Keratin 1 Maintains Skin Integrity and Participates in an Inflammatory
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Cell Line P53 Mutation Type UM
A Cell line p53 mutation Type UM-SCC 1 wt UM-SCC5 Exon 5, 157 GTC --> TTC Missense mutation by transversion (Valine --> Phenylalanine UM-SCC6 wt UM-SCC9 wt UM-SCC11A wt UM-SCC11B Exon 7, 242 TGC --> TCC Missense mutation by transversion (Cysteine --> Serine) UM-SCC22A Exon 6, 220 TAT --> TGT Missense mutation by transition (Tyrosine --> Cysteine) UM-SCC22B Exon 6, 220 TAT --> TGT Missense mutation by transition (Tyrosine --> Cysteine) UM-SCC38 Exon 5, 132 AAG --> AAT Missense mutation by transversion (Lysine --> Asparagine) UM-SCC46 Exon 8, 278 CCT --> CGT Missense mutation by transversion (Proline --> Alanine) B 1 Supplementary Methods Cell Lines and Cell Culture A panel of ten established HNSCC cell lines from the University of Michigan series (UM-SCC) was obtained from Dr. T. E. Carey at the University of Michigan, Ann Arbor, MI. The UM-SCC cell lines were derived from eight patients with SCC of the upper aerodigestive tract (supplemental Table 1). Patient age at tumor diagnosis ranged from 37 to 72 years. The cell lines selected were obtained from patients with stage I-IV tumors, distributed among oral, pharyngeal and laryngeal sites. All the patients had aggressive disease, with early recurrence and death within two years of therapy. Cell lines established from single isolates of a patient specimen are designated by a numeric designation, and where isolates from two time points or anatomical sites were obtained, the designation includes an alphabetical suffix (i.e., "A" or "B"). The cell lines were maintained in Eagle's minimal essential media supplemented with 10% fetal bovine serum and penicillin/streptomycin. -

Study for Pathogenesis of Congenital Cholesteatoma with Comparison of Proteins Expressed in Congenital Cholesteatoma, Acquired C
Study for pathogenesis of congenital cholesteatoma with comparison of proteins expressed in congenital cholesteatoma, acquired cholesteatoma and skin of the external auditory canal through proteomics Seung Ho Shin Department of Medicine The Graduate School, Yonsei University Study for pathogenesis of congenital cholesteatoma with comparison of proteins expressed in congenital cholesteatoma, acquired cholesteatoma and skin of the external auditory canal through proteomics Directed by Professor Jae Young Choi The Doctoral Dissertation submitted to the Department of Medicine, the Graduate School of Yonsei University in partial fulfillment of the requirements for the degree of Doctor of Philosophy Seung Ho Shin June 2014 ACKNOWLEDGEMENTS In the initial period of my fellowship, I wrote a book, Temporal Bone Dissection Manual as a coauthor with Professor Won Sang Lee, Ho-Ki Lee and Jae Young Choi. Through this book, I learned about much knowledge from them. Professor Jae Young Choi advised me to go for a Ph.D. I admitted graduate school for a Ph.D. in 2007. In my doctoral course, he has instructed me in detail on the basic research. He has demonstrated precise and delicate laboratory techniques and showed outstanding ability to create new ideas. Also, he has often said to me that a researcher must be honest to his colleagues and even to himself. After the summer of 2013, he gave me an idea for this paper, which was for congenital cholesteatoma analysis with proteomics. He always displayed endless energy and enthusiasm for scientific experiments even after many demanding surgeries. His passion motivated me to follow suit and seven months of our work at last bore fruit. -

Spiny Mice (Acomys) Exhibit Attenuated Hallmarks of Aging And
bioRxiv preprint doi: https://doi.org/10.1101/2020.05.07.083287; this version posted May 10, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 2 3 4 5 6 Title: Spiny mice (Acomys) exhibit attenuated hallmarks of aging and rapid cell turnover after UV 7 exposure in the skin epidermis 8 Authors: Wesley Wong1, Austin Kim1, Ashley W. Seifert2, Malcolm Maden3, and Justin D. Crane1 9 Affiliations: 1Department of Biology, Northeastern University, 360 Huntington Avenue, Boston, 10 MA 02115, 2Department of Biology, University of Kentucky, Lexington, KY 40506, 3UF 11 Genetics Institute & Department of Biology, University of Florida, Gainesville, FL 32611 12 13 Keywords: Spiny mouse, skin, epidermis, UV radiation, aging 14 15 16 17 18 19 20 21 22 23 24 25 26 27 bioRxiv preprint doi: https://doi.org/10.1101/2020.05.07.083287; this version posted May 10, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 28 Abstract 29 The study of long-lived and regenerative animal models has revealed diverse protective responses 30 to stressors such as aging and tissue injury. Spiny mice (Acomys) are a unique mammalian model 31 of skin regeneration, but their response to other types of physiological skin damage have not been 32 investigated. -

Structural Heterogeneity of Cellular K5/K14 Filaments As Revealed by Cryo
bioRxiv preprint doi: https://doi.org/10.1101/2021.05.12.442145; this version posted May 14, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 Structural heterogeneity of cellular K5/K14 filaments as revealed by cryo- 2 electron microscopy 3 4 Short title: Structural heterogeneity of keratin filaments 5 6 7 Miriam S. Weber1, Matthias Eibauer1, Suganya Sivagurunathan2, Thomas M. Magin3, Robert D. 8 Goldman2, Ohad Medalia1* 9 1Department of Biochemistry, University of Zurich, Switzerland 10 2Department of Cell and Developmental Biology, Northwestern University Feinberg School of 11 Medicine, USA 12 3Institute of Biology, University of Leipzig, Germany 13 14 * Corresponding author: [email protected] 15 16 1 bioRxiv preprint doi: https://doi.org/10.1101/2021.05.12.442145; this version posted May 14, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 17 Abstract 18 Keratin intermediate filaments are an essential and major component of the cytoskeleton in epithelial 19 cells. They form a stable yet dynamic filamentous network extending from the nucleus to the cell 20 periphery. Keratin filaments provide cellular resistance to mechanical stresses, ensure cell and tissue 21 integrity in addition to regulatory functions. Mutations in keratin genes are related to a variety of 22 epithelial tissue diseases that mostly affect skin and hair. Despite their importance, the molecular 23 structure of keratin filaments remains largely unknown. In this study, we analyzed the structure of 24 keratin 5/keratin 14 filaments within ghost keratinocytes by cryo-electron microscopy and cryo- 25 electron tomography. -

P63 Transcription Factor Regulates Nuclear Shape and Expression of Nuclear Envelope
Durham Research Online Deposited in DRO: 21 September 2017 Version of attached le: Published Version Peer-review status of attached le: Peer-reviewed Citation for published item: Rapisarda, Valentina and Malashchuk, Igor and Asamaowei, Inemo E. and Poterlowicz, Krzysztof and Fessing, Michael Y. and Sharov, Andrey A. and Karakesisoglou, Iakowos and Botchkarev, Vladimir A. and Mardaryev, Andrei (2017) 'p63 transcription factor regulates nuclear shape and expression of nuclear envelope-associated genes in epidermal keratinocytes.', Journal of investigative dermatology., 137 (10). pp. 2157-2167. Further information on publisher's website: https://doi.org/10.1016/j.jid.2017.05.013 Publisher's copyright statement: This article is available under the terms of the Creative Commons Attribution License (CC BY). You may copy and distribute the article, create extracts, abstracts and new works from the article, alter and revise the article, text or data mine the article and otherwise reuse the article commercially (including reuse and/or resale of the article) without permission from Elsevier. You must give appropriate credit to the original work, together with a link to the formal publication through the relevant DOI and a link to the Creative Commons user license above. You must indicate if any changes are made but not in any way that suggests the licensor endorses you or your use of the work. Additional information: Use policy The full-text may be used and/or reproduced, and given to third parties in any format or medium, without prior permission or charge, for personal research or study, educational, or not-for-prot purposes provided that: • a full bibliographic reference is made to the original source • a link is made to the metadata record in DRO • the full-text is not changed in any way The full-text must not be sold in any format or medium without the formal permission of the copyright holders. -

ITRAQ-Based Quantitative Proteomic Analysis of Processed Euphorbia Lathyris L
Zhang et al. Proteome Science (2018) 16:8 https://doi.org/10.1186/s12953-018-0136-6 RESEARCH Open Access ITRAQ-based quantitative proteomic analysis of processed Euphorbia lathyris L. for reducing the intestinal toxicity Yu Zhang1, Yingzi Wang1*, Shaojing Li2*, Xiuting Zhang1, Wenhua Li1, Shengxiu Luo1, Zhenyang Sun1 and Ruijie Nie1 Abstract Background: Euphorbia lathyris L., a Traditional Chinese medicine (TCM), is commonly used for the treatment of hydropsy, ascites, constipation, amenorrhea, and scabies. Semen Euphorbiae Pulveratum, which is another type of Euphorbia lathyris that is commonly used in TCM practice and is obtained by removing the oil from the seed that is called paozhi, has been known to ease diarrhea. Whereas, the mechanisms of reducing intestinal toxicity have not been clearly investigated yet. Methods: In this study, the isobaric tags for relative and absolute quantitation (iTRAQ) in combination with the liquid chromatography-tandem mass spectrometry (LC-MS/MS) proteomic method was applied to investigate the effects of Euphorbia lathyris L. on the protein expression involved in intestinal metabolism, in order to illustrate the potential attenuated mechanism of Euphorbia lathyris L. processing. Differentially expressed proteins (DEPs) in the intestine after treated with Semen Euphorbiae (SE), Semen Euphorbiae Pulveratum (SEP) and Euphorbiae Factor 1 (EFL1) were identified. The bioinformatics analysis including GO analysis, pathway analysis, and network analysis were done to analyze the key metabolic pathways underlying the attenuation mechanism through protein network in diarrhea. Western blot were performed to validate selected protein and the related pathways. Results: A number of differentially expressed proteins that may be associated with intestinal inflammation were identified. -
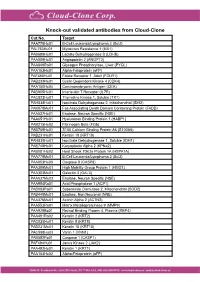
Knock-Out Validated Antibodies from Cloud-Clone Cat.No
Knock-out validated antibodies from Cloud-Clone Cat.No. Target PAA778Hu01 B-Cell Leukemia/Lymphoma 2 (Bcl2) PAL763Hu01 Myxovirus Resistance 1 (MX1) PAB698Hu01 Lactate Dehydrogenase B (LDHB) PAA009Hu01 Angiopoietin 2 (ANGPT2) PAA849Ra01 Glycogen Phosphorylase, Liver (PYGL) PAA153Hu01 Alpha-Fetoprotein (aFP) PAF460Hu01 Folate Receptor 1, Adult (FOLR1) PAB233Hu01 Cyclin Dependent Kinase 4 (CDK4) PAA150Hu04 Carcinoembryonic Antigen (CEA) PAB905Hu01 Interleukin 7 Receptor (IL7R) PAC823Hu01 Thymidine Kinase 1, Soluble (TK1) PAH838Hu01 Isocitrate Dehydrogenase 2, mitochondrial (IDH2) PAK078Mu01 Fas Associating Death Domain Containing Protein (FADD) PAA537Hu01 Enolase, Neuron Specific (NSE) PAA651Hu01 Hyaluronan Binding Protein 1 (HABP1) PAB215Hu02 Fibrinogen Beta (FGb) PAB769Hu01 S100 Calcium Binding Protein A6 (S100A6) PAB231Hu01 Keratin 18 (KRT18) PAH839Hu01 Isocitrate Dehydrogenase 1, Soluble (IDH1) PAE748Hu01 Karyopherin Alpha 2 (KPNa2) PAB081Hu02 Heat Shock 70kDa Protein 1A (HSPA1A) PAA778Mu01 B-Cell Leukemia/Lymphoma 2 (Bcl2) PAA853Hu03 Caspase 8 (CASP8) PAA399Mu01 High Mobility Group Protein 1 (HMG1) PAA303Mu01 Galectin 3 (GAL3) PAA537Mu02 Enolase, Neuron Specific (NSE) PAA994Ra01 Acid Phosphatase 1 (ACP1) PAB083Ra01 Superoxide Dismutase 2, Mitochondrial (SOD2) PAB449Mu01 Enolase, Non Neuronal (NNE) PAA376Mu01 Actinin Alpha 2 (ACTN2) PAA553Ra01 Matrix Metalloproteinase 9 (MMP9) PAA929Bo01 Retinol Binding Protein 4, Plasma (RBP4) PAA491Ra02 Keratin 2 (KRT2) PAC025Hu01 Keratin 8 (KRT8) PAB231Mu01 Keratin 18 (KRT18) PAC598Hu03 Vanin 1 (VNN1) -

Keratins Couple with the Nuclear Lamina and Regulate Proliferation in Colonic Epithelial Cells Carl-Gustaf A
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.22.164467; this version posted June 22, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Keratins couple with the nuclear lamina and regulate proliferation in colonic epithelial cells Carl-Gustaf A. Stenvall1*, Joel H. Nyström1*, Ciarán Butler-Hallissey1,5, Stephen A. Adam2, Roland Foisner3, Karen M. Ridge2, Robert D. Goldman2, Diana M. Toivola1,4 1 Cell Biology, Biosciences, Faculty of Science and Engineering, Åbo Akademi University, Turku, Finland 2 Department of Cell and Developmental Biology, Feinberg School of Medicine, Northwestern University, Chicago, Illinois, USA 3 Max Perutz Labs, Medical University of Vienna, Vienna Biocenter Campus (VBC), Vienna, Austria 4 Turku Center for Disease Modeling, Turku, Finland 5 Turku Bioscience Centre, University of Turku and Åbo Akademi University, Turku, Finland * indicates equal contribution Running Head: Colonocyte keratins couple to nuclear lamina Corresponding author: Diana M. Toivola Cell Biology/Biosciences, Faculty of Science and Engineering, Åbo Akademi University Tykistökatu 6A, FIN-20520 Turku, Finland Telephone: +358 2 2154092 E-mail: [email protected] Keywords: Keratins, lamin, intermediate filament, colon epithelial cells, LINC proteins, proliferation, pRb, YAP bioRxiv preprint doi: https://doi.org/10.1101/2020.06.22.164467; this version posted June 22, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -

Proteomics in Forensic Analysis: Applications for Human Samples
applied sciences Review Proteomics in Forensic Analysis: Applications for Human Samples Van-An Duong 1,† , Jong-Moon Park 1,† , Hee-Joung Lim 2,* and Hookeun Lee 1,* 1 College of Pharmacy, Gachon University, Incheon 21936, Korea; [email protected] (V.-A.D.); [email protected] (J.-M.P.) 2 Forensic Science Center for Odor Fingerprint Analysis, Police Science Institute, Korean National Police University, Asan 31539, Korea * Correspondence: [email protected] (H.-J.L.); [email protected] (H.L.); Tel.: +82-41-968-2893 (H.-J.L.); +82-32-820-4927 (H.L.) † These authors contributed equally. Abstract: Proteomics, the large-scale study of all proteins of an organism or system, is a powerful tool for studying biological systems. It can provide a holistic view of the physiological and biochemical states of given samples through identification and quantification of large numbers of peptides and proteins. In forensic science, proteomics can be used as a confirmatory and orthogonal technique for well-built genomic analyses. Proteomics is highly valuable in cases where nucleic acids are absent or degraded, such as hair and bone samples. It can be used to identify body fluids, ethnic group, gender, individual, and estimate post-mortem interval using bone, muscle, and decomposition fluid samples. Compared to genomic analysis, proteomics can provide a better global picture of a sample. It has been used in forensic science for a wide range of sample types and applications. In this review, we briefly introduce proteomic methods, including sample preparation techniques, data acquisition using liquid chromatography-tandem mass spectrometry, and data analysis using database search, Citation: Duong, V.-A.; Park, J.-M.; spectral library search, and de novo sequencing. -

Supplementary Material Contents
Supplementary Material Contents Immune modulating proteins identified from exosomal samples.....................................................................2 Figure S1: Overlap between exosomal and soluble proteomes.................................................................................... 4 Bacterial strains:..............................................................................................................................................4 Figure S2: Variability between subjects of effects of exosomes on BL21-lux growth.................................................... 5 Figure S3: Early effects of exosomes on growth of BL21 E. coli .................................................................................... 5 Figure S4: Exosomal Lysis............................................................................................................................................ 6 Figure S5: Effect of pH on exosomal action.................................................................................................................. 7 Figure S6: Effect of exosomes on growth of UPEC (pH = 6.5) suspended in exosome-depleted urine supernatant ....... 8 Effective exosomal concentration....................................................................................................................8 Figure S7: Sample constitution for luminometry experiments..................................................................................... 8 Figure S8: Determining effective concentration ......................................................................................................... -

Supplementary Figure 1
Supplementary Figure 1 A Cisplatin Cisplatin Cisplatin Late resistance Sensitive cells Early resistance (H357CisR8M) (H357CisS) (H357CisR4M) B SCC-4 CisS SCC9 CisS H357 CisS SCC-4 CisR 4M SCC9 CisR 4M 120 120 H357 CisR 4M SCC4 CisR 8M * H357 CisR 8M 120 SCC9 CisR 8M 100 * * * * 100 * * * * * 100 * * * * * * * * * * * * * * 80 * 80 * 80 60 60 60 40 40 40 % of cell viability of cell % % of cell viability of cell % 20 ofviability cell % 20 20 0 0 0 5 1 5 10 15 20 25 30 35 40 1 5 2.5 7.5 10 15 20 25 30 35 40 2.5 7.5 2.5 7.5 10 15 20 25 30 35 12.5 12.5 DMSO DMSO DMSO Cisplatin (M) Cisplatin (M) Cisplatin (M) C 100 100 80 80 60 60 40 A375 CisS 40 A549 CisS A549 CisR A375 CisR % of cell viability of cell % 20 % ofviability cell % 20 0 0 1 2 3 4 5 6 8 10 12 14 16 18 20 25 30 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 DMSO Cisplatin (M) DMSO Cisplatin (M) Supplementary figure 1: Characterization of sensitive, early and late cisplatin resistant lines: A) Schematic presentation of establishing sensitive, early and late cisplatin resistant cancer lines B) Sensitive, early and late cisplatin resistant pattern (CisS, CisR4M and CisR8M) of H357, SCC9 and SCC4 cells were treated with indicated concentrations of cisplatin for 48h and cell viability was determined by MTT assay (n=3, *: P < 0.05). C) Sensitive and late cisplatin resistant lung cancer (A549) and melanoma (A375) lines were established as described in method section. -
Impact of Keratin Network Regulation on Migrating Cells
Impact of Keratin Network Regulation on Migrating Cells Von der Fakultät für Mathematik, Informatik und Naturwissenschaften der RWTH Aachen University zur Erlangung des akademischen Grades eines Doktors der Naturwissenschaften genehmigte Dissertation vorgelegt von Anne Pora, Ingénieur, Master aus Rueil-Malmaison, Frankreich Berichter: Univ.-Prof. Dr. Björn Kampa Univ.-Prof. Dr. med. Rudolf Leube Tag der mündlichen Prüfung: 02.04.19 Diese Dissertation ist auf den Internetseiten der Universitätsbibliothek verfügbar. This work was performed at the Institute for Molecular and Cellular Anatomy at University Hospital RWTH Aachen by the mentorship of Prof. Dr. med. Rudolf E. Leube. It was exclusively performed by myself, unless otherwise stated in the text. 1. Reviewer: Univ.-Prof. Dr. Björn Kampa 2. Reviewer: Univ.-Prof. Dr. med. Rudolf E. Leube Toulouse (FR), 30.11.18 2 Table of Contents Table of Contents 3 Chapter 1: Introduction 6 1. Cell migration 6 A key process in physiological and pathological conditions 6 Different kinds of migration 6 Influence of the environment 7 2. The cytoskeleton: a key player in cell migration 9 The cytoskeleton 9 Actin and focal adhesions 9 Microtubules 12 Keratin intermediate filaments and hemidesmosomes 13 Cross-talk between keratin intermediate filaments and others 22 cytoskeletal components Imaging cytoskeletal dynamics in migrating cells 24 3. Objectives 26 Chapter 2: Materials and Methods 27 1. Cell culture conditions 27 2. Keratin extraction and immunoblotting 28 3. Immunofluorescence 32 4. Plasmid constructs and DNA transfection into cultured cells 34 5. Drug treatments 35 6. Micropatterning 35 7. Preparation of elastic substrates 36 8. Imaging conditions 36 3 9.