Kemi-Riskline
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

5. POTENTIAL for HUMAN EXPOSURE 5.1 OVERVIEW White
WHITE PHOSPHORUS 157 5. POTENTIAL FOR HUMAN EXPOSURE 5.1 OVERVIEW White phosphorus can enter the environment from its production, use, accidental spills during loading and unloading for shipment, and accidental spills during transport. Hazardous wastes sites containing white phosphorus can also be a source of phosphorus in the environment. White phosphorus has been found in at least 77 of the 1,430 current or former EPA National Priorities List (NPL) hazardous waste sites (HazDat 1996). However, the number of sites evaluated for white phosphorus is not known. The frequency of these sites within the United States can be seen in Figure 5-l. The persistence of elemental phosphorus in the air is very short due to oxidation to phosphorus oxides and ultimately to phosphorus acids. However, the particulate phosphorus aerosol may be coated with a protective oxide layer that may prevent further oxidation and extend the lifetime of particulate phosphorus in air. Both wet and dry deposition remove unreacted elemental phosphorus and the degradation products from the air. Similarly, elemental phosphorus oxidizes and hydrolyzes in water and in soil. A small amount of elemental phosphorus is lost from soil and water by volatilization. Phosphorus is used as a fumigant in the storage of grain. Because of ease of application, pellets of aluminum or magnesium phosphide are commonly used (Garry et al. 1993). Phosphine, a highly toxic gas, is generated from phosphide. The rate of formation of phosphine (permissible exposure limit [PEL], 0.4 mg/m3) is dependent on the ambient temperature and humidity. Its release is rapid, and it is extremely fatal to the unprotected person (Garry et al. -
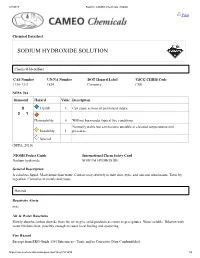
Sodium Hydroxide, Solution (Material Safety Data Sheet)
3/7/2018 Report | CAMEO Chemicals | NOAA Print Chemical Datasheet SODIUM HYDROXIDE SOLUTION Chemical Identifiers CAS Number UN/NA Number DOT Hazard Label USCG CHRIS Code 1310-73-2 1824 Corrosive CSS NFPA 704 Diamond Hazard Value Description 0 Health 3 Can cause serious or permanent injury. 3 1 Flammability 0 Will not burn under typical fire conditions. Normally stable but can become unstable at elevated temperatures and Instability 1 pressures. Special (NFPA, 2010) NIOSH Pocket Guide International Chem Safety Card Sodium hydroxide SODIUM HYDROXIDE General Description A colorless liquid. More dense than water. Contact may severely irritate skin, eyes, and mucous membranes. Toxic by ingestion. Corrosive to metals and tissue. Hazards Reactivity Alerts none Air & Water Reactions Slowly absorbs carbon dioxide from the air to give solid products as crusts or precipitates. Water soluble. Dilution with water liberates heat, possibly enough to cause local boiling and spattering. Fire Hazard Excerpt from ERG Guide 154 [Substances - Toxic and/or Corrosive (Non-Combustible)]: https://cameochemicals.noaa.gov/report?key=CH1499 1/5 3/7/2018 Report | CAMEO Chemicals | NOAA Non-combustible, substance itself does not burn but may decompose upon heating to produce corrosive and/or toxic fumes. Some are oxidizers and may ignite combustibles (wood, paper, oil, clothing, etc.). Contact with metals may evolve flammable hydrogen gas. Containers may explode when heated. For electric vehicles or equipment, ERG Guide 147 (lithium ion batteries) or ERG Guide 138 (sodium batteries) should also be consulted. (ERG, 2016) Health Hazard Causes severe burns of eyes, skin, and mucous membranes. (USCG, 1999) Reactivity Profile SODIUM HYDROXIDE SOLUTION refers to an aqueous solution of sodium hydroxide. -
Alphabetical Index of Substances and Articles
ALPHABETICAL INDEX OF SUBSTANCES AND ARTICLES - 355 - NOTES TO THE INDEX 1. This index is an alphabetical list of the substances and articles which are listed in numerical order in the Dangerous Goods List in Chapter 3.2. 2. For the purpose of determining the alphabetical order the following information has been ignored even when it forms part of the proper shipping name: numbers; Greek letters; the abbreviations “sec” and “tert”; and the letters “N” (nitrogen), “n” (normal), “o” (ortho) “m” (meta), “p” (para) and “N.O.S.” (not otherwise specified). 3. The name of a substance or article in block capital letters indicates a proper shipping name. 4. The name of a substance or article in block capital letters followed by the word “see” indicates an alternative proper shipping name or part of a proper shipping name (except for PCBs). 5. An entry in lower case letters followed by the word “see” indicates that the entry is not a proper shipping name; it is a synonym. 6. Where an entry is partly in block capital letters and partly in lower case letters, the latter part is considered not to be part of the proper shipping name. 7. A proper shipping name may be used in the singular or plural, as appropriate, for the purposes of documentation and package marking. - 356 - INDEX Name and description Class UN No. Name and description Class UN No. Accumulators, electric, see 4.3 3292 Acid mixture, nitrating acid, see 8 1796 8 2794 8 2795 Acid mixture, spent, nitrating acid, see 8 1826 8 2800 8 3028 Acraldehyde, inhibited, see 6.1 1092 ACETAL 3 1088 -

Chemical Chemical Hazard and Compatibility Information
Chemical Chemical Hazard and Compatibility Information Acetic Acid HAZARDS & STORAGE: Corrosive and combustible liquid. Serious health hazard. Reacts with oxidizing and alkali materials. Keep above freezing point (62 degrees F) to avoid rupture of carboys and glass containers.. INCOMPATIBILITIES: 2-amino-ethanol, Acetaldehyde, Acetic anhydride, Acids, Alcohol, Amines, 2-Amino-ethanol, Ammonia, Ammonium nitrate, 5-Azidotetrazole, Bases, Bromine pentafluoride, Caustics (strong), Chlorosulfonic acid, Chromic Acid, Chromium trioxide, Chlorine trifluoride, Ethylene imine, Ethylene glycol, Ethylene diamine, Hydrogen cyanide, Hydrogen peroxide, Hydrogen sulfide, Hydroxyl compounds, Ketones, Nitric Acid, Oleum, Oxidizers (strong), P(OCN)3, Perchloric acid, Permanganates, Peroxides, Phenols, Phosphorus isocyanate, Phosphorus trichloride, Potassium hydroxide, Potassium permanganate, Potassium-tert-butoxide, Sodium hydroxide, Sodium peroxide, Sulfuric acid, n-Xylene. Acetone HAZARDS & STORAGE: Store in a cool, dry, well ventilated place. INCOMPATIBILITIES: Acids, Bromine trifluoride, Bromine, Bromoform, Carbon, Chloroform, Chromium oxide, Chromium trioxide, Chromyl chloride, Dioxygen difluoride, Fluorine oxide, Hydrogen peroxide, 2-Methyl-1,2-butadiene, NaOBr, Nitric acid, Nitrosyl chloride, Nitrosyl perchlorate, Nitryl perchlorate, NOCl, Oxidizing materials, Permonosulfuric acid, Peroxomonosulfuric acid, Potassium-tert-butoxide, Sulfur dichloride, Sulfuric acid, thio-Diglycol, Thiotrithiazyl perchlorate, Trichloromelamine, 2,4,6-Trichloro-1,3,5-triazine -

United States Paterrtg?Iee Patented V.Decp 28, ,1954
2,698,267 United States PaterrtG?iee Patented v.Decp 28, ,1954 serve as a‘ ?uxing agent toconvert ,theloxide land‘z-nitride, or: any~of the other impurities awhichmay;be;»present,t to a liquid slag which can be squeezed or workedaout of'sthe 2,698,267 , metal readily. No entirelyusatisfactory ?uxingfagent-Pfor WORKING 0F TITANIUM'" the working of titanium .has heretofore'been ‘developed. It is apparent that any procedure which-canbe-employed -\\___ Roy - A. Halversen, Deal-born,“ Mich» in the working of titanium-‘to give products superior-to No Drawing. Appli‘chtion'June'ZS, 1953, those now possible to obtain would be of~extremewalue It has now been found’that most of‘the' dit?culties Serial No.'364,209 encountered in the working of-ytitanium due to there 6 Claims. ' (Cl; 1484-115) A tention of non-metallic substances-and of-highlyreac-tive metals in the worked metal, and to the conversionrof metal . to oxide or nitride, can beeovercome almost entirely-by hot-working the metal while keepingpitsv surface blanketed This invention :relatesv to the .working. of. titanium, ‘ with an atmosphere comprising aphosphorus toxidepsuch particularly to a method for. working titanium'toobtain as phosphorus trioxide or phosphorus pentoxidew vWhen articles of improved properties. the working is carried out in this manner, substantially The increasing technological importance of titanium all of the titanium oxide and nitride, most of the-silica, metal is well known. Because of its light weight, high the reactive metals and their oxides and-manypther im strength, maintenancev of its strength at high \tempera- .. purities often associated with the metal in small propor tures and- other advantageousproperties, titanium has tions, are converted smoothly and rapidly to phosphorus shown itself to be unique among the metals for-{many containing slags which are liquid over substantially; the purposes. -

The Combustion of Phosphorus
Scholars' Mine Professional Degree Theses Student Theses and Dissertations 1944 The combustion of phosphorus Erwin Charles Hoeman Follow this and additional works at: https://scholarsmine.mst.edu/professional_theses Part of the Chemical Engineering Commons Department: Recommended Citation Hoeman, Erwin Charles, "The combustion of phosphorus" (1944). Professional Degree Theses. 284. https://scholarsmine.mst.edu/professional_theses/284 This Thesis - Open Access is brought to you for free and open access by Scholars' Mine. It has been accepted for inclusion in Professional Degree Theses by an authorized administrator of Scholars' Mine. This work is protected by U. S. Copyright Law. Unauthorized use including reproduction for redistribution requires the permission of the copyright holder. For more information, please contact [email protected]. THE COMBUSTION OF PHOSPHORUS BY ERWIN CHA.RLES HODWt A 'l'HESIS subnitted to the faculty of the SCHOOL OF MINES AND METALLURGY OF THE UNIVERSITY OF MISSOURI 1D partial. fulfillment of the work required tor the Degre. of CBDlICAL gGIIllma Rolla~ II1s80url 1944 Approved by: It;-\/ '~I Cha1rmaD,De.partmant of. Chaistry ind Chea1cal IDg1Deer1ng. i ACKNOWLEDGMJ!JiT The author gratefu1lr acknowledges the experience gained in the production and utilization of phosphorus, through his employ ment in the Department of Chemical Engineering of the United States Tennessee Valley Authority. 'SpecificallY', he acknowledges the supervision of work and inspiration gained through his association with Dr. RaY'Dlond L. Copson, Chief of the Research and ,Development Division; Dr. GradY' Tarbutton, Assistant to the Chief; and Mr. John H. Walthall,. Head of the Developllellt Section. Particular thanks for guidanoe in the selection of the general plaD for this paper are due to Mr. -

E:\KM2 2020\KM 2 2020\01 Obalka Predna
KRÍZOVÝ MANAŽMENT DOI 10.26552/krm.C.2020.2.5-13 ISSN – 1336 - 0019 TOXICITY OF PLASTICS IN A FIRE AND ITS DANGEROUS PROPERTIES TOXICITA PLASTOV V POŽIARI A ICH NEBEZPEČNÉ VLASTNOSTI MARTIN HRINKO ABSTRACT: The article describes and analyses toxic substances produced during the combustion of plastics which affect human health. Accidents and emergencies resulting from the combustion of plastic materials frequently occur in industrial production and technological processes. The authors illustrate this fact using the most recent example - the fire in the manufacturing and logistics premises in Chropyně, the Czech Republic, with an intervention of professional, as well as volunteer firefighters and specialized fire and rescue units. KEYWORDS: Toxicity. Fire. Safety. Fire Protection. INTRODUCTION In the industrial environment, e.g. in motoring, aviation and many other key industries, a wide range of substances with various chemical properties is used. These, as a result of a chemical reaction caused by the fire, are transformed into tens or hundreds of different chemical substances with new and, in most cases, even more dangerous chemical properties. It is to be noted that the toxic properties of the newly produced substances also depend on the type of extinguishing agent used. Saving human lives (including the ones of the firefighters and other personnel) is the main goal during firefighting. The dangerous factors during firefighting are: elevated ambient temperature, excessive formation of smoke, a decrease in oxygen content in the air and toxic products of fire. Elevated ambient temperature makes the firefighters‘ work difficult, provokes defatigation and dehydration. Inhalation of hot products of combustion damages the airways, decreases blood pressure and may result in the failure of blood circulation, pulmonary edema or even in death. -
Hazardous Materials Descriptions and Codes
2012 Commodity Flow Survey Hazardous Materials Descriptions and Codes Hazardous Materials Descriptions and Proper Shipping Names UN or NA Code Accellerene, see p-Nitrosodimethylaniline Accumulators, electric, see Batteries, wet etc Accumulators, pressurized, pneumatic or hydraulic (containing non-flammable gas), see Articles pressurized, pneumatic or hydraulic (containing non-flammable gas) Acetal 1088 Acetaldehyde 1089 Acetaldehyde ammonia 1841 Acetaldehyde oxime 2332 Acetic acid, glacial or Acetic acid solution, with more than 80 percent acid, by mass 2789 Acetic acid solution, not less than 50 percent but not more than 80 percent acid, by 2790 mass Acetic acid solution, with more than 10 percent and less than 50 percent acid, by mass 2790 Acetic anhydride 1715 Acetone 1090 Acetone cyanohydrin, stabilized 1541 Acetone oils 1091 Acetonitrile 1648 Acetyl bromide 1716 Acetyl chloride 1717 Acetyl iodide 1898 Acetyl methyl carbinol 2621 Acetylene, dissolved 1001 Acetylene tetrabromide, see Tetrabromoethane Acid butyl phosphate, see Butyl acid phosphate Acid, sludge, see Sludge acid Acridine 2713 Acrolein dimer, stabilized 2607 Acrolein, stabilized 1092 Acrylamide, solid 2074 Acrylamide solution 3426 Acrylic acid, stabilized 2218 Acrylonitrile, stabilized 1093 Actuating cartridge, explosive, see Cartridges, power device Adhesives, containing a flammable liquid 1133 Adiponitrile 2205 Aerosols, poison, Packing Group III (each not exceeding 1 L capacity) 1950 Aerosols, flammable, (each not exceeding 1 L capacity) 1950 Source: Electronic Code of Federal Regulations http://ecfr.gpoaccess.gov/cgi/t/text/text- idx?c=ecfr&sid=dfec99df9f21ef29b59a8565433a56cd&rgn=div6&view=text&node=49:2.1.1.3.8.2&idno=49 1 Hazardous Materials Descriptions and Proper Shipping Names UN or NA Code Aerosols, flammable, n.o.s. -

Inorganic Nomenclature
6. INORGANIC NOMENCLATURE I 1. SPEAKING. Grammar – Time Clauses. Complete these sentences with your ideas. Then ask about them in pairs. Example: When I get home … I´m going to have a bath. Q: What are you going to do when you get home? a) When as I get home today ……………………………………. b) As soon as this lesson finishes …………………………………… c) After I finish my studies ……………………………………….. a) When I was a child ……………………………………………….. d) When I attended secondary school ………………………….. ……. e) …………………………………………………….. before I get too old. f) When I´m on holiday ………………………………………………… 2. Elements and compounds. Revision. Work in small groups. Try to answer these questions. a) What is the difference between an element (e.g. H) and a compound (e.g. H2SO4)? Try to write a definition of an element and a compound. b) What types and groups of elements do you know? c) Do you know any names of elements? What do you know about them? d) What is an ion? What types of ions do you know? What is their charge? e) What is an isotope? Give examples of isotopes. f) What is the difference between binary and ternary compounds? g) Give examples of some organic and inorganic compounds, acids and bases, salts, oxides, hydroxides. What do you know about them? What are their properties? What is their use? h) Explain these terms: chemical symbol, chemical formula, chemical equation. Give examples. 1 3. Listening. Listen to the Song of the elements by Tom Lehrer and fill in the gaps. 1 There’s antimony, arsenic, aluminum, selenium, There’s holmium and helium and hafnium and erbium, And hydrogen and and nitrogen and And and francium and fluorine rhenium. -

The Role of Oxygen and Water Abstract Black Phosphorus (BP)
Degradation of Black Phosphorus: The Role of Oxygen and Water Yuan Huang,1,2,3† Jingsi Qiao,4† Kai He,2 Stoyan Bliznakov,5 Eli Sutter,6 Xianjue Chen,1,3 Da Luo,1,3 Fanke Meng,5 Dong Su,2 Jeremy Decker,1 Wei Ji,4,* Rodney S. Ruoff,1, 3* and Peter Sutter7,* 1Center for Multidimensional Carbon Materials (CMCM), Institute for Basic Science (IBS), Ulsan 689- 798, Republic of Korea 2Center for Functional Nanomaterials, Brookhaven National Laboratory, Upton, NY 11973, USA 3Department of Chemistry and School of Materials Science and Engineering, Ulsan National Institute of Science and Technology, Ulsan 689-798, Republic of Korea 4Department of Physics and Beijing Key Laboratory of Optoelectronic Functional Materials & Micro- nano Devices, Renmin University of China, Beijing 100872, China 5Chemistry Department, Brookhaven National Laboratory, Upton, New York 11973, USA 6Department of Mechanical & Materials Engineering, University of Nebraska-Lincoln, Lincoln, NE 68588, USA 7Department of Electrical & Computer Engineering, University of Nebraska-Lincoln, Lincoln, NE 68588, USA Abstract Black phosphorus (BP) has attracted significant interest as a monolayer or few-layer material with extraordinary electrical and optoelectronic properties. However, degradation in air and other environments is an unresolved issue that may limit future applications. In particular the role of different ambient species has remained controversial. Here, we report systematic experiments combined with ab-initio calculations that address the effects of oxygen and water in the degradation of BP. Our results show that BP rapidly degrades whenever oxygen is present, but is unaffected by deaerated (i.e., O2 depleted) water. This behavior is rationalized by oxidation involving a facile dissociative chemisorption of O2, whereas H2O molecules are weakly physisorbed and do not dissociate on the BP surface. -

MLP-011005-09Lavapurplekt MSDS
LavaPurple Kit MSDS version 1.0 November 6, 2006 Material Safety Data Sheet Language: English ___________________________________________________________________ 1. Identification of the material and supplier Product Name: LavaPurple Total Protein Kit 5mL Catalogue number: LP-011005 Company Details Manufacturer gelcompany GmbH Paul-Ehrlich-Straße 17 D-72076 Tübingen Emergency telephone number : +49 (0)7071 257030 Area of Application: Industrial applications. Product Use: Analytical chemistry. Research use only. ___________________________________________________________________ 2. Hazard Identification Hazard Symbol(s): C R-35 F-Xn R11-20/21/22-36 Xi:R37/38-41 Risk Phrases: R35 - Causes severe burns R11-20/21/22-36 – Highly flammable. Harmful by inhalation, in contact with skin and if swallowed. R37/38-41 - Irritating to respiratory system and skin. Risk of serious damage to eyes. Safety Phrases: 16-37/39-45 - Keep away from sources of ignition – no smoking. Wear suitable protective clothing, gloves and eye/face protection. In case of contact with eyes, rinse immediately with plenty of water and seek medical advice. In case of accident or if you feel unwell, seek medical advice immediately (show the label where possible). Statement of hazardous/dangerous nature HAZARDOUS SUBSTANCE. NON-DANGEROUS GOODS. ___________________________________________________________________ www.gelcompany.com Page 1 / 8 DIN - MLP-011005-09 LavaPurple Kit MSDS version 1.0 November 6, 2006 3. Composition/information on ingredients Mixture: Yes. Kit consists of four components. A solution of epicocconone in dimethyl sulfoxide/acetonitrile, solid sodium hydroxide, solid boric acid and solid citric acid. Chemical name CAS no. % by Volume Epicocconone 371163-96-1 NA Dimethyl sulfoxide 67-68-5 67.5 Acetonitrile 75-05-08 32.2 Sodium hydroxide 1310-73-2 NA Boric Acid 10043-35-3 NA Citric Acid 5979-29-1 NA Additional Information: Not applicable Appearance: Purple Liquid. -

Material Safety Data Sheet
MATERIAL SAFETY DATA SHEET 1. PRODUCT AND COMPANY IDENTIFICATION Formulator: Gowan Company Emergency Phone: (928) 783-3803 P.O. Box 5569 For 24-Hour Emergency Yuma, Arizona 85366-5569 Assistance (Spill, Leak, Fire, or (928) 783-8844 Exposure), Call CHEMTREC®: Inside the U.S.: (800) 424-9300 Outside the U.S.: (703) 527-3887 For MEDICAL Emergency: (888) 478-0798 Product: Malathion 5 Dust EPA Signal Word: Caution EPA Registration No.: 10163-142 Active Ingredient: Malathion (5.0%) CAS No.: 121-75-5 Chemical Name: O, O-Dimethyl dithiophosphate of diethyl mercaptosuccinate Chemical Class Organophosphorous pesticide 2. HAZARDS IDENTIFICATION Physical Properties Appearance: Off-white powder Odor: Mild, sulfurous odor Symptoms of Overexposure May cause headaches, nausea, vomiting, cramps, weakness, blurred vision, pin-point pupils, tightness in chest, labored breathing, nervousness, sweating, watering of eyes, drooling or frothing of nose and mouth, and muscle spasms. Medical Conditions Likely to be Aggravated by Exposure Skin contact may aggravated preexisting skin conditions. Inhalation of mists may aggravate preexisting respiratory conditions. Primary Routes of Exposure Harmful if inhaled, ingested or skin contact occurs. Hazardous Decomposition Products Carbon monoxide, carbon dioxide, sulfur dioxide, phosphorus trioxide, methyl mercaptan, hydrogen sulfide, and dimethyl sulfide. Unusual Fire, Explosion, and Reactivity Hazards Product is slightly combustible. Product may support combustion at elevated temperatures. Malathion decomposes rapidly