Benzodiazepines: a Review of Research Results, 1980
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guaiana, G., Barbui, C., Caldwell, DM, Davies, SJC, Furukawa, TA
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Explore Bristol Research Guaiana, G., Barbui, C., Caldwell, D. M., Davies, S. J. C., Furukawa, T. A., Imai, H., ... Cipriani, A. (2017). Antidepressants, benzodiazepines and azapirones for panic disorder in adults: a network meta-analysis. Cochrane Database of Systematic Reviews, 2017(7), [CD012729]. https://doi.org/10.1002/14651858.CD012729 Publisher's PDF, also known as Version of record Link to published version (if available): 10.1002/14651858.CD012729 Link to publication record in Explore Bristol Research PDF-document This is the final published version of the article (version of record). It first appeared online via Cochrane Library at https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012729/full . Please refer to any applicable terms of use of the publisher. University of Bristol - Explore Bristol Research General rights This document is made available in accordance with publisher policies. Please cite only the published version using the reference above. Full terms of use are available: http://www.bristol.ac.uk/pure/about/ebr-terms Cochrane Database of Systematic Reviews Antidepressants, benzodiazepines and azapirones for panic disorder in adults: a network meta-analysis (Protocol) Guaiana G, Barbui C, Caldwell DM, Davies SJC, Furukawa TA, Imai H, Koesters M, Tajika A, Bighelli I, Pompoli A, Cipriani A Guaiana G, Barbui C, Caldwell DM, Davies SJC, Furukawa TA, Imai H, Koesters M, Tajika A, Bighelli I, Pompoli A, Cipriani A. Antidepressants, benzodiazepines and azapirones for panic disorder in adults: a network meta-analysis. Cochrane Database of Systematic Reviews 2017, Issue 7. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Effect of Diazepam and Fosazepam (A Soluble Derivative of Diazepam) on Sleep in Man A.N
Br. J. clin. Pharmac. (1976), 3, 533-541 EFFECT OF DIAZEPAM AND FOSAZEPAM (A SOLUBLE DERIVATIVE OF DIAZEPAM) ON SLEEP IN MAN A.N. NICHOLSON, BARBARA M. STONE & CORAL H. CLARKE Royal Air Force Institute of Aviation Medicine, Farnborough, Hampshire 1 The effect of diazepam (5 mg and 10 mg), and fosazepam (60 mg and 80 mg), a soluble derivative of diazepam, on sleep was studied in six healthy adult males using electroencephalography for sleep measures, and analogue scales for subjective assessments of well-being and sleep quality. The effect of diazepam was limited to the night of ingestion, but the effect of fosazepam was carried over to the next night and so modified sleep for about 30 h after ingestion. 2 Effects on total sleep time were limited to the night of ingestion. There were increases with diazepam (10 mg) (P = 0.05), and with fosazepam (60 mg and 80 mg) (P = 0.001). For the night of ingestion sleep onset latencies were shortened, and awakenings were reduced by both drugs. The latency to stage 3 was shortened by fosazepam (60 mg and 80 mg) (P = 0.05). 3 The low and high dose of each drug reduced the duration (min) of stage 0 sleep (P = 0.01), but fosazepam also reduced the duration (min) of stage 1 sleep (P = 0.001), and there was an increase in stage 2 sleep (P = 0.01). With fosazepam there were carry over effects to the next night with reduction of stage 1 sleep (P = 0.05). There were no effects on the duration of stage 3, but there was evidence that stage 4 activity was reduced during the recovery night after ingestion of fosazepam (80 mg). -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -

APO-NITRAZEPAM Nitrazepam Tablets BP 5 Mg, 10 Mg
PRODUCT MONOGRAPH APO-NITRAZEPAM Nitrazepam Tablets BP 5 mg, 10 mg Hypnotic and Anticonvulsant APOTEX INC. DATE OF REVISION: 150 Signet Drive February 9, 2010 Weston, Ontario M9L 1T9 Control No: 133454 Page 1 of 21 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION....................................................... 3 SUMMARY PRODUCT INFORMATION.............................................................................. 3 INDICATIONS AND CLINICAL USE ................................................................................... 3 CONTRAINDICATIONS......................................................................................................... 3 WARNINGS AND PRECAUTIONS ....................................................................................... 3 ADVERSE REACTIONS ......................................................................................................... 7 DRUG INTERACTIONS.......................................................................................................... 7 DOSAGE AND ADMINISTRATION ..................................................................................... 8 OVERDOSAGE........................................................................................................................ 8 ACTION AND CLINICAL PHARMACOLOGY.................................................................... 9 STORAGE AND STABILITY ............................................................................................... 10 DOSAGE FORMS, COMPOSITION AND PACKAGING.................................................. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -
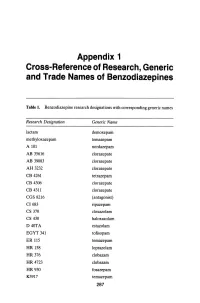
Appendix 1 Cross-Reference of Research, Generic and Trade Names of Benzodiazepines
Appendix 1 Cross-Reference of Research, Generic and Trade Names of Benzodiazepines Table 1. Benzodiazepine research designations with corresponding generic names Research Designation Generic Name lactam demoxepam methyloxazepam temazepam A 101 nordazepam AB 35616 clorazepate AB 39083 clorazepate AH 3232 clorazepate CB 4261 tetrazepam CB 4306 clorazepate CB 4311 clorazepate CGS 8216 (antagonist) CI683 ripazepam CS 370 cloxazolam CS 430 haloxazolam D40TA estazolam EGYT 341 tofisopam ER 115 temazepam HR 158 loprazolam HR376 clobazam HR 4723 clobazam HR930 fosazepam K3917 temazepam 287 THE BENZODIAZEPINES Research Designation Generic Name LA 111 diazepam LM 2717 clobazam ORF 8063 triflubazam Ro 4-5360 nitrazepam Ro 5-0690 chlordiazepoxide Ro 5-0883 desmethy1chlordiazepoxide Ro 5-2092 demoxepam Ro 5-2180 desmethyldiazepam Ro 5-2807 diazepam Ro 5-2925 desmethylmedazepam Ro 5-3059 nitrazepam Ro 5-3350 bromazepam Ro 5-3438 fludiazepam Ro 5-4023 clonazepam Ro 5-4200 flunitrazepam Ro 5-4556 medazepam Ro 5-5345 temazepam Ro 5-6789 oxazepam Ro 5-6901 flurazepam Ro 15-1788 (antagonist) Ro 21-3981 midazolam RU 31158 loprazolam S 1530 nimetazepam SAH 1123 isoquinazepam SAH 47603 temazepam SB 5833 camazepam SCH 12041 halazepam SCH 16134 quazepam U 28774 ketazolam U 31889 alprazolam U 33030 triazolam W4020 prazepam We 352 triflubazam 288 RESEARCH, GENERIC AND TRADE NAMES Research Designation Generic Name We 941 brotizolam Wy 2917 temazepam Wy 3467 diazepam Wy 3498 oxazepam Wy 3917 temazepam Wy 4036 lorazepam Wy 4082 lormetazepam Wy 4426 oxazepam Y 6047 -

List of Benzodiazepines - Wikipedia, the Free Encyclopedia
List of benzodiazepines - Wikipedia, the free encyclopedia Log in / create account Article Talk Read Edit Our updated Terms of Use will become effective on May 25, 2012. Find out more. List of benzodiazepines From Wikipedia, the free encyclopedia Main page The below tables contain a list of benzodiazepines that Benzodiazepines Contents are commonly prescribed, with their basic pharmacological Featured content characteristics such as half-life and equivalent doses to other Current events benzodiazepines also listed, along with their trade names and Random article primary uses. The elimination half-life is how long it takes for Donate to Wikipedia half of the drug to be eliminated by the body. "Time to peak" Interaction refers to when maximum levels of the drug in the blood occur Help after a given dose. Benzodiazepines generally share the About Wikipedia same pharmacological properties, such as anxiolytic, Community portal sedative, hypnotic, skeletal muscle relaxant, amnesic and Recent changes anticonvulsant (hypertension in combination with other anti The core structure of benzodiazepines. Contact Wikipedia hypertension medications). Variation in potency of certain "R" labels denote common locations of effects may exist among individual benzodiazepines. Some side chains, which give different Toolbox benzodiazepines produce active metabolites. Active benzodiazepines their unique properties. Print/export metabolites are produced when a person's body metabolizes Benzodiazepine the drug into compounds that share a similar pharmacological -

Harmonized Tariff Schedule of the United States (2004) -- Supplement 1 Annotated for Statistical Reporting Purposes
Harmonized Tariff Schedule of the United States (2004) -- Supplement 1 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2004) -- Supplement 1 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABACAVIR 136470-78-5 ACEXAMIC ACID 57-08-9 ABAFUNGIN 129639-79-8 ACICLOVIR 59277-89-3 ABAMECTIN 65195-55-3 ACIFRAN 72420-38-3 ABANOQUIL 90402-40-7 ACIPIMOX 51037-30-0 ABARELIX 183552-38-7 ACITAZANOLAST 114607-46-4 ABCIXIMAB 143653-53-6 ACITEMATE 101197-99-3 ABECARNIL 111841-85-1 ACITRETIN 55079-83-9 ABIRATERONE 154229-19-3 ACIVICIN 42228-92-2 ABITESARTAN 137882-98-5 ACLANTATE 39633-62-0 ABLUKAST 96566-25-5 ACLARUBICIN 57576-44-0 ABUNIDAZOLE 91017-58-2 ACLATONIUM NAPADISILATE 55077-30-0 ACADESINE 2627-69-2 ACODAZOLE 79152-85-5 ACAMPROSATE 77337-76-9 ACONIAZIDE 13410-86-1 ACAPRAZINE 55485-20-6 ACOXATRINE 748-44-7 ACARBOSE 56180-94-0 ACREOZAST 123548-56-1 ACEBROCHOL 514-50-1 ACRIDOREX 47487-22-9 ACEBURIC ACID 26976-72-7 -

Marrakesh Agreement Establishing the World Trade Organization
No. 31874 Multilateral Marrakesh Agreement establishing the World Trade Organ ization (with final act, annexes and protocol). Concluded at Marrakesh on 15 April 1994 Authentic texts: English, French and Spanish. Registered by the Director-General of the World Trade Organization, acting on behalf of the Parties, on 1 June 1995. Multilat ral Accord de Marrakech instituant l©Organisation mondiale du commerce (avec acte final, annexes et protocole). Conclu Marrakech le 15 avril 1994 Textes authentiques : anglais, français et espagnol. Enregistré par le Directeur général de l'Organisation mondiale du com merce, agissant au nom des Parties, le 1er juin 1995. Vol. 1867, 1-31874 4_________United Nations — Treaty Series • Nations Unies — Recueil des Traités 1995 Table of contents Table des matières Indice [Volume 1867] FINAL ACT EMBODYING THE RESULTS OF THE URUGUAY ROUND OF MULTILATERAL TRADE NEGOTIATIONS ACTE FINAL REPRENANT LES RESULTATS DES NEGOCIATIONS COMMERCIALES MULTILATERALES DU CYCLE D©URUGUAY ACTA FINAL EN QUE SE INCORPOR N LOS RESULTADOS DE LA RONDA URUGUAY DE NEGOCIACIONES COMERCIALES MULTILATERALES SIGNATURES - SIGNATURES - FIRMAS MINISTERIAL DECISIONS, DECLARATIONS AND UNDERSTANDING DECISIONS, DECLARATIONS ET MEMORANDUM D©ACCORD MINISTERIELS DECISIONES, DECLARACIONES Y ENTEND MIENTO MINISTERIALES MARRAKESH AGREEMENT ESTABLISHING THE WORLD TRADE ORGANIZATION ACCORD DE MARRAKECH INSTITUANT L©ORGANISATION MONDIALE DU COMMERCE ACUERDO DE MARRAKECH POR EL QUE SE ESTABLECE LA ORGANIZACI N MUND1AL DEL COMERCIO ANNEX 1 ANNEXE 1 ANEXO 1 ANNEX -
Nitrazepam: Lastingly Effective but Trouble on Withdrawal
1558 BRITISH MEDICAL JOURNAL 26 JUNE 1976 References I Chaturvedi, N C, et al, British Heart Journal, 1974, 36, 533. 1u Restieaux, N, et al, Lancet, 1967, 1, 1285. Harpur, J E, et al, Lancet, 1971, 2, 1331. 11 Thompson, P, and Sloman, G, British Medical journal, 1971, 4, 136. 2 Royston, G R, British Heart3Journal, 1972, 34, 526. 1' Grace, W J, and Yarvote, P M, Chest, 1971, 59, 15. Br Med J: first published as 10.1136/bmj.1.6025.1558 on 26 June 1976. Downloaded from 3 Moyer, J B, Hiller, G I, and Detroit, M, American Heart Journal, 1951, 13 Reynell, P C, British Heart Journal, 1975, 37, 166. 41, 340. 14 Soler, N G, et al, Groden, B M, Allison, A, and Shaw, G B, Scottish Medical,Journal, 1967, Lancet, 1974, 1, 475. 12, 435. Ia Bradley, R F, and Bryfogle, J W, American J7ournal of Medicine, 1956, 5 Adgey, A A J, British Heart Journal, 1969, 31, 750. 20, 207. 6 Hutter, A M, et al, New England Journal of Medicine, 1973, 288, 1141. LB Partamian, J 0, and Bradley, R F, New EnglandJournal of Medicine, 1965, 7 Tucker, H H, et al, British Medical Journal, 1973, 1, 10. 273, 455. I Hayes, M J, Morris, G K, and Hampton, J R, British Heart Journal, 17 Harrower, A D B, and Clarke, B F, British Medical Jrournal, 1976, 1, 1974, 36, 395. 126. Nitrazepam: lastingly effective but trouble on withdrawal KIRSTINE ADAM, LIISI ADAMSON, VLASTA BREZINOVA, WILLIAM M HUNTER, IAN OSWALD British MedicallJournal, 1976, 1, 1558-1560 Methods Ten volunteers, with the agreement of their general practitioners, Summary took part in this study of nitrazepam 5 mg nightly.