Plasmodium Knowlesi
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Plate Tectonics and Seismic Activities in Sabah Area
Plate Tectonics and Seismic Activities in Sabah Area Kuei-hsiang CHENG* Kao Yuan University, 1821 Zhongshan Road, Luzhu District, Kaohsiung, Taiwan. *Corresponding author: [email protected]; Tel: 886-7-6077750; Fax: 886-7-6077762 A b s t r a c t Received: 27 November 2015 Ever since the Pliocene which was 1.6 million years ago, the structural Revised: 25 December 2015 geology of Sabah is already formed; it is mainly influenced by the early Accepted: 7 January 2016 South China Sea Plate, which is subducted into the Sunda Plate. However, In press: 8 January 2016 since the Cenozoic, the Sunda Plate is mainly influenced by the western and Online: 1 April 2016 southern of the Sunda-Java Arc and Trench system, and the eastern side of Luzon Arc and Trench system which has an overall impact on the tectonic Keywords: and seismic activity of Sunda plate. Despite the increasing tectonic activities Arc and Trench System, of Sunda-Java Arc and Trench System, and of Luzon Arc and Trench Tectonic earthquake, Seismic System since the Quaternary, which cause many large and frequent zoning, GM(1,1)model, earthquakes. One particular big earthquake is the M9.0 one in Indian Ocean Seismic potential assessment in 2004, leading to more than two hundred and ninety thousand deaths or missing by the tsunami caused by the earthquake. As for Borneo island which is located in residual arc, the impact of tectonic earthquake is trivial; on the other hand, the Celebes Sea which belongs to the back-arc basin is influenced by the collision of small plates, North Sulawesi, which leads to two M≧7 earthquakes (1996 M7.9 and 1999 M7.1) in the 20th century. -

M.V. Solita's Passage Notes
M.V. SOLITA’S PASSAGE NOTES SABAH BORNEO, MALAYSIA Updated August 2014 1 CONTENTS General comments Visas 4 Access to overseas funds 4 Phone and Internet 4 Weather 5 Navigation 5 Geographical Observations 6 Flags 10 Town information Kota Kinabalu 11 Sandakan 22 Tawau 25 Kudat 27 Labuan 31 Sabah Rivers Kinabatangan 34 Klias 37 Tadian 39 Pura Pura 40 Maraup 41 Anchorages 42 2 Sabah is one of the 13 Malaysian states and with Sarawak, lies on the northern side of the island of Borneo, between the Sulu and South China Seas. Sabah and Sarawak cover the northern coast of the island. The lower two‐thirds of Borneo is Kalimantan, which belongs to Indonesia. The area has a fascinating history, and probably because it is on one of the main trade routes through South East Asia, Borneo has had many masters. Sabah and Sarawak were incorporated into the Federation of Malaysia in 1963 and Malaysia is now regarded a safe and orderly Islamic country. Sabah has a diverse ethnic population of just over 3 million people with 32 recognised ethnic groups. The largest of these is the Malays (these include the many different cultural groups that originally existed in their own homeland within Sabah), Chinese and “non‐official immigrants” (mainly Filipino and Indonesian). In recent centuries piracy was common here, but it is now generally considered relatively safe for cruising. However, the nearby islands of Southern Philippines have had some problems with militant fundamentalist Muslim groups – there have been riots and violence on Mindanao and the Tawi Tawi Islands and isolated episodes of kidnapping of people from Sabah in the past 10 years or so. -

Plasmodium Vivax Population Structure and Transmission Dynamics in Sabah Malaysia
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Charles Darwin University's Institutional Digital Repository Plasmodium vivax Population Structure and Transmission Dynamics in Sabah Malaysia Noor Rain Abdullah1, Bridget E. Barber2,3, Timothy William2,4, Nor Azrina Norahmad1,Umi Rubiah Satsu1, Prem Kumar Muniandy1, Zakiah Ismail1, Matthew J. Grigg2,3, Jenarun Jelip4, Kim Piera3, Lorenz von Seidlein3, Tsin W. Yeo3, Nicholas M. Anstey3,5, Ric N. Price3,5,6, Sarah Auburn3* 1 Herbal Medicine Research Centre, Institute for Medical Research, Kuala Lumpar, Malaysia, 2 Infectious Diseases Unit, Queen Elizabeth Hospital, Kota Kinabalu, Sabah, Malaysia, 3 Global and Tropical Health Division, Menzies School of Health Research and Charles Darwin University, Darwin, Australia, 4 Sabah Department of Health, Kota Kinabalu, Sabah, Malaysia, 5 Division of Medicine, Royal Darwin Hospital, Darwin, Australia, 6 Centre for Tropical Medicine, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, United Kingdom Abstract Despite significant progress in the control of malaria in Malaysia, the complex transmission dynamics of P. vivax continue to challenge national efforts to achieve elimination. To assess the impact of ongoing interventions on P. vivax transmission dynamics in Sabah, we genotyped 9 short tandem repeat markers in a total of 97 isolates (8 recurrences) from across Sabah, with a focus on two districts, Kota Marudu (KM, n = 24) and Kota Kinabalu (KK, n = 21), over a 2 year period. STRUCTURE analysis on the Sabah-wide dataset demonstrated multiple sub-populations. Significant differentiation (FST = 0.243) was observed between KM and KK, located just 130 Km apart. -

Study on the Transportation System in the East Coast of Sabah
International Journal of Recent Technology and Engineering (IJRTE) ISSN: 2277-3878, Volume-9 Issue-4, November 2020 Study on the Transportation System in the East Coast of Sabah Mohd Azizul Bin Ladin, Fariq Ismeth Jaimin, Nazaruddin Abdul Taha, Lillian Gungat, Abdul Karim Mirasa, Sidah Binti Idris Abstract: Being situated in eastern Malaysia, Sabah is one of be divided into two areas, urban and rural. Within the urban the states which have a firm economic foundation through areas of Sabah, the road networks are better, and some types agriculture, forestry as well as petroleum industries. However, of public transportation, although unreliable, are available for even though it is rich with the natural resources that have long the public. However, like other urban road networks in the served for the country’s economic growth, as a whole, Sabah is considered a little behind her counterparts in the Peninsular world, it faces its main adversary, the road congestion. This Malaysia in terms of infrastructure and development. This study causes pollution and harm to the environment as well as the mainly examines the transportation network in Semporna, Tawau health of the citizens within the area. Moving on to the rural and Lahad Datu which is mostly in poor condition. This is side of Sabah, congestion is not a serious issue as the road because it is extensively used for the industrial activities including network in the area is not connected enough to even create logging, palm industries and quarries. Based on the survey, it is road congestion. The sight of gravel roads, mud path, and found that the road mostly had potholes, edge raveling, uneven surfaces, road rutting, congestion problems and limited parking potholes are the norm. -

The Study on Development for Enhancing Rural Women Entrepreneurs in Sabah, Malaysia
No. MINISTRY OF AGRICULTURE JAPAN INTERNATIONAL AND FOOD INDUSTRY COOPERATION AGENCY SABAH, MALAYSIA THE STUDY ON DEVELOPMENT FOR ENHANCING RURAL WOMEN ENTREPRENEURS IN SABAH, MALAYSIA FINAL REPORT VOLUME II FEBRUARY 2004 KRI INTERNATIONAL CORP. AFA JR 04-13 THE STUDY ON DEVELOPMENT FOR ENHANCING RURAL WOMEN ENTREPRENEURS IN SABAH, MALAYSIA FINAL REPORT AND SUPPORTING BOOKS MAIN REPORT FINAL REPORT VOLUME I - MASTER PLAN - FINAL REPORT VOLUME II - SITUATION ANALYSIS AND VERIFICATION SURVEY - PUANDESA DATABOOK PUANDESA GUIDELINE FOR RURAL WOMEN ENTREPRENEURS - HOW TO START A MICRO BUSINESS IN YOUR COMMUNITY - EXCHANGE RATE (as of 30 December 2003) US$1.00 = RM3.8= Yen107.15 LOCATION MAP PUANDESA THE STUDY ON DEVELOPMENT FOR ENHANCING RURAL WOMEN ENTREPRENEURS IN SABAH, MALAYSIA FINAL REPORT CONTENTS LOCATION MAP PART I: SITUATION ANALYSIS CHAPTER 1: STUDY OUTLINE ..........................................................................................................1 1.1 BACKGROUND .........................................................................................................................1 1.2 OBJECTIVE OF THE STUDY....................................................................................................2 1.3 TARGET GROUP OF THE STUDY ...........................................................................................2 1.4 MAJOR ACTIVITIES AND TIME-FRAME...............................................................................2 1.5 NICKNAME OF THE STUDY ...................................................................................................6 -

Vector Compositions Change Across Forested to Deforested Ecotones in Emerging Areas of Zoonotic Malaria Transmission in Malaysia
Vector compositions change across forested to deforested ecotones in emerging areas of zoonotic malaria transmission in Malaysia Frances M. Hawkes1, Benny O. Manin1, Amanda Cooper, Sylvia Daim, Rahman Homathevi, Jenarun Jelip, Tanrang Husin, and Tock H. Chua* *Corresponding author; Telephone: +60126029046; Email: [email protected], [email protected] 1These first authors contributed equally to this article. Author affiliations Natural Resources Institute, University of Greenwich at Medway, Chatham Maritime, Kent, ME4 4TB, UK Frances M. Hawkes Universiti Malaysia Sabah, Kota Kinabalu, Sabah, 88400 Malaysia Benny O. Manin, Sylvia Daim, Rahman Homathevi, Tock H. Chua Royal Botanic Gardens Kew, Richmond, London, TW9 3AB, UK Amanda Cooper Disease Control Division, Ministry of Health, Federal Government Administration Centre, Putrajaya, Malaysia 1 Jenarun Jelip Division of Public Health, Sabah Department of Health, Kota Kinabalu, Sabah, Malaysia Tanrang Husin 2 Abstract In lowland areas of Malaysia, Plasmodium knowlesi infection is associated with land use change and high proportions of the vector Anopheles balabacensis. We conducted a 15-month study in two Malaysian villages to determine the effect of habitat on vector populations in understudied high-altitude, high-incidence districts. Anopheles mosquitoes were sampled in human settlements, plantations and forest edges, and screened for Plasmodium species by PCR. We report the first An. donaldi positive for P. knowlesi. This potential vector was associated with habitat fragmentation measured as disturbed forest edge:area ratio, while An. balabacensis was not, indicating fragmented land use could favour An. donaldi. Anopheline species richness and diversity decreased from forest edge, to plantation, to human settlement. Greater numbers of An. balabacensis and An. -
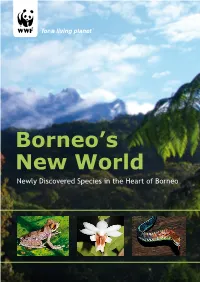
Borneo's New World
Borneo’s New World Newly Discovered Species in the Heart of Borneo Dendrelaphis haasi, a new snake species discovered in 2008 © Gernot Vogel © Gernot WWF’s Heart of Borneo Vision With this report, WWF’s Initiative in support of the Heart of Borneo recognises the work of scientists The equatorial rainforests of the Heart and researchers who have dedicated countless hours to the discovery of of Borneo are conserved and effectively new species in the Heart of Borneo, managed through a network of protected for the world to appreciate and in its areas, productive forests and other wisdom preserve. sustainable land-uses, through cooperation with governments, private sector and civil society. Cover photos: Main / View of Gunung Kinabalu, Sabah © Eric in S F (sic); © A.Shapiro (WWF-US). Based on NASA, Visible Earth, Inset photos from left to right / Rhacophorus belalongensis © Max Dehling; ESRI, 2008 data sources. Dendrobium lohokii © Amos Tan; Dendrelaphis kopsteini © Gernot Vogel. A declaration of support for newly discovered species In February 2007, an historic Declaration to conserve the Heart of Borneo, an area covering 220,000km2 of irreplaceable rainforest on the world’s third largest island, was officially signed between its three governments – Brunei Darussalam, Indonesia and Malaysia. That single ground breaking decision taken by the three through a network of protected areas and responsibly governments to safeguard one of the most biologically managed forests. rich and diverse habitats on earth, was a massive visionary step. Its importance is underlined by the To support the efforts of the three governments, WWF number and diversity of species discovered in the Heart launched a large scale conservation initiative, one that of Borneo since the Declaration was made. -

Status of Coral Reefs in Malaysia, 2019
Status of Coral Reefs in Malaysia, 2019 Reef Check Malaysia Contents Executive Summary 1 1 Introduction 2 2 Reef Check 3 2.1 Background 3 2.2 Survey Methodology 3 2.3 Survey Sites 4 3 2019 Survey Results & Analysis 5 3.1 Status of Coral Reefs in Malaysia 5 3.2 Status of Coral Reefs in Key Eco-regions in Malaysia 10 Sunda Shelf 12 Malacca Strait 36 North Borneo 42 4 Reef Check Data Over the Year 60 4.1 Peninsular versus East Malaysia over 13 Years 60 4.2 Changing Reef Health in Selected Areas 65 5 Summary and Recommendations 75 5.1 Summary 75 5.2 Recommendations 76 5.3 Conclusion 77 Acknowledgements 78 References 81 Appendix 1: 2019 Survey Sites 82 Saving Our Reefs Research, Education, Conservation Executive Summary 1. A total of 180 sites were surveyed in 2019 (2018: 212), 97 in Peninsular Malaysia and 83 in East Malaysia. The surveys are a continuation of a successful National Reef Check Survey Programme that has now run for thirteen years. 2. The surveys were carried out by trained volunteers as well as government officials from Marine Parks Malaysia, reflecting commitment from the Government in further improving management of Malaysia’s coral reefs. Surveys were carried out on several islands off Peninsular Malaysia’s East and West coast, covering both established Marine Protected Areas (MPAs) and non-protected areas, and in various parts of East Malaysia, both Sabah and Sarawak. 3. The results indicate that the Malaysian coral reefs surveyed have a relatively high level of living coral, at 40.63% (2018: 42.42%). -

Wave Characteristics in Sabah Waters
American Journal of Environmental Sciences 6 (3): 219-223, 2010 ISSN 1553-345X © 2010 Science Publications Wave Characteristics in Sabah Waters 1Ejria Saleh, 1Jessie Beliku, 1Than Aung and 2Awnesh Singh 1Borneo Marine Research Institute, University Malaysia Sabah, Locked Bag 2073, 88999 Kota Kinabalu, Sabah, Malaysia 2Laboratory Studies in Geophysics and Oceanography Space, 14 Avenue Edouard Belin, 31400 Toulouse France Abstract: Problem statement: This study was conducted to identify and compare the wave characteristics in Sabah waters at five different key locations so as to determine the effects of the Northeast Monsoon (NEM) and the Southwest Monsoon (SWM) along the east and west coasts of Sabah. Approach: Monthly wave height and wave period data for 8 years covering offshore areas of Labuan, Kota Kinabalu (KK), Kudat, Sandakan and Tawau were collected from the Meteorological Department, Sabah Branch. The data was analyzed at different areas through the Probability Density Function (PDF) to estimate the most likely wave height and wave period in the study area. Wave power was also calculated using the wave power formula to identify the strength of waves in Sabah waters. The significance of wave characteristics during the NEM and the SWM for the east coast (Sandakan and Tawau) and west coast (Labuan and KK) of Sabah are presented in this study. Results: The range of wave heights in coastal waters surrounding Sabah was found to be 0.5-2 m. Wave height is usually higher than 1 m in the west coast during NEM while the east coast has a wave height of ~0.5 m for − both monsoons. -

Itinerary 1 Getting to Kudat
Suggested Itineraries Overnight stays are highly recommended, and itineraries can be tailor-made to your preference. Contact the community representatives for the ultimate AKCC experience. banggi Itinerary 1 Itinerary 2 Getting to Kudat: bavang jamal 2 Days/ 1 Night - Tajau Laut and Inukiran 3 Days/2 Nights - Inukiran, Loro Kecil, • By Bus: Kudat is served by several bus companies Bavang Jamal, and Tajau Laut tajau laut in Kota Kinabalu and Sandakan. Day 1 - Tajau Laut /Simpang Magayau loro kecil • By car: Cars for rent are found at Kota Kinabalu • Leave Kota Kinabalu - Lunch Day 1 - Inukiran International Airport. Road journeys to Kudat take • Briefing followed by snorkeling or activity • Leave Kota Kinabalu for Inukiran kudat up to 3 hours. of choice - Tea break - Lunch • Sunset trip to Simpang Magayau • Craft and cultural demonstration Getting to AKCC by Public Transport: • Dinner and cultural activities at Tajau Laut - Tea break • Visitors travelling by bus to Inukiran, Bavang • Village trails and/or hike to the peak of Jamal, Loro Kecil, and Tajau Laut can be dropped Day 2 - Inukiran Matunggong forest reserve off along the main road to Kudat and can request • Sunrise beach breakfast/Leave Tajau Laut • Dinner and cultural activities at for pick-up. for Inukiran Inukiran inukiran • Visitors to Banggi Island can take the public ferry • Craft and cultural activities at Inukiran from Kudat port to Karakit. - Lunch Day 2 - Loro Kecil/Bavang Jamal • Visit to gong-makers of Sumangkap • Trip to Loro Kecil and hiking in the For details, contact: - Tea break headlands of the cove or activity of • Return to Kota Kinabalu choice - Lunch 1. -

Borneo's New World
Borneo’s New World Newly Discovered Species in the Heart of Borneo Dendrelaphis haasi, a new snake species discovered in 2008 © Gernot Vogel © Gernot Heart of Borneo Vision With this report, WWF’s Initiative in support of the Heart of Borneo recognises the work of scientists The equatorial rainforests of the Heart and researchers who have dedicated countless hours to the discovery of of Borneo are conserved and effectively new species in the Heart of Borneo, managed through a network of protected for the world to appreciate and in its areas, productive forests and other wisdom preserve. sustainable land-uses, through cooperation with governments, the private sector and civil society. Cover photos: Main / View of Gunung Kinabalu, Sabah © Eric in S F (sic); © A.Shapiro (WWF-US). Based on NASA, Visible Earth, Inset photos from left to right / Rhacophorus belalongensis © Max Dehling; ESRI, 2008 data sources. Dendrobium lohokii © Amos Tan; Dendrelaphis kopsteini © Gernot Vogel. A declaration of support for biodiversity In February 2007, an historic Declaration to conserve the Heart of Borneo, an area covering 220,000km2 of irreplaceable rainforest on the world’s third largest island, was officially signed between its three governments – Brunei Darussalam, Indonesia and Malaysia. That single ground breaking decision taken by the three WWF’s Heart of Borneo Initiative governments to safeguard one of the most biologically rich and diverse habitats on earth, was a massive To support the efforts of the three governments, WWF visionary step. Its importance is underlined by the launched a large scale conservation initiative, one that number and diversity of species discovered in the Heart spans the local-to-global spectrum. -

Tourism Growth & Challenges
Sharing P roperty Information in S abah with You PPH 260/7/2008(006770) Volume XIV, December 2007 Tourism GGGGGGrrrrrroooooowwwwwwtttttthhhhhh &&&&&& CCCCCChhhhhhaaaaaalllllllllllleeeeeennnnnnggggggeeeeeessssss Melapi Restaurant at Sukau Rainforest Lodge 1 Borneo Hypermall Inside this issue ● New Hotel Developments Of late, Sabah has been abuzz with talks of tourism-related ● Lahad Datu: Facts & Figures ● Happenings events. Sabah Tourism Board statistics show a 14% jump in ● New Developments visitor arrivals to 2.1 million from 2005 to 2006, generating ● Budget 2008 Highlights ● Feature Developments: Taman receipts of RM2.6billion. Arrivals up to October 2007 have Malakun & Puteri Damai reached 1.9million. Major resort and hotels in the State Capital are reporting good take up rates. Sabah is gearing up for more Lumpur and then to Sabah. Coupled active years ahead with the completion of the low cost carrier with new direct flights by other airlines from Asia, this has created a positive terminal in January 2007 and the massive upgrade of the Kota optimism that with the completion of Kinabalu International Airport, which is expected to see its first the airport extension, visitor arrivals to Sabah will increase manifold. Even phase completed by April 2008. Close to 2,000 hotel rooms of without the new airport extension, the various classifications are currently under construction in Kota Low Cost Carrier Terminal is already doing well through Air Asia. We were all caught flat footed as this has never happened to us WTWS: How would you describe tourism in Sabah? before. If the same thing happened to the international Teo: Sabah is entering a new and most exciting phase airport, the ripple effect will be even more significant.