The 10 Most Common Toxicoses in Dogs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Characterization of Residential Pest Control Products Used in Inner City Communities in New York City
Journal of Exposure Science and Environmental Epidemiology (2010), 1–11 r 2010 Nature America, Inc. All rights reserved 1559-0631/10 www.nature.com/jes Characterization of residential pest control products used in inner city communities in New York City MEGAN K. HORTONa, J. BRYAN JACOBSONb, WENDY MCKELVEYb, DARRELL HOLMESa, BETTY FINCHERc, AUDREY QUANTANOc, BEINVENDIDA PAEZ DIAZc, FAYE SHABBAZZc, PEGGY SHEPARDc, ANDREW RUNDLEa AND ROBIN M. WHYATTa aColumbia Center for Children’s Environmental Health, Mailman School of Public Health, Columbia University, New York, New York, USA bNew York City Department of Health and Mental Hygiene, New York, New York, USA cWest Harlem Environmental Action, New York, New York, USA The Columbia Center for Children’s Environmental Health (CCCEH) previously reported widespread residential insecticide use in urban communities in New York City. Research suggests that pyrethroids are replacing organophosphates (OPs) in response to 2000–2001 US EPA pesticide regulations restricting OP use. A systematic assessment of active ingredients used for residential pest control is lacking. We queried a database of pesticide applications reported by licensed applicators between 1999 and 2005 and surveyed pest control products available in 145 stores within 29 zip codes in the CCCEH catchment area including Northern Manhattan and the South Bronx. Pyrethroids, pyrethrins, piperonyl butoxide, and hydramethylnon were the most common insecticide active ingredients reported as used by licensed pesticide applicators within the 29 zip codes of the CCCEH catchment area between 1999 and 2005. Use of certain pyrethroids and some non-spray insecticides such as fipronil and boric acid increased significantly by year (logistic regression, OR41.0, Po0.05), whereas use of OPs, including chlorpyrifos and diazinon decreased significantly by year (logistic regression, ORo1.0, Po0.05). -

Animal Behaviour, Animal Welfare and the Scientific Study of Affect
WellBeing International WBI Studies Repository 5-2009 Animal Behaviour, Animal Welfare and the Scientific Study of Affect David Fraser University of British Columbia Follow this and additional works at: https://www.wellbeingintlstudiesrepository.org/emotio Part of the Animal Studies Commons, Comparative Psychology Commons, and the Other Animal Sciences Commons Recommended Citation Fraser, D. (2009). Animal behaviour, animal welfare and the scientific study of affect. Applied Animal Behaviour Science, 118(3), 108-117. This material is brought to you for free and open access by WellBeing International. It has been accepted for inclusion by an authorized administrator of the WBI Studies Repository. For more information, please contact [email protected]. Animal Behaviour, Animal Welfare and the Scientific Study of Affect David Fraser University of British Columbia KEYWORDS animal behaviour, animal welfare, affect, emotion, qualitative research ABSTRACT Many questions about animal welfare involve the affective states of animals (pain, fear, distress) and people look to science to clarify these issues as a basis for practices, policies and standards. However, the science of the mid twentieth century tended to be silent on matters of animal affect for both philosophical and methodological reasons. Philosophically, under the influence of Positivism many scientists considered that the affective states of animals fall outside the scope of science. Certain methodological features of the research also favoured explanations that did not involve affect. The features included the tendency to rely on abstract, quantitative measures rather than description, to use controlled experiments more than naturalistic observation, and to focus on measures of central tendency (means, medians) rather than individual differences. -

Functional Aspects of Emotions in Fish
Behavioural Processes 100 (2013) 153–159 Contents lists available at ScienceDirect Behavioural Processes jou rnal homepage: www.elsevier.com/locate/behavproc Functional aspects of emotions in fish ∗ Silje Kittilsen Norwegian School of Veterinary Science, Norway a r t i c l e i n f o a b s t r a c t Article history: There is an ongoing scientific discussion on whether fish have emotions, and if so how they experience Received 19 March 2013 them? The discussion has incorporated important areas such as brain anatomy and function, physiological Received in revised form and behavioural responses, and the cognitive abilities that fish possess. Little attention has however, been 10 September 2013 directed towards what functional aspects emotions ought to have in fish. If fish have emotions – why? Accepted 11 September 2013 The elucidation of this question and an assessment of the scientific evidences of emotions in fish in an evolutionary and functional framework would represent a valuable contribution in the discussion on Keywords: whether fish are emotional creatures. Here parts of the vast amount of literature from both biology and Emotions Behaviour psychology relating to the scientific field of emotions, animal emotion, and the functional aspects that Cognition emotions fulfil in the lives of humans and animals are reviewed. Subsequently, by viewing fish behaviour, Psychology physiology and cognitive abilities in the light of this functional framework it is possible to infer what Fish functions emotions may serve in fish. This approach may contribute to the vital running discussion on Evolution the subject of emotions in fish. In fact, if it can be substantiated that emotions are likely to serve a function in fish similar to that of other higher vertebrate species, the notion that fish do have emotions will be strengthened. -

AVMA Guidelines for the Euthanasia of Animals: 2020 Edition*
AVMA Guidelines for the Euthanasia of Animals: 2020 Edition* Members of the Panel on Euthanasia Steven Leary, DVM, DACLAM (Chair); Fidelis Pharmaceuticals, High Ridge, Missouri Wendy Underwood, DVM (Vice Chair); Indianapolis, Indiana Raymond Anthony, PhD (Ethicist); University of Alaska Anchorage, Anchorage, Alaska Samuel Cartner, DVM, MPH, PhD, DACLAM (Lead, Laboratory Animals Working Group); University of Alabama at Birmingham, Birmingham, Alabama Temple Grandin, PhD (Lead, Physical Methods Working Group); Colorado State University, Fort Collins, Colorado Cheryl Greenacre, DVM, DABVP (Lead, Avian Working Group); University of Tennessee, Knoxville, Tennessee Sharon Gwaltney-Brant, DVM, PhD, DABVT, DABT (Lead, Noninhaled Agents Working Group); Veterinary Information Network, Mahomet, Illinois Mary Ann McCrackin, DVM, PhD, DACVS, DACLAM (Lead, Companion Animals Working Group); University of Georgia, Athens, Georgia Robert Meyer, DVM, DACVAA (Lead, Inhaled Agents Working Group); Mississippi State University, Mississippi State, Mississippi David Miller, DVM, PhD, DACZM, DACAW (Lead, Reptiles, Zoo and Wildlife Working Group); Loveland, Colorado Jan Shearer, DVM, MS, DACAW (Lead, Animals Farmed for Food and Fiber Working Group); Iowa State University, Ames, Iowa Tracy Turner, DVM, MS, DACVS, DACVSMR (Lead, Equine Working Group); Turner Equine Sports Medicine and Surgery, Stillwater, Minnesota Roy Yanong, VMD (Lead, Aquatics Working Group); University of Florida, Ruskin, Florida AVMA Staff Consultants Cia L. Johnson, DVM, MS, MSc; Director, -
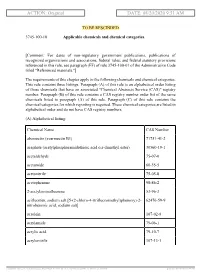
ACTION: Original DATE: 08/20/2020 9:51 AM
ACTION: Original DATE: 08/20/2020 9:51 AM TO BE RESCINDED 3745-100-10 Applicable chemicals and chemical categories. [Comment: For dates of non-regulatory government publications, publications of recognized organizations and associations, federal rules, and federal statutory provisions referenced in this rule, see paragraph (FF) of rule 3745-100-01 of the Administrative Code titled "Referenced materials."] The requirements of this chapter apply to the following chemicals and chemical categories. This rule contains three listings. Paragraph (A) of this rule is an alphabetical order listing of those chemicals that have an associated "Chemical Abstracts Service (CAS)" registry number. Paragraph (B) of this rule contains a CAS registry number order list of the same chemicals listed in paragraph (A) of this rule. Paragraph (C) of this rule contains the chemical categories for which reporting is required. These chemical categories are listed in alphabetical order and do not have CAS registry numbers. (A) Alphabetical listing: Chemical Name CAS Number abamectin (avermectin B1) 71751-41-2 acephate (acetylphosphoramidothioic acid o,s-dimethyl ester) 30560-19-1 acetaldehyde 75-07-0 acetamide 60-35-5 acetonitrile 75-05-8 acetophenone 98-86-2 2-acetylaminofluorene 53-96-3 acifluorfen, sodium salt [5-(2-chloro-4-(trifluoromethyl)phenoxy)-2- 62476-59-9 nitrobenzoic acid, sodium salt] acrolein 107-02-8 acrylamide 79-06-1 acrylic acid 79-10-7 acrylonitrile 107-13-1 [ stylesheet: rule.xsl 2.14, authoring tool: RAS XMetaL R2_0F1, (dv: 0, p: 185720, pa: -

(12) United States Patent (10) Patent No.: US 8,852,618 B2 Clough (45) Date of Patent: Oct
USOO8852618B2 (12) United States Patent (10) Patent No.: US 8,852,618 B2 Clough (45) Date of Patent: Oct. 7, 2014 (54) INSECTICIDAL MIXTURE CONTAINING CA 2429218 A1 6, 2002 GAMMA-CYHALOTHRN CH 689326 A5 4f1995 EP O237227 A1 9, 1987 EP 0771526 A2 5, 1997 (75) Inventor: Martin Stephen Clough, Bracknell EP O988788 A1 3f2000 (GB) FR 272O230 A1 12/1995 JP 63. 126805 A2 5, 1988 (73) Assignee: Syngenta Limited, Guildford (GB) JP 63126805 A2 5, 1988 JP 63126805 5, 1998 c - r WO WO 86 O7525 A1 12, 1986 (*) Notice: Subject to any disclaimer, the term of this WO WO 93 03618 A2 3, 1993 patent is extended or adjusted under 35 WO WO95 229O2 A1 8/1995 U.S.C. 154(b) by 824 days. WO WO9533380 A1 12, 1995 WO WO 96 16543 A2 6, 1996 (21) Appl. No.: 12/633,063 WO WO97 06687 A1 2/1997 WO WO974O692 A1 11, 1997 (22) Filed: Dec.a V88, 2009 WO WOOOO2453 A1 1, 2000 OTHER PUBLICATIONS (65) Prior Publication Data US 201O/OO81714 A1 Apr. 1, 2010 Canadian Office Action (Applin. No. 2,452,515 filed: Jul. 10, 2002) mailing date Oct. 1, 2010 (pp. 1-2). Related U.S. Application Data Allen et al. Transgenic & Conventional Insect & Weed Control Sys tems; Proceedings of the Beltwide Cotton Conference, vol. 2, 1065 (62) Division of application No. 10/484.745, filed as 1068 (1999), USA. application No. PCT/GB02/03181 on Jul. 10, 2002, Anonymous; Pesticide Mixtures for Control of Insect and Acarid now Pat. No. -

Veterinary Toxicology
GINTARAS DAUNORAS VETERINARY TOXICOLOGY Lecture notes and classes works Study kit for LUHS Veterinary Faculty Foreign Students LSMU LEIDYBOS NAMAI, KAUNAS 2012 Lietuvos sveikatos moksl ų universitetas Veterinarijos akademija Neužkre čiam ųjų lig ų katedra Gintaras Daunoras VETERINARIN Ė TOKSIKOLOGIJA Paskait ų konspektai ir praktikos darb ų aprašai Mokomoji knyga LSMU Veterinarijos fakulteto užsienio studentams LSMU LEIDYBOS NAMAI, KAUNAS 2012 UDK Dau Apsvarstyta: LSMU VA Veterinarijos fakulteto Neužkre čiam ųjų lig ų katedros pos ėdyje, 2012 m. rugs ėjo 20 d., protokolo Nr. 01 LSMU VA Veterinarijos fakulteto tarybos pos ėdyje, 2012 m. rugs ėjo 28 d., protokolo Nr. 08 Recenzavo: doc. dr. Alius Pockevi čius LSMU VA Užkre čiam ųjų lig ų katedra dr. Aidas Grigonis LSMU VA Neužkre čiam ųjų lig ų katedra CONTENTS Introduction ……………………………………………………………………………………… 7 SECTION I. Lecture notes ………………………………………………………………………. 8 1. GENERAL VETERINARY TOXICOLOGY ……….……………………………………….. 8 1.1. Veterinary toxicology aims and tasks ……………………………………………………... 8 1.2. EC and Lithuanian legal documents for hazardous substances and pollution ……………. 11 1.3. Classification of poisons ……………………………………………………………………. 12 1.4. Chemicals classification and labelling ……………………………………………………… 14 2. Toxicokinetics ………………………………………………………………………...………. 15 2.2. Migration of substances through biological membranes …………………………………… 15 2.3. ADME notion ………………………………………………………………………………. 15 2.4. Possibilities of poisons entering into an animal body and methods of absorption ……… 16 2.5. Poison distribution -

Ants in the Home Fact Sheet No
Ants in the Home Fact Sheet No. 5.518 Insect Series|Home and Garden by W.S. Cranshaw* Almost anywhere in the state one the nest, tend the young and do other Quick Facts travels, ants will be the most common necessary colony duties. Many kinds of insects that can be found in yards, gardens, ants produce workers that are all the • Most ants that are found in fields and forests. Tremendous numbers same size (monomorphic); some, such as homes nest outdoors and of ants normally reside in a typical house field ants, have workers that vary in size enter homes only to search lot, although most lead unobserved lives (polymorphic). for food or water. underground or otherwise out of sight. Each colony contains one or, sometimes, Often it is only when they occur indoors or a few queens (Figure 1). These are fertile • Almost all ants are workers, produce their periodic mating swarms that females that are larger than workers and wingless females that search they come to human attention. dedicated to egg production. The minute for food and maintain the Overall, the activities of ants are quite eggs are taken from the queen and tended colony. beneficial. Many feed on other insects, by the workers. Upon egg hatch, the • A small proportion of an including pest insects. Ant scavenging pale-colored, legless larvae are fed and helps to recycle organic matter and their protected by the workers. When full-grown, ant colony are winged tunneling is useful in aerating and mixing ant larvae produce a smooth silken cocoon reproductive forms. -

Transfer of Ingested Insecticides Among Cockroaches: Effects of Active Ingredient, Bait Formulation, and Assay Procedures
HOUSEHOLD AND STRUCTURAL INSECTS Transfer of Ingested Insecticides Among Cockroaches: Effects of Active Ingredient, Bait Formulation, and Assay Procedures 1 2 1, 3 GRZEGORZ BUCZKOWSKI, ROBERT J. KOPANIC, JR., AND COBY SCHAL J. Econ. Entomol. 94(5): 1229Ð1236(2001) ABSTRACT Foraging cockroaches ingest insecticide baits, translocate them, and can cause mor- tality in untreated cockroaches that contact the foragers or ingest their excretions. Translocation of eight ingested baits by adult male Blattella germanica (L.) was examined in relation to the type of the active ingredient, formulation, and foraging area. Ingested boric acid, chlorpyrifos, Þpronil, and hydramethylnon that were excreted by adults in small dishes killed 100% of Þrst instars within 10 d and Ͼ50% of second instars within 14 d. Residues from these ingested baits were also highly effective on nymphs in larger arenas and killed 16Ð100% of the adults. However, when the baits and dead cockroaches were removed from the large arenas and replaced with new cockroaches, only residues of the slow-acting hydramethylnon killed most of the nymphs and adults, whereas residues of fast acting insecticides (chlorpyrifos and Þpronil) killed fewer nymphs and adults. Excretions from cockroaches that ingested abamectin baits failed to cause signiÞcant mortality in cockroaches that contacted the residues. These results suggest that hydramethylnon is highly effective in these assays because cockroaches that feed on the bait have ample time to return to their shelter and defecate insecticide-laden feces. The relatively high concentration of hydramethylnon in the bait (2.15%) and its apparent stability in the digestive tract and feces probably contribute to the efÞcacy of hydra- methylnon. -

The Veterinarian's Guide
The Veterinarian’s Guide Bromethalin Addendum The Soft Bait Innovators™ Liphatech, Inc. • 3600 W. Elm Street • Milwaukee, WI 53209 • 1-888-331-7900 • www.liphatech.com NOTE: The information in this guide does not represent labeling and does not replace information on rodenticide labels relating to exposure of non-target species. Please read and follow all label directions on all rodenticide products you are using. Mentions of trade names in this publication does not imply endorsement of these products. Assault® is a registered trademark of PM Resources (St. Louis, MO) TakeDown™ and Cannon™ are trademarks of Liphatech, Inc. (Milwaukee, WI) Gunslinger® is a registered trademark of Liphatech, Inc. (Milwaukee, WI) Fastrac® is a registered trademark of Bell Labs (Madison, WI) Top Gun™ is a trademark of JT Eaton (Twinsburg, OH) Tomcat® and Rampage® are registered trademarks of Motomco (Madison, WI) Trounce® is a registered trademark of Agricultural Feeds (St. Louis, MO) At the time of this printing all information was deemed accurate and reliable. Liphatech, Inc. 3600 W. Elm Street Milwaukee, WI 53209 1-888-331-7900 www.liphatech.com October, 2016 The Veterinarian’s Guide - Bromethalin Addendum The Veterinarian’s Guide to Accidental Rodenticide Ingestion by Dogs and Cats focuses on anticoagulants. This addendum is intended to help veterinarians recognize and treat the symptoms of bromethalin toxicity in domestic animals. It describes bromethalin’s mode of action and how it is used as a rodenticide. In addition to reviewing the symptoms of bromethalin poisoning in domestic animals and the acute toxicity levels for dogs and cats (Table 5), we have also included the American Society for Prevention of Cruelty to Animals’ Animal Poison Control Center (ASPCA APCC) recommendations for decontamination (Tables 6 and 7). -
Bromethalin Ingestion
PEEER REVR IEWEWED PRACTICAL TOXICOLOGY The Decontamination Dilemma: Bromethalin Ingestion Renee Tourdot, DVM, ASPCA Animal Poison Control Center shutterstock.com/Ysbrand Cosijn Bromethalin-based rodenticide bait exposures have become increasingly common since the Welcome to Practical Toxicology, brought to you in 1 partnership between Today’s Veterinary Practice and product became available in 1985. In 2015, the ASPCA Animal Poison Control Center (APCC) the American Society for the Prevention of (www.aspcapro.org/poison). This column provides practical clinical information about diagnosing and Cruelty to Animals Animal Poison Control treating pets that have been exposed to potentially Center received 2791 calls regarding exposures harmful substances. to bromethalin-based rodenticides.2 The APCC: • Provides 24-hour diagnostic and treatment Exposures to this toxin present a unique challenge recommendations by specially trained veterinary to clinicians. Once signs of convulsant syndrome—a toxicologists neurologic syndrome caused by bromethalin • Protects and improves animal lives through toxicology toxicosis—have developed, prognosis for recovery is education, consulting services, and case data review poor.3,4 Therefore, most clinicians seem aware that • Developed and maintains AnTox, an animal toxicology database system that identifies and characterizes prompt and aggressive decontamination measures toxic effects of substances in animals must be taken. However, if decontamination • Works closely with human poison control centers to is too aggressive, iatrogenic hypernatremia can provide animal poisoning information develop, and clinical hypernatremia can be just as • Offers extensive veterinary life-threatening as a large bromethalin exposure. toxicology consulting to organizations in industry, government, and agriculture. To further complicate matters, clinical signs of hypernatremia can appear similar to the neurologic If treating a patient that 5 requires emergency care for signs caused by bromethalin. -

RRAC Guidelines on Anticoagulant Rodenticide Resistance Management Editor: Rodenticide Resistance Action Committee (RRAC) of Croplife International Aim
RRAC guidelines on Anticoagulant Rodenticide Resistance Management Editor: Rodenticide Resistance Action Committee (RRAC) of CropLife International Aim This document provides guidance to advisors, national authorities, professionals, practitioners and others on the nature of anticoagulant resistance in rodents, the identification of anticoagulant resistance, strategies for rodenticide application that will avoid the development of resistance and the management of resistance where it occurs. The Rodenticide Resistance Action Committee (RRAC) is a working group within the framework of CropLife International. Participating companies include: Bayer CropScience, BASF, LiphaTech S. A., PelGar, Rentokil Initial, Syngenta and Zapi. Senior technical specialists, with specific expertise in rodenticides, represent their companies on this committee. The RRAC is grateful to the following co-authors: Stefan Endepols, Alan Buckle, Charlie Eason, Hans-Joachim Pelz, Adrian Meyer, Philippe Berny, Kristof Baert and Colin Prescott. Photos provided by Stefan Endepols. Contents 1. Introduction ............................................................................................................................................................................................................. 2 2. Classification and history of rodenticide compounds ..............................................................................................3 3. Mode of action of anticoagulant rodenticides, resistance mechanisms, and resistance mutations ......................................................................................................6