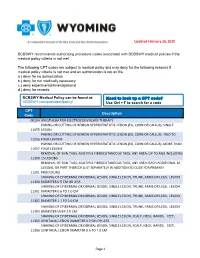
CPT Code Description 00104 ANESTHESIA FOR
Updated February 20, 2020 BCBSWY recommends authorizing procedure codes associated with BCBSWY medical policies if the medical policy criteria is not met. The following CPT codes are subject to medical policy and may deny for the following reasons if medical policy criteria is not met and an authorization is not on file: a.) deny for no authorization b.) deny for not medically necessary c.) deny experimental/investigational d.) deny for records BCBSWY Medical Policy can be found at: Need to look up a CPT code? BCBSWY.com/providers/policy/ Use Ctrl + F to search for a code CPT Description Code 00104 ANESTHESIA FOR ELECTROCONVULSIVE THERAPY PARING OR CUTTING OF BENIGN HYPERKERATOTIC LESION (EG, CORN OR CALLUS); SINGLE 11055 LESION PARING OR CUTTING OF BENIGN HYPERKERATOTIC LESION (EG, CORN OR CALLUS); TWO TO 11056 FOUR LESIONS PARING OR CUTTING OF BENIGN HYPERKERATOTIC LESION (EG, CORN OR CALLUS); MORE THAN 11057 FOUR LESIONS REMOVAL OF SKIN TAGS, MULTIPLE FIBROCUTANEOUS TAGS, ANY AREA; UP TO AND INCLUDING 11200 15 LESIONS REMOVAL OF SKIN TAGS, MULTIPLE FIBROCUTANEOUS TAGS, ANY AREA; EACH ADDITIONAL 10 LESIONS, OR PART THEREOF (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY 11201 PROCEDURE) SHAVING OF EPIDERMAL OR DERMAL LESION, SINGLE LESION, TRUNK, ARMS OR LEGS; LESION 11300 DIAMETER 0.5 CM OR LESS SHAVING OF EPIDERMAL OR DERMAL LESION, SINGLE LESION, TRUNK, ARMS OR LEGS; LESION 11301 DIAMETER 0.6 TO 1.0 CM SHAVING OF EPIDERMAL OR DERMAL LESION, SINGLE LESION, TRUNK, ARMS OR LEGS; LESION 11302 DIAMETER 1.1 TO 2.0 CM SHAVING OF EPIDERMAL -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Anesthesia for Video-Assisted Thoracoscopic Surgery
23 Anesthesia for Video-Assisted Thoracoscopic Surgery Edmond Cohen Historical Considerations of Video-Assisted Thoracoscopy ....................................... 331 Medical Thoracoscopy ................................................................................................. 332 Surgical Thoracoscopy ................................................................................................. 332 Anesthetic Management ............................................................................................... 334 Postoperative Pain Management .................................................................................. 338 Clinical Case Discussion .............................................................................................. 339 Key Points Jacobaeus Thoracoscopy, the introduction of an illuminated tube through a small incision made between the ribs, was • Limited options to treat hypoxemia during one-lung venti- first used in 1910 for the treatment of tuberculosis. In 1882 lation (OLV) compared to open thoracotomy. Continuous the tubercle bacillus was discovered by Koch, and Forlanini positive airway pressure (CPAP) interferes with surgi- observed that tuberculous cavities collapsed and healed after cal exposure during video-assisted thoracoscopic surgery patients developed a spontaneous pneumothorax. The tech- (VATS). nique of injecting approximately 200 cc of air under pressure • Priority on rapid and complete lung collapse. to create an artificial pneumothorax became a widely used • Possibility -

Cosmetic and Reconstructive Procedures Corporate Medical Policy
Cosmetic and Reconstructive Procedures Corporate Medical Policy File Name: Cosmetic and Reconstructive Procedures File Code: UM.SURG.02 Origination: 06/2016 Last Review: 01/2020 Next Review: 01/2021 Effective Date: 04/01/2020 Description/Summary The term, “cosmetic and reconstructive procedures” includes procedures ranging from purely cosmetic to purely reconstructive. Benefit application has the potential to be confusing to members because there is an area of overlap where cosmetic procedures may have a reconstructive component and reconstructive procedures may have a cosmetic component. These procedures are categorized and benefits are authorized based upon the fundamental purpose of the procedure. The American Medical Association and the American Society of Plastic Surgeons have agreed upon the following definitions: • Cosmetic procedures are those that are performed to reshape normal structures of the body in order to improve the patient’s appearance and self- esteem. • Reconstructive procedures are those procedures performed on abnormal structures of the body, caused by congenital defects, developmental abnormalities, trauma, infection, tumors or disease. It is generally performed to improve function but may also be done to approximate a normal appearance. In order to be considered medically necessary, the goal of reconstructive surgery must be to correct an abnormality in order to restore physiological function to the extent possible. As such, for reconstructive surgery to be considered medically necessary there must be a reasonable -

Hemodynamic Response to Thoracoscopy and Thoracotomy
Physiol. Res. 59: 363-371, 2010 Hemodynamic Response to Thoracoscopy and Thoracotomy S. TRČA1, Z. KRŠKA1, O. KITTNAR2, M. MLČEK2, R. DEMEŠ1, V. DANZIG3, S. ŠIMEK3, J. BRUTHANS4, R. FRAŠKO1 1First Surgical Department, Clinical Department of Abdominal, Thoracic Surgery and Traumatology of the First Faculty of Medicine and General Teaching Hospital, Charles University, Prague, 2Institute of Physiology, First Faculty of Medicine, Charles University, Prague, 3Second Medical Department, Clinical Department of Cardiology and Angiology, First Faculty of Medicine and General Teaching Hospital, Charles University, Prague, 4Department of Anesthesiology and Resuscitation, First Faculty of Medicine and General Teaching Hospital, Charles University, Prague, Czech Republic Received January 23, 2009 Accepted June 3, 2009 On-line August 12, 2009 Summary Key words Operations in the pleural cavity are connected with circulatory Hemodynamics • Pulmonary circulation • Thoracoscopy • changes in pulmonary circulation and general changes of Thoracotomy hemodynamics. These changes are influenced by the position of patient’s body on the operation table and by the introduction of Corresponding author artificial pneumothorax. Thoracoscopy is an advanced surgical Otomar Kittnar, Institute of Physiology, 1st Medical Faculty, approach in thoracic surgery, but its hemodynamic effect is still Charles University, Albertov 5, 128 00 Prague 2, Czech Republic. not known. The aim of the present study was to compare the E-mail: [email protected] hemodynamic response to surgeries carried out by open (thoracotomy – TT) and closed (thoracoscopy – TS) surgical approach. Thirty-eight patients have been monitored throughout Introduction the operation – from the introduction of anesthesia to completing the surgery. Monitored parameters were systolic blood pressure There are numerous reports about hemodynamic (BPs), diastolic blood pressure (BPd), O2 saturation (SaO2), changes during the operation in pleural cavity (Hill et al.