Identification of Candidate Agents Active Against N. Ceranae Infection in Honey Bees: Establishment of a Medium Throughput Screening Assay Based on N
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antiseptics and Disinfectants for the Treatment Of
Verstraelen et al. BMC Infectious Diseases 2012, 12:148 http://www.biomedcentral.com/1471-2334/12/148 RESEARCH ARTICLE Open Access Antiseptics and disinfectants for the treatment of bacterial vaginosis: A systematic review Hans Verstraelen1*, Rita Verhelst2, Kristien Roelens1 and Marleen Temmerman1,2 Abstract Background: The study objective was to assess the available data on efficacy and tolerability of antiseptics and disinfectants in treating bacterial vaginosis (BV). Methods: A systematic search was conducted by consulting PubMed (1966-2010), CINAHL (1982-2010), IPA (1970- 2010), and the Cochrane CENTRAL databases. Clinical trials were searched for by the generic names of all antiseptics and disinfectants listed in the Anatomical Therapeutic Chemical (ATC) Classification System under the code D08A. Clinical trials were considered eligible if the efficacy of antiseptics and disinfectants in the treatment of BV was assessed in comparison to placebo or standard antibiotic treatment with metronidazole or clindamycin and if diagnosis of BV relied on standard criteria such as Amsel’s and Nugent’s criteria. Results: A total of 262 articles were found, of which 15 reports on clinical trials were assessed. Of these, four randomised controlled trials (RCTs) were withheld from analysis. Reasons for exclusion were primarily the lack of standard criteria to diagnose BV or to assess cure, and control treatment not involving placebo or standard antibiotic treatment. Risk of bias for the included studies was assessed with the Cochrane Collaboration’s tool for assessing risk of bias. Three studies showed non-inferiority of chlorhexidine and polyhexamethylene biguanide compared to metronidazole or clindamycin. One RCT found that a single vaginal douche with hydrogen peroxide was slightly, though significantly less effective than a single oral dose of metronidazole. -

Index Vol. 12-15
353 INDEX VOL. 12-15 Die Stichworte des Sachregisters sind in der jeweiligen Sprache der einzelnen Beitrage aufgefiihrt. Les termes repris dans la Table des matieres sont donnes selon la langue dans laquelle l'ouvrage est ecrit. The references of the Subject Index are given in the language of the respective contribution. 14 AAG (Alpha-acid glycoprotein) 120 14 Adenosine 108 12 Abortion 151 12 Adenosine-phosphate 311 13 Abscisin 12, 46, 66 13 Adenosine-5'-phosphosulfate 148 14 Absorbierbarkeit 317 13 Adenosine triphosphate 358 14 Absorption 309, 350 15 S-Adenosylmethionine 261 13 Absorption of drugs 139 13 Adipaenin (Spasmolytin) 318 14 - 15 12 Adrenal atrophy 96 14 Absorptionsgeschwindigkeit 300, 306 14 - 163, 164 14 Absorptionsquote 324 13 Adrenal gland 362 14 ACAI (Anticorticocatabolic activity in 12 Adrenalin(e) 319 dex) 145 14 - 209, 210 12 Acalo 197 15 - 161 13 Aceclidine (3-Acetoxyquinuclidine) 307, 13 {i-Adrenergic blockers 119 308, 310, 311, 330, 332 13 Adrenergic-blocking activity 56 13 Acedapsone 193,195,197 14 O(-Adrenergic blocking drugs 36, 37, 43 13 Aceperone (Acetabutone) 121 14 {i-Adrenergic blocking drugs 38 12 Acepromazin (Plegizil) 200 14 Adrenergic drugs 90 15 Acetanilid 156 12 Adrenocorticosteroids 14, 30 15 Acetazolamide 219 12 Adrenocorticotropic hormone (ACTH) 13 Acetoacetyl-coenzyme A 258 16,30,155 12 Acetohexamide 16 14 - 149,153,163,165,167,171 15 1-Acetoxy-8-aminooctahydroindolizin 15 Adrenocorticotropin (ACTH) 216 (Slaframin) 168 14 Adrenosterone 153 13 4-Acetoxy-1-azabicyclo(3, 2, 2)-nonane 12 Adreson 252 -

4. Antibacterial/Steroid Combination Therapy in Infected Eczema
Acta Derm Venereol 2008; Suppl 216: 28–34 4. Antibacterial/steroid combination therapy in infected eczema Anthony C. CHU Infection with Staphylococcus aureus is common in all present, the use of anti-staphylococcal agents with top- forms of eczema. Production of superantigens by S. aureus ical corticosteroids has been shown to produce greater increases skin inflammation in eczema; antibacterial clinical improvement than topical corticosteroids alone treatment is thus pivotal. Poor patient compliance is a (6, 7). These findings are in keeping with the demon- major cause of treatment failure; combination prepara- stration that S. aureus can be isolated from more than tions that contain an antibacterial and a topical steroid 90% of atopic eczema skin lesions (8); in one study, it and that work quickly can improve compliance and thus was isolated from 100% of lesional skin and 79% of treatment outcome. Fusidic acid has advantages over normal skin in patients with atopic eczema (9). other available topical antibacterial agents – neomycin, We observed similar rates of infection in a prospective gentamicin, clioquinol, chlortetracycline, and the anti- audit at the Hammersmith Hospital, in which all new fungal agent miconazole. The clinical efficacy, antibac- patients referred with atopic eczema were evaluated. In terial activity and cosmetic acceptability of fusidic acid/ a 2-month period, 30 patients were referred (22 children corticosteroid combinations are similar to or better than and 8 adults). The reason given by the primary health those of comparator combinations. Fusidic acid/steroid physician for referral in 29 was failure to respond to combinations work quickly with observable improvement prescribed treatment, and one patient was referred be- within the first week. -
Clioquinol: Summary Report
Clioquinol: Summary Report Item Type Report Authors Gianturco, Stephanie L.; Pavlech, Laura L.; Storm, Kathena D.; Yoon, SeJeong; Yuen, Melissa V.; Mattingly, Ashlee N. Publication Date 2020-01 Keywords Clioquinol; Compounding; Food, Drug, and Cosmetic Act, Section 503B; Food and Drug Administration; Outsourcing facility; Drug compounding; Legislation, Drug; United States Food and Drug Administration Rights Attribution-NoDerivatives 4.0 International Download date 24/09/2021 22:12:31 Item License http://creativecommons.org/licenses/by-nd/4.0/ Link to Item http://hdl.handle.net/10713/12091 Summary Report Clioquinol Prepared for: Food and Drug Administration Clinical use of bulk drug substances nominated for inclusion on the 503B Bulks List Grant number: 2U01FD005946 Prepared by: University of Maryland Center of Excellence in Regulatory Science and Innovation (M-CERSI) University of Maryland School of Pharmacy January 2020 This report was supported by the Food and Drug Administration (FDA) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award (U01FD005946) totaling $2,342,364, with 100 percent funded by the FDA/HHS. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, the FDA/HHS or the U.S. Government. 1 Table of Contents REVIEW OF NOMINATIONS ................................................................................................... 4 METHODOLOGY ................................................................................................................... -

Effect of 8-Hydroxyquinoline and Derivatives on Human Neuroblastoma SH-SY5Y Cells Under High Glucose
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Crossref Effect of 8-hydroxyquinoline and derivatives on human neuroblastoma SH-SY5Y cells under high glucose Wilasinee Suwanjang1, Supaluk Prachayasittikul2 and Virapong Prachayasittikul3 1 Center for Research and Innovation, Faculty of Medical Technology, Mahidol University, Bangkok, Thailand 2 Center of Data Mining and Biomedical Informatics, Faculty of Medical Technology, Mahidol University, Bangkok, Thailand 3 Department of Clinical Microbiology and Applied Technology, Faculty of Medical Technology, Mahidol University, Bangkok, Thailand ABSTRACT 8-Hydroxyquinoline and derivatives exhibit multifunctional properties, including antioxidant, antineurodegenerative, anticancer, anti-inflammatory and antidiabetic activities. In biological systems, elevation of intracellular calcium can cause calpain activation, leading to cell death. Here, the effect of 8-hydroxyquinoline and derivatives (5-chloro-7-iodo-8-hydroxyquinoline or clioquinol and 8-hydroxy-5-nitroquinoline or nitroxoline) on calpain-dependent (calpain-calpastatin) pathways in human neu- roblastoma (SH-SY5Y) cells was investigated. 8-Hydroxyquinoline and derivatives ameliorated high glucose toxicity in SH-SY5Y cells. The investigated compounds, particularly clioquinol, attenuated the increased expression of calpain, even under high- glucose conditions. 8-Hydroxyquinoline and derivatives thus adversely affected the promotion of neuronal cell death by high glucose via the calpain-calpastatin -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -
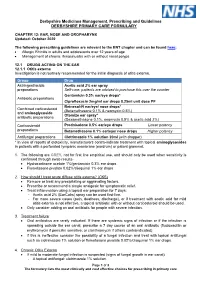
EAR, NOSE and OROPHARYNX Updated: October 2020
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

ESCMID Online Lecture Library © by Author ESCMID Online Lecture Library
Microsporidia, Dientamoeba and Blastocystis. © by author Tom van Gool Section Parasitology, AcademicESCMID Medical Online Centre, Amsterdam,Lecture NetherlandsLibrary Microsporidiosis in HIV-infected and HIV-negative individuals © by author ESCMID Online Lecture Library 1985: Mr. P. Bieneusi in Paris with AIDS ….in a biopsy of the small intestine a strange microorganism was observed with EM…… © by author ESCMID Online Lecture Library Prof. Isabelle Desportes Hôpital Pitié-Salpêtrière (Paris) © by author ESCMID Online Lecture Library “Small parasite belonging to the microsporidia but is unknown species”: Enterocytozoon bieneusi Microsporidia • obligate intracellular protozoan parasites • more than 144 genera and 1200 species • important parasites© by author in all phyla of animals ESCMID Online Lecture Library • since 1985 recognized in AIDS • nowadays 9 genera and 14 species Typical spore stage of microsporidia Coiled polar filament © by author ESCMID Online LectureThick Library exopspore with chitin Life cycle of microsporidia (Encephalitozoon) E.i. © by author ESCMID Online Lecture Library E.h. Schottelius MI 2000 Important microsporidia in AIDS I • Enterocytozoon bieneusi • Discovered in 1985 • Named after© byMr author Bieneusi • Most important microsporidian in ESCMIDAIDS Online Lecture Library The Lancet, Clinical Practice, 1991 • chronic diarrhea • cholangiopathy • rhinosinusitis© by author ESCMID• HIV infectedOnline patients Lecture CD 4Library <100 Diagnosis of Enterocytozoon bieneusi © by author ESCMID Online Lecture Library Diagnosis of human microsporidiosis 1985: electron microscopy of duodenal biopsies © by author ESCMID Online Lecture Library Drawback of all earlier methods of diagnosis: invasive procedure (small intestinal biopsy) needed Wanted: easy, non-invasive diagnostic procedure © by author ESCMID Online Lecture Library © by author ESCMID Online Lecture Library E. bieneusi with Uvitex 2B stain © by author ESCMID Online Lecture Library E. -

Infectious Keratitis: Short Answers
Q Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? A Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas Infectious keratitis: Short answers Pseudomonas corneal ulcer associated with CL wear Q Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? A Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? CL wear Infectious keratitis: Short answers Acanthamoeba keratitis associated with CL wear Q Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? CL wear What are the three main culprits in fungal keratitis? What is the topical antifungal of choice for each? Fusarium:fungus 1 Topical…natamycin Aspergillisfungus 2 and Candida:fungus 3 A Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? CL wear What are the three main culprits in fungal keratitis? What is the topical antifungal of choice for each? Candida: Topical…natamycin Aspergillis and Fusarium: Q Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? CL wear What are the three main culprits in fungal keratitis? -

Chemical Modulators of Fibrinogen Production and Their Impact on Venous Thrombosis
Published online: 2020-12-10 Coagulation and Fibrinolysis 433 Chemical Modulators of Fibrinogen Production and Their Impact on Venous Thrombosis Rui Vilar1 Samuel W. Lukowski1,2 Marco Garieri1 Corinne Di Sanza1 Marguerite Neerman-Arbez1,3 Richard J. Fish1 1 Department of Genetic Medicine and Development, University of Address for correspondence Richard J. Fish, Department of Genetic Geneva Faculty of Medicine, Geneva, Switzerland Medicine and Development, Faculty of Medicine, University of 2 Institute for Molecular Bioscience, The University of Queensland, Geneva, 1, rue Michel-Servet, Geneva 1206, Switzerland Saint Lucia, Queensland, Australia (e-mail: [email protected]). 3 iGE3, Institute of Genetics and Genomics in Geneva, Geneva, Switzerland Thromb Haemost 2021;121:433–448. Abstract Thrombosis is a leading cause of morbidity and mortality. Fibrinogen, the soluble substrate for fibrin-based clotting, has a central role in haemostasis and thrombosis and its plasma concentration correlates with cardiovascular disease event risk and a prothrombotic state in experimental models. We aimed to identify chemical entities capable of changing fibrinogen production and test their impact on experimental thrombosis. A total of 1,280 bioactive compounds were screened for their ability to alter fibrinogen production by hepatocyte-derived cancer cells and a selected panel was tested in zebrafish larvae. Anthralin and all-trans retinoic acid (RA) were identified as fibrinogen-lowering and fibrinogen-increasing moieties, respectively. In zebrafish larvae, anthralin prolonged laser-induced venous occlusion times and reduced thrombocyte accumulation at injury sites. RA had opposite effects. Treatment with RA, a nuclear receptor ligand, increased fibrinogen mRNA levels. Using an antisense morpholino oligonucleotide to deplete zebra- fish fibrinogen, we correlated a shortening of laser-induced venous thrombosis times with RA treatment and fibrinogen protein levels. -

Raised Serum Protein-Bound Iodine After Topical Clioquinol A. C
Case reports 515 Postgrad Med J: first published as 10.1136/pgmj.47.549.515 on 1 July 1971. Downloaded from Raised serum protein-bound iodine after topical clioquinol A. C. UPJOHN H-J. B. GALBRAITH M.R.C.S., L.R.C.P. M.D., F.R.C.P. General Practitioner, Ongar Physician, Chelmsford Hospitals BETHEL SOLOMONS M.D., F.R.C.P.I. Dermatologist, Chelmsford Hospitals RAISED serum levels ofprotein-bound iodine (PBI) in hydrocortisone cream, and continued to do so for 17 patients with normal thyroid function have been weeks until her first out-patient visit to the skin observed on many occasions after oral treatment department (B. S.). Apart from her varicose condi- with 5-chloro-7-iodo-8-hydroxyquinoline (iodo- tion she. complained of constant nervousness. chlorhydroxyquinoline, clioquinol, Enterovioform) Further examination revealed some signs of thyro- (Thoren, 1960; Levin, Josephson & Grtnewald, toxicosis. The PBI was 22 tug/100 ml. She stopped 1966; Sonksen et al., 1968). It is less well appre- using the cream, and 3 weeks later her PBI was 5-2 Protected by copyright. ciated that clioquinol administered topically can [ug/100 ml. She agreed to use the cream again, and be absorbed in sufficient quantities to influence after 3 weeks, during which time she had used nearly the PBI and the uptake of radio-active iodine by the three 20 g tubes, her PBI was 13-4 [g/100 ml. She thyroid gland. then stopped using the cream and her PBI had returned to 5 0 tzg/100 ml a month later. -

The Medical Letter
Page 1 of 2 MICROSPORIDIOSIS Drug Adult dosage Pediatric dosage Ocular (Encephalitozoon hellem, E.cuniculi, Vittaforma corneae [Nosema corneum]) Drug of choice: Albendazole1,2 400 mg PO bid plus fumagillin3* Intestinal (E. bieneusi, E. [Septata] intestinalis) E. bieneusi Drug of choice: Fumagillin4* 20 mg PO tid x 14d E. intestinalis Drug of choice: Albendazole1,2 400 mg PO bid x 21d Disseminated (E. hellem, E. cuniculi, E. intestinalis, Pleistophora sp., Trachipleistophora sp. and Brachiola vesicularum) Drug of choice:5 Albendazole1,2* 400 mg PO bid * Availability problems. See table below. 1. Not FDA-approved for this indication. 2. Albendazole must be taken with food; a fatty meal increases oral bioavailability. 3. CM Chan et al, Ophthalmology 2003; 110:1420. Ocular lesions due to E. hellem in HIV-infected patients have responded to fumagillin eyedrops prepared from Fumidil-B (bicyclohexyl ammonium fumagillin) used to control a microsporidial disease of honey bees (MJ Garvey et al, Ann Pharmacother 1995; 29:872), available from Leiter’s Park Avenue Pharmacy, San Jose, CA (800-292-6773; www.leit- errx.com) is a compounding pharmacy that specializes in ophthalmic drugs. For lesions due to V. corneae, topical therapy is gener- ally not effective and keratoplasty may be required (RM Davis et al, Ophthalmology 1990; 97:953). 4. Oral fumagillin (Flisint – Sanofi-Aventis, France) has been effective in treating E. bieneusi (J-M Molina et al, N Engl J Med 2002; 346:1963), but has been associated with thrombocytopenia and neutropenia. Highly active antiretroviral therapy (HAART) may lead to microbiologic and clinical response in HIV-infected patients with microsporidial diarrhea.