National Preparedness and Response Plan for COVID
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gross National Happiness Commission the Royal Government of Bhutan
STRATEGIC PROGRAMME FOR CLIMATE RESILIENCE (SPCR) UNDER THE PILOT PROGRAMME FOR CLIMATE RESILIENCE (PPCR) Climate-Resilient & Low-Carbon Sustainable Development Toward Maximizing the Royal Government of Bhutan’s Gross National Happiness GROSS NATIONAL HAPPINESS COMMISSION THE ROYAL GOVERNMENT OF BHUTAN FOREWORD The Royal Government of Bhutan (RGoB) recognizes the devastating impact that climate change is having on Bhutan’s economy and our vulnerable communities and biosphere, and we are committed to address these challenges and opportunities through the 12th Five Year Plan (2018-2023). In this context, during the 2009 Conference of the Parties 15 (COP 15) in Copenhagen, RGoB pledged to remain a carbon-neutral country, and has successfully done so. This was reaffirmed at the COP 21 in Paris in 2015. Despite being a negative-emission Least Developed Country (LDC), Bhutan continues to restrain its socioeconomic development to maintain more than 71% of its geographical area under forest cover,1 and currently more than 50% of the total land area is formally under protected areas2, biological corridors and natural reserves. In fact, our constitutional mandate declares that at least 60% of Bhutan’s total land areas shall remain under forest cover at all times. This Strategic Program for Climate Resilience (SPCR) represents a solid framework to build the climate- resilience of vulnerable sectors of the economy and at-risk communities across the country responding to the priorities of NDC. It also offers an integrated story line on Bhutan’s national -

Royal Government of Bhutan Ministry of Finance
ROYAL GOVERNMENT OF BHUTAN MINISTRY OF FINANCE COMPENSATION RATES - 2017 DEPARTMENT OF NATIONAL PROPERTIES PROPERTY ASSESSMENT AND VALUATION AGENCY C O N T E N T S Sl. No. P A R T I C U L A R S Page No. 1. A – Rural Land Compensation Rates 2017 a) Kamzhing (Dry Land) 1 b) Chhuzhing (Wet land) 2 c) Ngultho Dumra (Cash Crop Land) 3 d) Class A1(Land close to Thromde) 4 2. Factors determining Rural Land Compensation 5 3. B – Urban Land Compensation Rates 2017 a) Thimphu Thromde 6 b) Phuntsholing Thromde 7 c) Gelephu Thromde 8 d) Samdrup Jongkhar Thromde 9 e) Samtse Thromde 10 f) Damphu Throm de 11 g) Rest of the Dzongkhag Thromdes 12 h) Yenlag Thromdes 13 i) Sarpang Yenlag Thromde 14 j) Duksum Yenlag Thromde 15 k) Specific Towns 15 4. Factors determining Urban Land Compensation 15 5. Guideline on Compensation rate for building 16 6. Implementation Procedure 16 7. C – Agricultural Compensation Rates 2017 a. Compensation Rates for Fruit Trees 17 b. Compensation Rate for Developed Pasture 18 c. Compensation Rate for Fodder Trees 18 d. Land Development Cost of Chhuzhing 18 e. Formula for working out Compensation of Forest Trees 18 8. Format for Rural Land Valuation 19 9. Format for Urban Land Valuation 20 ROYAL GOVERNMENT OF BHUTAN MINISTRY OF FINANCE Department of National Properties Property Assessment & Valuation Agency A - Rural Land Compensation Rates 2017 (a) For Rural Kamzhing Land Amount Nu./decimal Sl. No. Dzongkhag Class A Class B Class C 1 Bumthang 9,130.90 6,391.63 3,852.13 2 Chhukha 6,916.18 4,841.33 3,112.89 3 Dagana 5,538.22 3,876.75 -
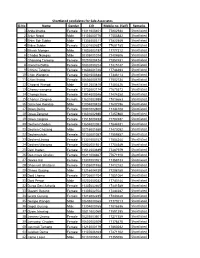
Shortlisted 41 Batch
Shortlisted candidates for Sale Associates Sl.No Name Gender CID Mobile no. (Self) Remarks 1 Anita kharka Female 11311000401 77802934 Shortlisted 2 Arjun Nepal Male 11103000776 17553882 Shortlisted 3 Bhim Bdr Subba Male 11304000311 77822549 Shortlisted 4 Bidya Subba Female 10301000657 77691785 Shortlisted 5 Bikash Monger Male 11802002197 17777312 Shortlisted 6 Chador Namgay Male 10305001074 77404606 Shortlisted 7 Chaisang Tamang Female 10201000424 77857481 Shortlisted 8 chencho Bidha Female 10802000224 17425147 Shortlisted 9 Chhimi Tshomo Female 11604001748 17746393 Shortlisted 10 Chim Wangmo Female 11601000388 17346113 Shortlisted 11 Chimi lhamo Female 10606000570 17502734 Shortlisted 12 Chogyal Wangdi Male 11512003810 17453426 Shortlisted 13 Choney wangmo Female 11703002174 77675573 Shortlisted 14 Chonga lham Female 11914000346 17474358 Shortlisted 15 Chorten Zangmo Female 11601002959 17816663 Shortlisted 16 Damchoe lhendup Male 12004000428 17607296 Shortlisted 17 Dawa Dema Female 10801002800 17344108 Shortlisted 18 Dawa Zangmo Female 11601002980 17457860 Shortlisted 19 Dawa zangmo Female 11513000453 77704937 Shortlisted 20 Dechen Choden Female 11604002052 17844531 Shortlisted 21 Dechen Chozang Male 10715001580 17473092 Shortlisted 22 Dechen chuki Female 10102001057 17559857 Shortlisted 23 Dechen Lhamo Female 11301000747 17504244 Shortlisted 24 Dechen Wangmo Female 10902001921 17704549 Shortlisted 25 Deki lhaden Female 11512003689 77487979 Shortlisted 26 Deo maya Ghalley Female 10211004667 77671910 Shortlisted 27 Devika Rai Female 11307003761 -

Farming and Biodiversity of Pigs in Bhutan
Animal Genetic Resources, 2011, 48, 47–61. © Food and Agriculture Organization of the United Nations, 2011 doi:10.1017/S2078633610001256 Farming and biodiversity of pigs in Bhutan K. Nidup1,2, D. Tshering3, S. Wangdi4, C. Gyeltshen5, T. Phuntsho5 and C. Moran1 1Centre for Advanced Technologies in Animal Genetics and Reproduction (REPROGEN), Faculty of Veterinary Science, University of Sydney, Australia; 2College of Natural Resources, Royal University of Bhutan, Lobesa, Bhutan; 3Department of Livestock, National Pig Breeding Centre, Ministry of Agriculture, Thimphu, Bhutan; 4Department of Livestock, Regional Pig and Poultry Breeding Centre, Ministry of Agriculture, Lingmithang, Bhutan; 5Department of Livestock, Regional Pig and Poultry Breeding Centre, Ministry of Agriculture, Gelephu, Bhutan Summary Pigs have socio-economic and cultural importance to the livelihood of many Bhutanese rural communities. While there is evidence of increased religious disapproval of pig raising, the consumption of pork, which is mainly met from imports, is increasing every year. Pig development activities are mainly focused on introduction of exotic germplasm. There is an evidence of a slow but steady increase in the population of improved pigs in the country. On the other hand, indigenous pigs still comprise 68 percent of the total pig population but their numbers are rapidly declining. If this trend continues, indigenous pigs will become extinct within the next 10 years. Once lost, this important genetic resource is largely irreplaceable. Therefore, Government of Bhutan must make an effort to protect, promote and utilize indigenous pig resources in a sustainable manner. In addition to the current ex situ conservation programme based on cryopre- servation of semen, which needs strengthening, in situ conservation and a nucleus farm is required to combat the enormous decline of the population of indigenous pigs and to ensure a sustainable source of swine genetic resources in the country. -

21 Indian Nationals Among the 187 Total Covid-19 Cases in the Country
SATURDAY KUENSELTHAT THE PEOPLE SHALL BE INFORMED AUGUST 29" ( & ( & D k ' + COVID-19: Bhutan: 187 | Global: 24,605,229 | Recovered: 16,869,866 | Death: 834,771 | US: 6,046,060 ?dZ_W0)").*"+-+| West Bengal: 150,772 | Assam: 98,807 | Arunachal Pradesh: 3,633 | Sikkim: 1,542 MoE proposes to re-open classes IX to XII When lockdown ceases Yangchen C Rinzin The Ministry of Education has submitted a pro- posal to the Prime Minister to re-open Classes IX and XI along with Classes X and XII if the pandemic situation improves and the lockdown is lifted. Education Minister Jai Bir Rai told Kuensel that the proposal was readied before the na- tionwide lockdown came into force on August 11, as the ministry felt the need for face-face teaching. “But before the ministry could submit the proposal to the government, the nationwide lockdown was declared,” he said. Classes X and XII were re-opened before the From the recent mass surveillance: People queue up at Dhamdara for Covid-19 test Pg 15 lockdown in July. Regular classes for X and XII have been suspended following a nationwide lockdown on August 11. The minister said that the ministry is con- cerned, as the pandemic has affected students. We’re already noticing that closure of schools 21 Indian nationals among has impacted students and many students have also started losing interest in studies,” the minis- ter said. “We know that we’re not in a good situa- the 187 total Covid-19 tion, but we need to make a decision by keeping the virus at bay, as the trend is worrying.” Pg 2 cases in the country Younten Tshedup old man tested positive while in the the country of origin, anyone who is quarantine on August 22. -

The World Bank IMPLEMENTATION COMPLETION and RESULTS
Document of The World Bank FOR OFFICIAL USE ONLY Report No: ICR00004941 IMPLEMENTATION COMPLETION AND RESULTS REPORT IDA 47440 and 54310 (AF) ON A CREDIT IN THE AMOUNT OF SDR7.75 MILLION (US$12.0 MILLION EQUIVALENT) AND AN ADDITIONAL CREDIT IN THE AMOUNT OF SDR11.3 MILLION (US$17.4 MILLION EQUIVALENT) TO THE KINGDOM OF BHUTAN FOR THE SECOND URBAN DEVELOPMENT PROJECT DECEMBER 27, 2019 Urban, Resilience And Land Global Practice Sustainable Development South Asia Region CURRENCY EQUIVALENTS (Exchange Rate Effective November 27, 2019) Bhutanese Currency Unit = Ngultrum (BTN) BTN71.31 = US$1 US$1.37 = SDR 1 FISCAL YEAR July 1 - June 30 Regional Vice President: Hartwig Schafer Country Director: Mercy Miyang Tembon Regional Director: John A. Roome Practice Manager: Catalina Marulanda Task Team Leader(s): David Mason ICR Main Contributor: David Mason ABBREVIATIONS AND ACRONYMS ADB Asian Development Bank AF Additional Financing AHP Affected Households and Persons APA Alternative Procurement Arrangement BLSS Bhutan Living Standards Survey BTN Bhutanese Ngultrum BUDP-1 Bhutan Urban Development Project (Cr. 3310) BUDP-2 Second Bhutan Urban Development Project CAS Country Assistance Strategy CNDP Comprehensive National Development Plan CPF Country Partnership Framework CPLC Cash Payment in Lieu of Land Compensation CWSS Central Water Supply Scheme DAR Digital Asset Registry EMP Environmental Management Plan FM Financial Management FYP Five Year Plan GNHC Gross National Happiness Commission GRC Grievance Redress Committee GRM Grievance Redressal Mechanism -

Construction Development Board
LIST OF PARTICIPANTS FOR REFRESHER COURSE LARGE AND MEDIUM CONTRACTORS FROM 20th - 22nd JANUARY 2020 AT CST, PHUENTSHOLING CID/Work Permit No. Sl# CDB# Name of Firm Class Name of Participant of Participant KENCHO DORJI 1 1043 L Kencho Dorji 102022000997 Construction Private Limited 2 2631 YARKAY Construction L Geeta Gurung 11216001231 YANGKHIL Construction Private 3 2182 L Phuentsho T Norbu 10606001676 Limited DRUK KUNZANG 4 4060 L Passang Dorji 11402000211 Construction Pvt.Ltd LHENDUP NORBU 5 7030 L Sangay Norbu 11105002162 Construction 6 4181 Jadung Engineering Private Limited L Choki Mo 11703002492 7 1081 MINDU Construction Private Limited L Tashi Jigme 10803000757 DHODTER RIGTSEL 8 5116 L Karma tshomo 11101001199 Company Private Limited SONAM JAMTSHO & BROS 9 3248 L Sonam Jamtsho 10606001512 CONSTRUCTIONPVT. LTD. 10 1542 D Lhen Private Limited L Suman Chhetei 11202004922 11 1811 K.D Builders Private Limited L Sudesh Pradhan 11208004258 12 3206 BHUTAN Construction Private Limited L Ngawang Delkar 10711002326 PELJOR LHENDUP 13 6712 L Ugyen Tshewang 11605003208 Construction Private Limited Chaggwong Construction Private 14 1033 L Dechen Yangzom 12008002562 Limited 15 3531 YONGPHEL Builders M chophel 10703002484 16 2920 WANGMO Construction M Sanjana Darjee 10308003433 SANGAY THINLEY 17 1432 M Madan Ghalley 11303000869 Construction 18 1846 PEMA Construction M Pema Rinzin 11703001736 19 1757 CHETHUN Construction M Wangchuk 10603000362 20 3155 C.T Construction M Karma 11501001834 21 7276 DALA Construction M Dawa Tsirang 10807001643 K-RANGRIK 22 3061 M Tashi Choden 11505003436 Construction Company Private Limited 23 4074 2Q Engineering Works Private Limited M Kinzang Dorji 11803001018 RINZIN DORJI 24 1099 M Rinzin Dorji 10605000105 Construction 25 3447 SANGAY D Construction M Sangay Dema 11411000024 LHOJONG Construction Private 26 1862 M Kinley Om 11008000886 Limited 27 1994 LAMA Industry M Anil Lama 10308002127 28 7093 Bumzang Builders M Jangchub Yoeser 10701001503 29 8080 FANTHOG Builders M Pema Choney 12007001145 30 5747 Guardian Construction Pvt. -

Nepal & Bhutan
Nepal & Bhutan Nepal & Bhutan 10 days | Kathmandu to Kathmandu PRIVATE TOUR: Combine two What's Included Day 1 : Kathmandu Welcome to Nepal and the start of your beautiful Himalayan Kingdoms • 9 breakfasts, 5 lunches & 6 dinners holiday! Pick up and complete a landing card in one magical tour. Enter the including dinner at a Nepali cultural on the plane or in the airport before you go serene and spiritual lands of Nepal evening through customs. Upon arrival you will be met and Bhutan, and experience the • 4 nights standard hotel in Kathmandu, 5 by our representatives and transferred to your nights standard hotel/lodges in Bhutan countries' rich histories and unique hotel where you will receive a welcome drink • Airport arrival and departure transfers cultural heritages. From the brightly and a briefing about your trip. Overnight - • Return economy class return flight Kathmandu coloured fluttering prayer flags of Kathmandu - Paro - Kathmandu Nepal to the elaborate traditional • Guided sightseeing of Kathmandu and Day 2 : Pashupatinath Temple dress of the Bhutanese, these Bhutan as detailed in the itinerary captivating lands cannot fail to • Services of local English speaking tour enchant. guides • All entrance fees to included sites and monuments HIGHLIGHTS AND INCLUSIONS • Services of licensed Nepalese & Bhutanese English speaking tour guides Trip Highlights • All relevant transfers and transportation in • Kathmandu and the Kathmandu Valley - private vehicles Patan Durbar Square, Swayambhunath • Bhutan Visa fee and travel Permit Pagoda, Bodhnath Buddhist stupa and (excludes visa admin fee of USD$20 pp, Enjoy a full day of sightseeing in the various other temples and shrines payable upon arrival) Kathmandu Valley. -
Annual Report 2015-2016
Royal Civil Service Commission Annual Report 2015-2016 ANNUAL REPORT (July 2015 - June 2016) STATE OF THE ROYAL CIVIL SERVICE Royal Civil Service Commission ROYAL GOVERNMENT OF BHUTAN Excellence in Service i Royal Civil Service Commission Annual Report 2015-2016 Excellence in Service ii Excellence in Service Royal Civil Service Commissio n Annual Report 2015-2016 Royal Civil Service Commission Annual Report 2015-2016 Table of Contents List of Abbreviations ................................................................................................................................ i INTRODUCTION ......................................................................................................................................... 1 i. Scope of the Report .......................................................................................................................... 3 ii. Commission Mee ngs ....................................................................................................................... 3 iii. Representa on of Commission in Boards/Commi ees and Lead Role in Reforms ......................... 4 iv. Focal Commissioners for Agencies .................................................................................................... 4 v. Budget Report 2015-2016 ................................................................................................................. 5 PART 1: CIVIL SERVICE STATISTICS - KEY HIGHLIGHTS ....................................................................... 7 1.1 Civil -

The Executive
The Executive VOLUME I NOVEMBER 7, 2018 - NOVEMBER 7, 2019 YEAR IN OFFICE Laying foundation for change 1,000 Golden Days Plus Digital transformation Removal of “cut Teachers, the Narrowing gap Densa Meet: off” for Class X highest paid civil through pay the other servant revision Mines and Cabinet Minerals Bill AM with PM: Getting to know Revising Tourism policy 9 better Tariff revision Private sector Policies development approved committee Laying foundation for change “Climb higher on the shoulders of past achievements - your task is not to fill old shoes or follow a well-trodden path, but to forge a new road leading towards a brighter future.” His Majesty The King Royal Institute of Management August 9, 2019 Contents • Introduction 8 • From the Prime Minister 10 • Initiating change 13 • Country before party 14 • Revisiting our vision 15 • The 12th Plan is critical 18 • The Nine Thrusts 19 • Densa, the other Cabinet 22 • High value, low volume tourism 22 • More focus on health and education 24 • AM with PM: A dialogue with the Prime Minister 25 • Investing in our children 26 • Pay revised to close gap 27 • Rewarding the backbone of education 28 • Taking APA beyond formalities 29 • Block grant empowers LG 30 • Major tax reforms 30 • TVET transforms 31 • Cautious steps in hydro 32 • Encouraging responsible journalism 32 • Private sector-led economy 33 • Meeting pledges 34 • Policies Approved 36 • Guidelines reviewed and adopted 37 • Overhauling health 38 • A fair chance for every Bhutanese child 41 • Education comes first 42 • Grateful -

Statistical Information on Elections in Bhutan in Elections on Information Statistical Information on Elections in Bhutan (2006-2015)
STATISTICAL Statistical Information on Elections in Bhutan INFORMATION on Elections in Bhutan (2006-2015) www.election-bhutan.org.bt (2006-2015) Election Commission of Bhutan, Post Box No. 2008, Olakha, Thimphu, Bhutan Telephone: +975-02-334851/334852, Fax: +975-02-334763 Election Statistics (2006-2015) 2006-2015 Election Commi ssion of Bhutan 1 Election Statistics (2006-2015) © Election Commission of Bhutan No part of this book may be reproduced in any form. Anybody wishing to use the name, photo, cover design, part of material or thereof in any form of this book may do so with due permission or acknowledgement of the Election Commission of Bhutan. For any querry : [email protected] 2 Election Statistics (2006-2015) The Statistical Information on Elections in Bhutan 2006-2015 is the first edition of data being published by the Election Commission of Bhutan (ECB). The book provides comprehensive statistical information of all elections that the Election Commission has conducted since its establishment in 2006 to 2015 including the First and Second Parliamentary Elections in 2008 and 2013, Thromde Elections in 2011, three phases of Local Government Elections in 2012 and series of Re-Elections and Bye-Elections for both Parliamentary and Local Government. This publication will enable readers to get reliable information related to voters, voter turnout, election officials, media coverage of elections and other relevant and available information related to elections in Bhutan. The data and information compiled in this book are based on the information collected from the polling stations, Dzongkhag Election Offices, and the ECB Head Office. The book is expected to be a source of information and serve as a data bank for any users wishing to carry out research and studies on matters related to elections in Bhutan. -

Economic and Finance Committee's Review Report on National Budget for Financial Year 2020-21 June 6, 2020
ECONOMIC AND FINANCE COMMITTEE’S REVIEW REPORT ON NATIONAL BUDGET FOR FINANCIAL YEAR 2020-21 JUNE 6, 2020 COMMITTEE MEMBERS: 1. Hon’ble Kinley Wangchuk, Athang Thedtsho Constituency, Chairperson 2. Hon’ble Ganesh Gimary, Phuntshopelri Constituency, Dy. Chairperson 3. Hon’ble Dorji Wangdi, Panbang Constituency 4. Hon’ble Jurme Wangchuk, Drujeygang Tseza Constituency 5. Hon’ble Garja Man Rai, Sergithang Tserang Toed Constituency 6. Hon’ble Kinga Penjor, Gangzur Minjey Constituency 7. Hon’ble Tek Bhadur Rai, Shompangkha Constituency 8. Hon’ble Bimal Thapa, Kilkhorthang Mendrelgang Constituency 9. Hon’ble Passang Dorji, Bartsham Shongphu Constituency 10. Hon’ble Rinzin Jamtsho, Kengkhar Weringla Constituency 11. Hon’ble Gyembo Tshering, Bardo Trong Constituency 12. Hon’ble Choki Gyeltshen, Membi Tsaenkhar Constituency 13. Hon’ble Dupthob, Bumdeling Jamkhar Constituency Economic and Finance Committee’s review report on National Budget for Financial Year 2020-21 Introduction At the feet of the Glorious Golden Throne, I, on behalf of the thirteen Hon’ble Members of the Economic and Finance Committee would like to sincerely thank the Hon’ble Speaker for bestowing me the opportunity to present the Budget Review Report. Before introducing the report, I would like to address the House on the global health crisis the world is facing, a crisis far graver than what we have seen. COVID-19 has impacted nearly every country in the world, however due to His Majesty’s farsighted leadership our nation is able to successfully prevent COVID-19 taking tolls on Bhutanese lives. During the national address on National Resilience Fund delivered on 10th April, 2020, His Majesty commanded that, “in times of normal conditions, while making national choices, we must carefully examine and weigh the difference between sufficiency and insufficiency, the important and the unimportant, benefits and costs by deliberating over long-term rather than short-term interests.