Psychosocial Adaptation to Pregnancy Regina Lederman • Karen Weis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Humour of Homer
The Humour of Homer Samuel Butler A lecture delivered at the Working Men's College, Great Ormond Street 30th January, 1892 The first of the two great poems commonly ascribed to Homer is called the Iliad|a title which we may be sure was not given it by the author. It professes to treat of a quarrel between Agamemnon and Achilles that broke out while the Greeks were besieging the city of Troy, and it does, indeed, deal largely with the consequences of this quarrel; whether, however, the ostensible subject did not conceal another that was nearer the poet's heart| I mean the last days, death, and burial of Hector|is a point that I cannot determine. Nor yet can I determine how much of the Iliadas we now have it is by Homer, and how much by a later writer or writers. This is a very vexed question, but I myself believe the Iliadto be entirely by a single poet. The second poem commonly ascribed to the same author is called the Odyssey. It deals with the adventures of Ulysses during his ten years of wandering after Troy had fallen. These two works have of late years been believed to be by different authors. The Iliadis now generally held to be the older work by some one or two hundred years. The leading ideas of the Iliadare love, war, and plunder, though this last is less insisted on than the other two. The key-note is struck with a woman's charms, and a quarrel among men for their possession. -

OH-00143; Aaron C. Kane and Sarah Taylor Kane
Transcript of OH-00143 Aaron C. Kane and Sarah Taylor Kane Interviewed by John Wearmouth on February 19, 1988 Accession #: 2006.034; OH-00143 Transcribed by Shannon Neal on 10/15/2020 Southern Maryland Studies Center College of Southern Maryland Phone: (301) 934-7626 8730 Mitchell Road, P.O. Box 910 E-mail: [email protected] La Plata, MD 20646 Website: csmd.edu/smsc The Stories of Southern Maryland Oral History Transcription Project has been made possible in part by a major grant from the National Endowment for the Humanities (NEH): Stories of Southern Maryland. https://www.neh.gov/ Any views, findings, conclusions, or recommendations expressed in this transcription, do not necessarily represent those of the National Endowment for the Humanities. Format Interview available as MP3 file or WAV: ssoh00143 (1:34:59) Content Disclaimer The Southern Maryland Studies Center offers public access to transcripts of oral histories and other archival materials that provide historical evidence and are products of their particular times. These may contain offensive language, negative stereotypes or graphic descriptions of past events that do not represent the opinions of the College of Southern Maryland or the Southern Maryland Studies Center. Typographic Note • [Inaudible] is used when a word cannot be understood. • Brackets are used when the transcriber is not sure about a word or part of a word, to add a note indicating a non-verbal sound and to add clarifying information. • Em Dash — is used to indicate an interruption or false start. • Ellipses … is used to indicate a natural extended pause in speech Subjects African American teachers Depressions Education Education, Higher Middle school principals School integration Segregation in education Tags Depression, 1929 Music teacher Aaron C. -

Which of the Following Signposts Was Featured in the Passage? Contrasts & Contradictions Aha Moment Tough Questions Words Of
Whitney’s face lit up when she saw me climb aboard the bus. “Right here, Lexi! You can sit beside me! I’ll even give you Which of the following signposts the window seat.” 1A I raised my eyebrows in surprise. “Um… okay!” I said as I was featured in the passage? plopped down in the seat beside Whitney. I had been dreading this new 45-minute bus ride ever since my parents announced Contrasts & Contradictions that we would be moving to an acreage outside of town. I knew Whitney rode this bus, but she and I had never been the best Aha Moment of friends. We just didn’t have that much in common. Whitney Tough Questions had been wearing makeup and flirting with boys since she was Words of the Wiser eight years old. I, on the other hand, had no interest in covering my face in a rainbow of colors. Furthermore, I only Again & Again ever talked to boys about our favorite sports teams, and I Memory Moment was a bit uncomfortable even doing that. “Hey, I had a question about math, Lex. Do you mind helping me?” she asked. “No, of course not,” I answered. She peeked inside her backpack. “Oh, I guess I forgot my math book at school. Do you have yours?” 1B I unzipped my backpack and dug out my math book, open- ing to our assignment. “Which part did you need help with?” “Actually, I think I can figure it out. Maybe I’ll just copy down your answers, and then when I’m doing my assignment Answer the question that follows later, I can check my answers against yours to just to make the signpost you identified. -

A Mix Methods Evaluation of the Effectiveness of a Group-Based Prenatal Yoga Programme on Perceived Stress in Pregnant Women
A mix methods evaluation of the effectiveness of a group-based prenatal yoga programme on perceived stress in pregnant women Zehra Baykal Akmese ( [email protected] ) Ege Universitesi https://orcid.org/0000-0002-4753-2421 Sezer Er Güneri Ege Universitesi Research article Keywords: Yoga, Pregnancy, Pregnant women, General Adaptation Syndrome, Relaxation, Perceived Stress Posted Date: September 15th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-48031/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/22 Abstract Background Yoga is recommended as a behavioural self-management strategy for stress. However, the evidence of how it affects women's stress perception is not much studied. Hence the present study was taken to assess the perceived stress score and to explore the experiences of pregnant women of stress management before and after prenatal yoga programme according to Selye's General Adaptation Syndrome Theory. Methods This study was made using concurrent triangulation mixed method design. Quantitative part of the study was made pretest-posttest with control group experimental study, qualitative part of the study was made phenomenological method. Quantitative data were gathered from 31 pregnant women in both yoga and control groups. As for qualitative data, 21 and 15 pregnant women were interviewed in the rst and second interviews, respectively. Pregnant Woman Description Form was used as a data collection tool; a visual analogue scale was used for measuring stress score; and the interviews were made through Semi- Structured Interview Form. The themes were determined according to the stages of Selye's General Adaptation Syndrome Theory. -

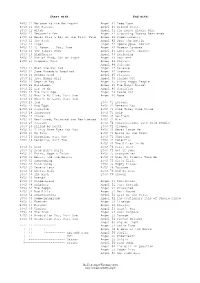
Songs by Title
Songs by Title Title Artist Title Artist #1 Goldfrapp (Medley) Can't Help Falling Elvis Presley John Legend In Love Nelly (Medley) It's Now Or Never Elvis Presley Pharrell Ft Kanye West (Medley) One Night Elvis Presley Skye Sweetnam (Medley) Rock & Roll Mike Denver Skye Sweetnam Christmas Tinchy Stryder Ft N Dubz (Medley) Such A Night Elvis Presley #1 Crush Garbage (Medley) Surrender Elvis Presley #1 Enemy Chipmunks Ft Daisy Dares (Medley) Suspicion Elvis Presley You (Medley) Teddy Bear Elvis Presley Daisy Dares You & (Olivia) Lost And Turned Whispers Chipmunk Out #1 Spot (TH) Ludacris (You Gotta) Fight For Your Richard Cheese #9 Dream John Lennon Right (To Party) & All That Jazz Catherine Zeta Jones +1 (Workout Mix) Martin Solveig & Sam White & Get Away Esquires 007 (Shanty Town) Desmond Dekker & I Ciara 03 Bonnie & Clyde Jay Z Ft Beyonce & I Am Telling You Im Not Jennifer Hudson Going 1 3 Dog Night & I Love Her Beatles Backstreet Boys & I Love You So Elvis Presley Chorus Line Hirley Bassey Creed Perry Como Faith Hill & If I Had Teddy Pendergrass HearSay & It Stoned Me Van Morrison Mary J Blige Ft U2 & Our Feelings Babyface Metallica & She Said Lucas Prata Tammy Wynette Ft George Jones & She Was Talking Heads Tyrese & So It Goes Billy Joel U2 & Still Reba McEntire U2 Ft Mary J Blige & The Angels Sing Barry Manilow 1 & 1 Robert Miles & The Beat Goes On Whispers 1 000 Times A Day Patty Loveless & The Cradle Will Rock Van Halen 1 2 I Love You Clay Walker & The Crowd Goes Wild Mark Wills 1 2 Step Ciara Ft Missy Elliott & The Grass Wont Pay -

Academic Excellence … Personal Growth … Small School Environment Roadrunner
Building New Opportunities A publication of Sedona Charter School Enrichment Specials K-8 Tuition-free Montessori School Classrooms Without Walls Writing: SCS Staff and GC members Welcome to the Snack Shack! Photos: SCS Staff and parents The Suzuki Philosophy Design & Editing: Jane Cathcart Sights From Our Old-Fashioned Picnic academic excellence … personal growth … small school environment Roadrunner We want to take the opportunity to thank Patrons only concert in February, and you will receive 2 free tickets and reserved our parents, students and staff for working Our strings program is unique in around all of our construction these past seating at our winter and spring concerts in that we incorporate the tenets of several months. While not ideal, we are all the 2018-2019 school year. Suzuki Philosophy into our methods of doing our best to enjoy this new progress And for those of you who may have a teaching stringed instruments. In despite the inconveniences it may cause. tendency to worry, please don’t! The sharing the origins of the We are happy to announce that our tiny playground will be rebuilt across the parking philosophy and its basic principles, home for teacher KC O’Connor was lot as soon as the workers complete the we hope to help you and your completed in September and KC is Performing Arts Classroom. It is their final children progress through their enjoying her new home. Thanks to job on campus and the final piece of the musical journey. everyone who worked on the new deck and puzzle to get campus life “back to normal.” Dr. -

Guardian Consumerism in Twentieth Century America Mark Vandriel University of South Carolina
University of South Carolina Scholar Commons Theses and Dissertations 2017 Buy for the Sake of your Baby: Guardian Consumerism in Twentieth Century America Mark VanDriel University of South Carolina Follow this and additional works at: https://scholarcommons.sc.edu/etd Part of the History Commons Recommended Citation VanDriel, M.(2017). Buy for the Sake of your Baby: Guardian Consumerism in Twentieth Century America. (Doctoral dissertation). Retrieved from https://scholarcommons.sc.edu/etd/4226 This Open Access Dissertation is brought to you by Scholar Commons. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of Scholar Commons. For more information, please contact [email protected]. BUY FOR THE SAKE OF YOUR BABY: GUARDIAN CONSUMERISM IN TWENTIETH CENTURY AMERICA by Mark VanDriel Bachelor of Arts University of Northern Colorado, 2009 Submitted in Partial Fulfillment of the Requirements For the Degree of Doctor of Philosophy in History College of Arts and Sciences University of South Carolina 2017 Accepted by: Marjorie J. Spruill, Major Professor Kent Germany, Committee Member Deanne Messias, Committee Member Joseph November, Committee Member Cheryl L. Addy, Vice Provost and Dean of the Graduate School © Copyright by Mark VanDriel, 2017 All Rights Reserved. ii DEDICATION To Eliana VanDriel iii ACKNOWLEDGEMENTS I was introduced to the study of history by taking on the major as a transfer student to a new university with the intention of finishing a program in a single academic year. The condensed nature of this program blessed me by intense introductions to passionate historians who shared their craft with me. Steven Seegel, Aaron Haberman, Joan Clinefelter, and Marshall Clough at the University of Northern Colorado were magnificent inspirations and educators. -

Mary Anne Radmacher
May your walls know joy, may every room hold laughter, and every window open to great possibility. -- Mary Anne Radmacher (From Lauri’s front yard) The older I get the faster the year goes. Where did this year go? Oh, yes, it’s been a unique and crazy one! Who would have thought we would be living through a pandemic? I was thinking about the word “JOY.” Each year we put up huge sign in our front yard that spells out the word JOY. It twinkles with lights and is one of my favorite decorations to put up every year. I will admit it has been harder for me to find JOY over the last few months. I know many who are or have been sick with COVID-19 and two in our circle have lost their life to COVID over the last month. What is Joy? The definition of JOY according by the Webster Dictionary: 1a: the emotion evoked by well-being, success, or good fortune or by the prospect of possessing what one desires: DELIGHT b: the expression or exhibition of such emotion: GAIETY 2: a state of happiness or felicity: BLISS 3: a source or cause of delight Robert Holden, Ph.D., with The Happiness Project, recognizes these “5 Qualities of Joyful People.” “Do You Recognize These Qualities in Yourself?” 1. JOY IS CONSTANT When people tune in to the feeling of joy, what often emerges is an awareness that this joy is somehow always with us. Joy is quietly, invisibly ever-present. It is not “out there,” and it is not “in here”; rather, it is simply everywhere we are. -

Prenatal Attachment: a Developmental Model Helen Mck
Int. J. Prenatal and Perinatal Psychology and Medicine Vol. 20 (2008) No. 1/2, pp. 20–28 Prenatal Attachment: A Developmental Model Helen McK. Doan and Anona Zimerman Abstract: The attachment relationship between a pregnant woman and her developing fetus has been demonstrated to be of importance because of the potential link between prenatal attachment and parental behaviour both before and after birth (Condon & Corkindale, 1997; Pollock & Percy, 1999). While there is consistent evidence of individual differences in the level of attachment (Doan & Zimerman, 2002), there is still a need to clarify the factors that may help to explain this variation in scores. Over the past few years, our research has examined a number of cognitive, emotional and situational factors that relate to the level of prenatal attachment (Doan & Zimerman, 2003, 2006). While we have examined the effects of many factors on prenatal attachment, the two variables that most consistently related to the level of prenatal attachment are empathy and the cognitive ability to mentally represent the fetus. Against the backdrop of current research literature, we will propose an integrative framework that takes into account the linkages between empathy and cognition as a means for enlarging our understanding of the complexities of prenatal attachment. Zusammenfassung: Die Bindungsbeziehung zwischen einer Schwangeren und ihrem sich entwickelnden Kind hat sich wegen des moglichen¨ Bezuges zur vorgeburtlichen Bindungs- beziehung und elterlichem Verhalten vor und nach der Geburt als bedeutsam erwiesen (Condon & Corkindale, 1997; Pollock & Percy, 1999). W¨ahrend es eine verl¨assliche Evi- denz fur¨ individuelle Unterschiede in der Bindungsbeziehung gibt, ist es noch notwendig die Faktoren zu kl¨aren, die diese Unterschiede erkl¨aren konnen.¨ In den vergangenen Jahren hat unsere Forschung eine Anzahl von kognitiven, emotionalen und situativen Faktoren uberpr¨ uft,¨ die einen Bezug zum Grad der vorgeburtlichen Bindung haben (Doan & Zimer- man, 2003, 2006). -

BBO Orientation Packet
ACADEMY OF CANINE BEHAVIOR Basic Behavior and Obedience Class Orientation: FOCUS: Conditioning Markers. 1. Your dog will never take responsibility for getting trained. You must take the responsibility for educating your dog. This means that you must also take the responsibility of learning to communicate with your dog. Without communication there can be no education. 2. In the canine world there are no such things as equals; you will either lead or follow. A dog’s reasoning ability is similar to that of a two-year old child. A two-year old child does not make an effective leader; you must be the leader. 3. Every time you interact with your dog, they are learning something. If you are not teaching them the right behavior, they are learning the wrong behavior. 4. Negative attention is still attention. If the only way your dog can get your attention is be being bad, you will train them to act bad for attention. Remember to always reward your dog for good behavior. Pay attention when they are doing something right and let them know you like that behavior. 5. The consistency of your dog’s behavior, good or bad, will mirror the consistency of your training. If you train your dog by repeating the command ten times, you can expect the dog to respond 10% of the time. 6. A dog’s concept of right and wrong are very different from ours. Do not expect the dog to know what you may think is right or wrong. 7. If you are correcting the dog, are you certain the dog understand why it is being corrected? Have you educated and then generalized the concept? 8. -
Buffy & Angel Watching Order
Start with: End with: BtVS 11 Welcome to the Hellmouth Angel 41 Deep Down BtVS 11 The Harvest Angel 41 Ground State BtVS 11 Witch Angel 41 The House Always Wins BtVS 11 Teacher's Pet Angel 41 Slouching Toward Bethlehem BtVS 12 Never Kill a Boy on the First Date Angel 42 Supersymmetry BtVS 12 The Pack Angel 42 Spin the Bottle BtVS 12 Angel Angel 42 Apocalypse, Nowish BtVS 12 I, Robot... You, Jane Angel 42 Habeas Corpses BtVS 13 The Puppet Show Angel 43 Long Day's Journey BtVS 13 Nightmares Angel 43 Awakening BtVS 13 Out of Mind, Out of Sight Angel 43 Soulless BtVS 13 Prophecy Girl Angel 44 Calvary Angel 44 Salvage BtVS 21 When She Was Bad Angel 44 Release BtVS 21 Some Assembly Required Angel 44 Orpheus BtVS 21 School Hard Angel 45 Players BtVS 21 Inca Mummy Girl Angel 45 Inside Out BtVS 22 Reptile Boy Angel 45 Shiny Happy People BtVS 22 Halloween Angel 45 The Magic Bullet BtVS 22 Lie to Me Angel 46 Sacrifice BtVS 22 The Dark Age Angel 46 Peace Out BtVS 23 What's My Line, Part One Angel 46 Home BtVS 23 What's My Line, Part Two BtVS 23 Ted BtVS 71 Lessons BtVS 23 Bad Eggs BtVS 71 Beneath You BtVS 24 Surprise BtVS 71 Same Time, Same Place BtVS 24 Innocence BtVS 71 Help BtVS 24 Phases BtVS 72 Selfless BtVS 24 Bewitched, Bothered and Bewildered BtVS 72 Him BtVS 25 Passion BtVS 72 Conversations with Dead People BtVS 25 Killed by Death BtVS 72 Sleeper BtVS 25 I Only Have Eyes for You BtVS 73 Never Leave Me BtVS 25 Go Fish BtVS 73 Bring on the Night BtVS 26 Becoming, Part One BtVS 73 Showtime BtVS 26 Becoming, Part Two BtVS 74 Potential BtVS 74 -

The Importance of Multidisciplinary Management During Prenatal Care for Cleft Lip and Palate
The Importance of Multidisciplinary Management during Prenatal Care for Cleft Lip and Palate Hyun Ho Han1, Eun Jeong Choi1, Ji Min Kim1, Jong Chul Shin2, Jong Won Rhie1 Departments of 1Plastic and Reconstructive Surgery and 2Obstetrics and Gynecology, College of Medicine, The Catholic University of Korea, Original Article Seoul, Korea Background The prenatal ultrasound detection of cleft lip with or without cleft palate (CL/P) Correspondence: Jong Won Rhie and its continuous management in the prenatal, perinatal, and postnatal periods using a multi- Department of Plastic and Reconstructive Surgery, College of disciplinary team approach can be beneficial for parents and their infants. In this report, we Medicine, The Catholic University of share our experiences with the prenatal detection of CL/P and the multidisciplinary management Korea, 222 Banpo-daero, Seocho-gu, of this malformation in our institution’s Congenital Disease Center. Seoul 06591, Korea Methods The multidisciplinary team of the Congenital Disease Center for mothers of children Tel: +82-2-2258-6142 Fax: +82-2-594-7230 with CL/P is composed of obstetricians, plastic and reconstructive surgeons, pediatricians, and E-mail: [email protected] psychiatrists. A total of 11 fetuses were diagnosed with CL/P from March 2009 to December 2013, and their mothers were referred to the Congenital Disease Center of our hospital. When CL/P is suspected in the prenatal ultrasound screening examination, the pregnant woman is referred to our center for further evaluation. Results The abortion rate was 28% (3/11). The concordance rate of the sonographic and final diagnoses was 100%. Ten women (91%) reported that they were satisfied with the multidisci- plinary management in our center.