Italy Health System Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Central and Southern Italy Campania, Molise, Abruzzo, Marche, Umbria and Lazio Garigliano
EUROPEAN COMMISSION DIRECTORATE-GENERAL FOR ENERGY DIRECTORATE D - Nuclear Safety and Fuel Cycle Radiation Protection Main Conclusions of the Commission’s Article 35 verification NATIONAL MONITORING NETWORK FOR ENVIRONMENTAL RADIOACTIVITY Central and Southern Italy Campania, Molise, Abruzzo, Marche, Umbria and Lazio DISCHARGE AND ENVIRONMENTAL MONITORING Garigliano NPP Date: 12 to 17 September 2011 Verification team: Mr C. Gitzinger (team leader) Mr E. Henrich Mr. E. Hrnecek Mr. A. Ryan Reference: IT-11/06 INTRODUCTION Article 35 of the Euratom Treaty requires that each Member State shall establish facilities necessary to carry out continuous monitoring of the levels of radioactivity in air, water and soil and to ensure compliance with the basic safety standards (1). Article 35 also gives the European Commission (EC) the right of access to such facilities in order that it may verify their operation and efficiency. For the EC, the Directorate-General for Energy (DG ENER) and in particular its Radiation Protection Unit (at the time of the visit ENER.D.4, now ENER.D.3) is responsible for undertaking these verifications. The main purpose of verifications performed under Article 35 of the Euratom Treaty is to provide an independent assessment of the adequacy of monitoring facilities for: - Liquid and airborne discharges of radioactivity into the environment by a site (and control thereof). - Levels of environmental radioactivity at the site perimeter and in the marine, terrestrial and aquatic environment around the site, for all relevant pathways. - Levels of environmental radioactivity on the territory of the Member State. Taking into account previous bilateral protocols, a Commission Communication has been published in the Official Journal on 4 July 2006 with a view to define some practical arrangements for the conduct of Article 35 verification visits in Member States. -

Wines by the Glass
WINES BY THE GLASS ROSÉ Macari Vineyards Estate Mattituck 2016 North Fork, NY 11/36 CHAMPAGNE & SPARKLING Segura Viudas Blanco Cava Brut NV Catalunya, SP 10 Btl 187ml Segura Viudas Rose Cava Brut NV Catalunya, SP 10 Btl 187ml Caviro Romio Prosecco NV Veneto, IT 10/36 I Borboni Asprinio Brut NV Campania, IT 49 Btl Ferrari Brut NV Trentino, IT 49 Ferrari Giulio Ferrari Brut Riserva del Fondatore 2002 Trentino, IT 270 Btl Champagne Philippe Gonet Brut Signature Blanc de Blancs NV Champagne, FR 40 Btl 375ml Champagne Fleury Brut Blancs de Noir Rose NV Biodynamic Champagne, FR 45 Btl 375ml La Caudrina Moscato d’Asti Piedmont, IT 10/34 500ml FROM THE TAP $9 per Glass Trebbiano/Poderi dal Nespoli/Sustainably Farmed 2016 Emilia-Romagna, IT Pinot Grigio/Venegazzu Montelvini Veneto, IT Chardonnay/Millbrook Estate/Sustainably Farmed 2014 Hudson River Valley, NY Barbera d’Alba/Cascina Pace/Sustainably Farmed 2015 Piedmont, IT Sangiovese/Poderi Dal Nespoli, Sangiovese Rubicone 2015 Emilia-Romagna, IT Merlot-Cabernet Sauvignon/Venegazzu Montelvini Veneto, IT WHITES BY THE GLASS/BOTTLE Cantina Cembra Sauvignon Blanc 2016 Trentino, IT 10/36 Figini Gavi di Gavi Cortese 2016 Piedmont, IT 12/40 Albino Armani “io” Pinot Grigio 2016 Trentino, IT 10/34 Paco y Lola Albarino 2013 Rias Baixas, SP 14/49 Suhru Riesling (Dry) 2016 Long Island, NY 11/39 Tenuta dell’ Ugolino Le Piaole “Castelli di Jesi” Verdicchio 2016 Marche, IT 10/38 Tenute Iuzzolini Ciro Bianco 2014 Calabria, IT 10/34 Marabino “Muscatedda” Moscato di Noto (Dry) 2014 Certified Organic Sicily, IT -

Response of the LAZIO-Sirad Detector to Low Energy Electrons
29th International Cosmic Ray Conference Pune (2005) 2, 449-452 Response of the LAZIO-SiRad detector to low energy electrons R. Bencardinoa, F. Altamuraa, V. Bidolia, L. Bongiornoa, M. Casolinoa, M.P. De Pascalea, M. Riccic, P. Picozzaa, D. Aisab, A. Alvinob, S. Ascanib, P. Azzarellob, R. Battistonb, S. Bizzagliab, M. Bizzarrib, S. Blaskob, L. Di Massob, G. Chioccib, D. Cossonb, G. Espositob, S. Lucidib, A. Papib, V. Postolacheb, S. Rossib, G. Scolierib, M. Ionicab, A. Franceschic, S. Dell'Agnelloc, C. Falconed, S. Tassad, A.Kalmikove, A.V.Popove, A. Abramove, M.C. Korotkove, A.M. Galpere, A. Ivanovae, L. Contif, V. Sgrignaf, C. Stagnif, A. Buzzif, D. Zilpimianig, A. Pontettih and L. Valentinih (a) Physics Department of "Tor Vergata University" and Roma II Section of INFN, Via della Ricerca Scientifica 1, 00133 Roma, Italy (b) Physics Department and INFN Section of Perugia, Via Pascoli, 06100 Perugia, Italy (c) INFN, Laboratori Nazionali di Frascati, Via E. Fermi 40, 00044 Frascati, Italy (d) Nergal S.r.l. Via Baldanzellu 8, 00155 Roma, Italy (e) Moscow Engineering and Physics Institute, Kashirskoe Shosse 31, RU-115409 Moscow, Russia (f) Physics Department of "Roma III University" Via della vasca navale 84, 00146 Roma, Italy (g) Institute of geophysics, Georgian Academy of Science (GAS) and National Space agency of Tbilisi, republic of Georgia (h) Ferrari BSN, Località Miole 100, 67063 Oricola (AQ), Italy Presenter: R. Bencardino ([email protected]), ita-bencardino-R-abs1-sh36-poster LAZIO-SiRad, the Low Altitude Zone Ionization Observatory experiment, launched on February 28th 2005, started its operations on board the International Space Station in April 2005. -

Migrant Health in Italy: a Better Health Status Difficult to Maintain—Country
Campostrini et al. Population Health Metrics (2019) 17:14 https://doi.org/10.1186/s12963-019-0194-8 RESEARCH Open Access Migrant health in Italy: a better health status difficult to maintain—country of origin and assimilation effects studied from the Italian risk factor surveillance data Stefano Campostrini1* , Giuliano Carrozzi2, Santino Severoni3, Maria Masocco4, Stefania Salmaso4, WHO Migration Health Programme, Office of the Regional Director, WHO Regional Office for Europe and the PASSI National Coordinating group Abstract Background: Many studies on migrant health have focused on aspects of morbidity and mortality, but very few approach the relevant issues of migrants’ health considering behavioral risk factors. Previous studies have often been limited methodologically because of sample size or lack of information on migrant country of origin. Information about risk factors is fundamental to direct any intervention, particularly with regard to non- communicable diseases that are leading causes of death and disease. Thus, the main focus of our analysis is the influence of country of origin and the assimilation process. Method: Utilizing a surveillance system that has been collecting over 30,000 interviews a year in Italy since 2008, we have studied migrants’ attitudes and behaviors by country of origin and by length of stay. Given 6 years of observation, we have obtained and analyzed 228,201 interviews of which over 9000 were migrants. Results: While migrants overall present similar conditions to native-born Italians, major differences appear when country of origin or length of stay is considered. Subgroups of migrants present substantially different behaviors, some much better than native-born Italians, some worse. -

25Th INTERNATIONAL FEDERATION of HOSPITAL ENGINEERING CONGRESS
25th INTERNATIONAL FEDERATION OF HOSPITAL ENGINEERING CONGRESS IFHE MAY 27-31 2018 RIETI INVITATION Bologna June 10 2018 Dear International Federation of Hospital Engineering, The SIAIS (Italian Society for Architecture and Engineer for Healthcare) would be honoured to host in 2018, the IFHE 25th Congress, in Italy . The SIAIS believes that the opportunity to have in Italy the 25th edition of the IFHE Congress should not be missed for the following reasons: first of all, Italy is absent from the international scene for a long time, second is that the recurrence of twenty-five years cannot fail to see Italy, which in 1970 hosted the 1st IFHE Congress, as the organizer of this important moment in science. The proposed conference location is Rieti the centre of Italy. The proposed dates in 2018, are : from Sunday, May 27 to Thursday, May 31. The official languages of the congress will be English and Italian, therefore simultaneous translation from Italian to English and vice versa will be guaranteed. Should a large group of delegates of a particular language be present it will be possible to arrange a specific simultaneous translation. May is a very pleasant month in Rieti with nice weather, still long sunny days and warm temperatures. Rieti is an Italian town of 47 927 inhabitants of Latium, capital of the Province of Rieti. Traditionally considered to be the geographical center of Italy, and this referred to as "Umbilicus Italiae", is situated in a fertile plain down the slopes of Mount Terminillo, on the banks of the river Velino. Founded at the beginning of the Iron Age, became the most important city of the Sabine people. -
Health Care Systems in the Eu a Comparative Study
EUROPEAN PARLIAMENT DIRECTORATE GENERAL FOR RESEARCH WORKING PAPER HEALTH CARE SYSTEMS IN THE EU A COMPARATIVE STUDY Public Health and Consumer Protection Series SACO 101 EN This publication is available in the following languages: EN (original) DE FR The opinions expressed in this document are the sole responsibility of the author and do not necessarily represent the official position of the European Parliament. Reproduction and translation for non-commercial purposes are authorized, provided the source is acknowledged and the publisher is given prior notice and sent a copy. Publisher: EUROPEAN PARLIAMENT L-2929 LUXEMBOURG Author: Dr.med. Elke Jakubowski, MSc. HPPF, Advisor in Public Health Policy Department of Epidemiology and Social Medicine, Medical School Hannover Co-author: Dr.med. Reinhard Busse, M.P.H., Department of Epidemiology and Social Medicine, Medical School Hannover Editor: Graham R. Chambers BA Directorate-General for Research Division for Policies on Social Affairs, Women, Health and Culture Tel.: (00 352) 4300-23957 Fax: (00 352) 4300-27720 e-mail: [email protected] WITH SPECIAL GRATITUDE TO: James Kahan, Panos Kanavos, Julio Bastida-Lopez, Elias Mossialos, Miriam Wiley, Franco Sassi, Tore Schersten, Juha Teperi for their helpful comments and reviews of earlier drafts of the country chapters, and Manfred Huber for additional explanatory remarks on OECD Health Data. The manuscript was completed in May 1998. EUROPEAN PARLIAMENT DIRECTORATE GENERAL FOR RESEARCH WORKING PAPER HEALTH CARE SYSTEMS IN THE EU A COMPARATIVE STUDY Public Health and Consumer Protection Series SACO 101 EN 11-1998 Health Care Systems CONTENTS INTRODUCTION ........................................................... 5 PART ONE: A Comparative Outline of the Health Care Systems of the EU Member States ........................................ -

Health in Italy in the 21St Century
FOREWORD Rosy Bindi Minister of Health of Italy Roma, September 1999 This report provides the international community with an overall assessment of the state of health in Italy, as well as with the main developments of the Italian public health policy expected in the near future. It is intended as an important contribution towards the activities which, beginning with the 49th WHO Regional Committee in Florence, will be carried out in Europe with a view to defining health policies and strategies for the new century. This publication, which consists of two sections, illustrates the remarkable health achievements of Italy as regards both the control of diseases and their determinants, and the health care services. Overall, a clearly positive picture emerges, which is due not only to the environmental and cultural characteristics of Italy, but also to its health protection and care system which Italy intends to keep and indeed to improve in the interest of its citizens. The recent decisions taken in the framework of the reform of the National Health System in Italy intend to improve and strengthen the model of a universal health system based on equity and solidarity, which considers health as a fundamental human right irrespective of the economic, social and cultural conditions of each citizen. The new national health service guarantees, through its public resources, equal opportunities for accessing health services as well as homogenous and essential levels of health care throughout the country. Such a reorganization of the system has become necessary in order to meet new and growing demands for health within the framework of limited resources and with the understanding that equity in health is not only an ethical requirement, but also a rational and efficient way for allocating resources. -

Sea-Level Rise in Venice
https://doi.org/10.5194/nhess-2020-351 Preprint. Discussion started: 12 November 2020 c Author(s) 2020. CC BY 4.0 License. Review article: Sea-level rise in Venice: historic and future trends Davide Zanchettin1, Sara Bruni2*, Fabio Raicich3, Piero Lionello4, Fanny Adloff5, Alexey Androsov6,7, Fabrizio Antonioli8, Vincenzo Artale9, Eugenio Carminati10, Christian Ferrarin11, Vera Fofonova6, Robert J. Nicholls12, Sara Rubinetti1, Angelo Rubino1, Gianmaria Sannino8, Giorgio Spada2,Rémi Thiéblemont13, 5 Michael Tsimplis14, Georg Umgiesser11, Stefano Vignudelli15, Guy Wöppelmann16, Susanna Zerbini2 1University Ca’ Foscari of Venice, Dept. of Environmental Sciences, Informatics and Statistics, Via Torino 155, 30172 Mestre, Italy 2University of Bologna, Department of Physics and Astronomy, Viale Berti Pichat 8, 40127, Bologna, Italy 10 3CNR, Institute of Marine Sciences, AREA Science Park Q2 bldg., SS14 km 163.5, Basovizza, 34149 Trieste, Italy 4Unversità del Salento, Dept. of Biological and Environmental Sciences and Technologies, Centro Ecotekne Pal. M - S.P. 6, Lecce Monteroni, Italy 5National Centre for Atmospheric Science, University of Reading, Reading, UK 6Alfred Wegener Institute Helmholtz Centre for Polar and Marine Research, Postfach 12-01-61, 27515, Bremerhaven, 15 Germany 7Shirshov Institute of Oceanology, Moscow, 117997, Russia 8ENEA Casaccia, Climate and Impact Modeling Lab, SSPT-MET-CLIM, Via Anguillarese 301, 00123 Roma, Italy 9ENEA C.R. Frascati, SSPT-MET, Via Enrico Fermi 45, 00044 Frascati, Italy 10University of Rome La Sapienza, Dept. of Earth Sciences, Piazzale Aldo Moro 5, 00185 Roma, Italy 20 11CNR - National Research Council of Italy, ISMAR - Marine Sciences Institute, Castello 2737/F, 30122 Venezia, Italy 12 Tyndall Centre for Climate Change Research, University of East Anglia. -

The North-South Divide in Italy: Reality Or Perception?
CORE Metadata, citation and similar papers at core.ac.uk EUROPEAN SPATIAL RESEARCH AND POLICY Volume 25 2018 Number 1 http://dx.doi.org/10.18778/1231-1952.25.1.03 Dario MUSOLINO∗ THE NORTH-SOUTH DIVIDE IN ITALY: REALITY OR PERCEPTION? Abstract. Although the literature about the objective socio-economic characteristics of the Italian North- South divide is wide and exhaustive, the question of how it is perceived is much less investigated and studied. Moreover, the consistency between the reality and the perception of the North-South divide is completely unexplored. The paper presents and discusses some relevant analyses on this issue, using the findings of a research study on the stated locational preferences of entrepreneurs in Italy. Its ultimate aim, therefore, is to suggest a new approach to the analysis of the macro-regional development gaps. What emerges from these analyses is that the perception of the North-South divide is not consistent with its objective economic characteristics. One of these inconsistencies concerns the width of the ‘per- ception gap’, which is bigger than the ‘reality gap’. Another inconsistency concerns how entrepreneurs perceive in their mental maps regions and provinces in Northern and Southern Italy. The impression is that Italian entrepreneurs have a stereotyped, much too negative, image of Southern Italy, almost a ‘wall in the head’, as also can be observed in the German case (with respect to the East-West divide). Keywords: North-South divide, stated locational preferences, perception, image. 1. INTRODUCTION The North-South divide1 is probably the most known and most persistent charac- teristic of the Italian economic geography. -

Map 44 Latium-Campania Compiled by N
Map 44 Latium-Campania Compiled by N. Purcell, 1997 Introduction The landscape of central Italy has not been intrinsically stable. The steep slopes of the mountains have been deforested–several times in many cases–with consequent erosion; frane or avalanches remove large tracts of regolith, and doubly obliterate the archaeological record. In the valley-bottoms active streams have deposited and eroded successive layers of fill, sealing and destroying the evidence of settlement in many relatively favored niches. The more extensive lowlands have also seen substantial depositions of alluvial and colluvial material; the coasts have been exposed to erosion, aggradation and occasional tectonic deformation, or–spectacularly in the Bay of Naples– alternating collapse and re-elevation (“bradyseism”) at a staggeringly rapid pace. Earthquakes everywhere have accelerated the rate of change; vulcanicity in Campania has several times transformed substantial tracts of landscape beyond recognition–and reconstruction (thus no attempt is made here to re-create the contours of any of the sometimes very different forerunners of today’s Mt. Vesuvius). To this instability must be added the effect of intensive and continuous intervention by humanity. Episodes of depopulation in the Italian peninsula have arguably been neither prolonged nor pronounced within the timespan of the map and beyond. Even so, over the centuries the settlement pattern has been more than usually mutable, which has tended to obscure or damage the archaeological record. More archaeological evidence has emerged as modern urbanization spreads; but even more has been destroyed. What is available to the historical cartographer varies in quality from area to area in surprising ways. -

How to Cite Complete Issue More Information About This Article
Civitas - Revista de Ciências Sociais ISSN: 1519-6089 ISSN: 1984-7289 Pontifícia Universidade Católica do Rio Grande do Sul Vannucci, Alberto Systemic corruption and disorganized anticorruption in Italy: governance, politicization, and electoral accountability Civitas - Revista de Ciências Sociais, vol. 20, no. 3, 2020, September-December, pp. 408-424 Pontifícia Universidade Católica do Rio Grande do Sul DOI: https://doi.org/10.15448/1984-7289.2020.3.37877 Available in: https://www.redalyc.org/articulo.oa?id=74266204008 How to cite Complete issue Scientific Information System Redalyc More information about this article Network of Scientific Journals from Latin America and the Caribbean, Spain and Journal's webpage in redalyc.org Portugal Project academic non-profit, developed under the open access initiative OPEN ACCESS CIVITAS Revista de Ciências Sociais Programa de Pós-Graduação em Ciências Sociais Civitas 20 (3): 408-424, set.-dez. 2020 e-ISSN: 1984-7289 ISSN-L: 1519-6089 http://dx.doi.org/10.15448/1984-7289.2020.3.37877 DOSSIER: FIGHT AGAINST CORRUPTION: STATE OF THE ART AND ANALYSIS PERSPECTIVES Systemic corruption and disorganized anticorruption in Italy: governance, politicization, and electoral accountability Corrupção sistêmica e anticorrupção desorganizada na Itália: governança, politização e accountability eleitoral Corrupción sistémica y anticorrupción desorganizada en Italia: gobernanza, politización y accountability electoral Alberto Vannucci1 Abstract: This paper provides, trough different indicators, empirical evidence on the orcid.org/0000-0003-0434-1323 presumably high relevance of corruption in Italian politics and administration, providing [email protected] an explanation of how this “obscure” side of Italian politics – a pervasive market for corrupt exchanges – has found its way to regulate its hidden activities within an informal institutional framework, i.e. -
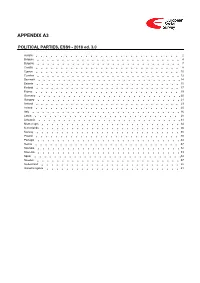
ESS9 Appendix A3 Political Parties Ed
APPENDIX A3 POLITICAL PARTIES, ESS9 - 2018 ed. 3.0 Austria 2 Belgium 4 Bulgaria 7 Croatia 8 Cyprus 10 Czechia 12 Denmark 14 Estonia 15 Finland 17 France 19 Germany 20 Hungary 21 Iceland 23 Ireland 25 Italy 26 Latvia 28 Lithuania 31 Montenegro 34 Netherlands 36 Norway 38 Poland 40 Portugal 44 Serbia 47 Slovakia 52 Slovenia 53 Spain 54 Sweden 57 Switzerland 58 United Kingdom 61 Version Notes, ESS9 Appendix A3 POLITICAL PARTIES ESS9 edition 3.0 (published 10.12.20): Changes from previous edition: Additional countries: Denmark, Iceland. ESS9 edition 2.0 (published 15.06.20): Changes from previous edition: Additional countries: Croatia, Latvia, Lithuania, Montenegro, Portugal, Slovakia, Spain, Sweden. Austria 1. Political parties Language used in data file: German Year of last election: 2017 Official party names, English 1. Sozialdemokratische Partei Österreichs (SPÖ) - Social Democratic Party of Austria - 26.9 % names/translation, and size in last 2. Österreichische Volkspartei (ÖVP) - Austrian People's Party - 31.5 % election: 3. Freiheitliche Partei Österreichs (FPÖ) - Freedom Party of Austria - 26.0 % 4. Liste Peter Pilz (PILZ) - PILZ - 4.4 % 5. Die Grünen – Die Grüne Alternative (Grüne) - The Greens – The Green Alternative - 3.8 % 6. Kommunistische Partei Österreichs (KPÖ) - Communist Party of Austria - 0.8 % 7. NEOS – Das Neue Österreich und Liberales Forum (NEOS) - NEOS – The New Austria and Liberal Forum - 5.3 % 8. G!LT - Verein zur Förderung der Offenen Demokratie (GILT) - My Vote Counts! - 1.0 % Description of political parties listed 1. The Social Democratic Party (Sozialdemokratische Partei Österreichs, or SPÖ) is a social above democratic/center-left political party that was founded in 1888 as the Social Democratic Worker's Party (Sozialdemokratische Arbeiterpartei, or SDAP), when Victor Adler managed to unite the various opposing factions.