Public Health Environment Bulletin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Greenhouse Gas Emissions Inventory for Kampala City and Metropolitan Region
Greenhouse Gas Emissions Inventory for Kampala City and Metropolitan Region Final Report Shuaib Lwasa Makerere University February 2013 1 Executive Summary This report presets a greenhouse gas emission inventory that was conducted as a baseline for Kampala city and 2012 as the base year. The inventory was conducted using the Global Protocol for Community-Scale Greenhouse Gas Emissions (GPC). The GPC builds on previous protocols that include the International Local Government GHG Emissions Analysis Protocol (ICLEI), Draft International Standard for Determining Greenhouse Gas Emissions for Cities (UNEP/UN-HABITAT/WB), GHG Protocol Standards (WRI/WBCSD), Baseline Emissions Inventory/Monitoring Emissions Inventory methodology (EC-CoM JRC), and Local Government Operations Protocol (ICLEI-USA). The baseline results are estimates of community-based emissions attributed to the 196 sq km of surface area of Kampala city and the city region that spans an area of 941.2 sq km. The population estimates of Kampala city at base year stand at 1.72 m and for the city-region 3.56 m adjusted from 2007 data. The total CO2e emissions stand at 313,320 tCO2e distributed as 53,178.5 tCO2e from stationary units, 26,407.3 tCO2e from mobile units, 203,771 tCO2e from wastes, 29,926.4 tCO2e from Industrial Processes and Product uses and 35.5 tCO2e from Agriculture, Forestry and Land Use. Using the adjusted population of the city, the percapita emission stands at 0.18216 tCO2e for in-boundary population and 0.08801 tCO2e for combined in-boundary and out-boundary population. Emissions are calculated based on activity data acquired from multiple sources and checked for minimization of overestimate and underestimate. -

Republic of Uganda
REPUBLIC OF UGANDA VALUE FOR MONEY AUDIT REPORT ON SOLID WASTE MANAGEMENT IN KAMPALA MARCH 2010 1 TABLE OF CONTENTS REPUBLIC OF UGANDA .......................................................................................................... 1 VALUE FOR MONEY AUDIT REPORT ..................................................................................... 1 ON SOLID WASTE MANAGEMENT IN KAMPALA .................................................................... 1 LIST OF ABBREVIATIONS ...................................................................................................... 4 EXECUTIVE SUMMARY ........................................................................................................... 5 CHAPTER 1 ......................................................................................................................... 10 INTRODUCTION ................................................................................................................ 10 1.0 BACKGROUND .............................................................................................10 1.1 MOTIVATION ...............................................................................................12 1.2 MANDATE ....................................................................................................13 1.3 VISION ........................................................................................................13 1.4 MISSION ................................................................................................................. -

Kampala Cholera Situation Report
Kampala Cholera Situation Report Date: Monday 4th February, 2019 1. Summary Statistics No Summary of cases Total Number Total Cholera suspects- Cummulative since start of 54 #1 outbreak on 2nd January 2019 1 New case(s) suspected 04 2 New cases(s) confirmed 54 Cummulative confirmed cases 22 New Deaths 01 #2 3 New deaths in Suspected 01 4 New deaths in Confirmed 00 5 Cumulative cases (Suspected & confirmed cases) 54 6 Cumulative deaths (Supected & confirmed cases) in Health Facilities 00 Community 03 7 Total number of cases on admission 00 8 Cummulative cases discharged 39 9 Cummulative Runaways from isolation (CTC) 07 #3 10 Number of contacts listed 93 11 Total contacts that completed 9 day follow-up 90 12 Contacts under follow-up 03 13 Total number of contacts followed up today 03 14 Current admissions of Health Care Workers 00 13 Cummulative cases of Health Care Workers 00 14 Cummulative deaths of Health Care Workers 00 15 Specimens collected and sent to CPHL today 04 16 Cumulative specimens collected 45 17 Cummulative cases with lab. confirmation (acute) 00 Cummulative cases with lab. confirmation (convalescent) 22 18 Date of admission of last confirmed case 01/02/2019 19 Date of discharge of last confirmed case 02/02/2019 20 Confirmed cases that have died 1 (Died from the community) #1 The identified areas are Kamwokya Central Division, Mutudwe Rubaga, Kitintale Zone 10 Nakawa, Naguru - Kasende Nakawa, Kasanga Makindye, Kalambi Bulaga Wakiso, Banda Zone B3, Luzira Kamwanyi, Ndeba-Kironde, Katagwe Kamila Subconty Luwero District, -

Approved Bodaboda Stages
Approved Bodaboda Stages SN Division Parish Stage ID X-Coordinate Y-Coordinate 1 CENTRAL DIVISION BUKESA 1001 32.563999 0.317146 2 CENTRAL DIVISION BUKESA 1002 32.564999 0.317240 3 CENTRAL DIVISION BUKESA 1003 32.566799 0.319574 4 CENTRAL DIVISION BUKESA 1004 32.563301 0.320431 5 CENTRAL DIVISION BUKESA 1005 32.562698 0.321824 6 CENTRAL DIVISION BUKESA 1006 32.561100 0.324322 7 CENTRAL DIVISION INDUSTRIAL AREA 1007 32.610802 0.312010 8 CENTRAL DIVISION INDUSTRIAL AREA 1008 32.599201 0.314553 9 CENTRAL DIVISION KAGUGUBE 1009 32.565701 0.325353 10 CENTRAL DIVISION KAGUGUBE 1010 32.569099 0.325794 11 CENTRAL DIVISION KAGUGUBE 1011 32.567001 0.327003 12 CENTRAL DIVISION KAGUGUBE 1012 32.571301 0.327249 13 CENTRAL DIVISION KAMWOKYA II 1013 32.583698 0.342530 14 CENTRAL DIVISION KOLOLO I 1014 32.605900 0.326255 15 CENTRAL DIVISION KOLOLO I 1015 32.605400 0.326868 16 CENTRAL DIVISION MENGO 1016 32.567101 0.305112 17 CENTRAL DIVISION MENGO 1017 32.563702 0.306650 18 CENTRAL DIVISION MENGO 1018 32.565899 0.307312 19 CENTRAL DIVISION MENGO 1019 32.567501 0.307867 20 CENTRAL DIVISION MENGO 1020 32.567600 0.307938 21 CENTRAL DIVISION MENGO 1021 32.569500 0.308241 22 CENTRAL DIVISION MENGO 1022 32.569199 0.309950 23 CENTRAL DIVISION MENGO 1023 32.564800 0.310082 24 CENTRAL DIVISION MENGO 1024 32.567600 0.311253 25 CENTRAL DIVISION MENGO 1025 32.566002 0.311941 26 CENTRAL DIVISION OLD KAMPALA 1026 32.567501 0.314132 27 CENTRAL DIVISION OLD KAMPALA 1027 32.565701 0.314559 28 CENTRAL DIVISION OLD KAMPALA 1028 32.566002 0.314855 29 CENTRAL DIVISION OLD -

Psychiatric Hospitals in Uganda
Psychiatric hospitals in Uganda A human rights investigation w www.mdac.org mentaldisabilityadvocacy @MDACintl Psychiatric hospitals in Uganda A human rights investigation 2014 December 2014 ISBN 978-615-80107-7-1 Copyright statement: Mental Disability Advocacy Center (MDAC) and Mental Health Uganda (MHU), 2014. All rights reserved. Contents Foreword ...................................................................................................................................................................................................... 4 Executive summary ......................................................................................................................................................................................................... 6 1. Introduction, torture standards and hospitals visited.............................................................................................................................. 9 1(A). The need for human rights monitoring........................................................................................................................................................... 9 1(B). Uganda country profile .................................................................................................................................................................................... 10 1(C). Mental health ................................................................................................................................................................................................... -

Vote:122 Kampala Capital City Authority V1: Vote Overview I
Kampala Capital City Authority Ministerial Policy Statement FY 2020/21 Vote:122 Kampala Capital City Authority V1: Vote Overview I. Vote Mission Statement To Deliver Quality Services to the City II. Strategic Objective 1. Improve Productivity of the city 2. Improve quality of social services 3. Enhance Attractiveness of the city 4. Enhance safety of communities 5. Improve Transport services 6. Improve Governance and Accountability 7. Optimize Resource Utilization 8. Increase Financial Resource Availability 9. Improve Communication 10. Promote Disaster Preparedness and Management 11. Improve Regulatory Framework 12. Improve Business Process Management 13. Improve Information Management 14. Increase KCCA Productivity 15. Enhance Human resource development 16. Enhance Strategic partnerships and collaboration 17. Improve Workplace Infrastructure Kampala Capital City Authority Ministerial Policy Statement FY 2020/21 Vote:122 Kampala Capital City Authority III. Major Achievements in 2019/20 SOLID WASTE MANAGEMENT -A total of 385 roads were cleaned across all divisions. Of these, 337 were swept daily whereas 48 roads periodically swept -A total of 112,801 tons of garbage was disposed of at the landfill from all the divisions by 189 (Max) collector trucks from a total of 21,858 trips of which 44% was delivered by KCCA while the rest (56%) was delivered by private companies -Fuelled and maintained 29 Garbage truck, made 5,683 trips to the Landfill at Kiteezi consuming a total of 119,623 litres of fuel. Community dialogue and sensitization -A total of 164 Community dialogues and sensitization meetings were conducted with 81 in Kawempe, 11 in Makindye, 26 in Central, 15 in Rubaga and 31 in Nakawa. -

Health Sector Semi-Annual Monitoring Report FY2020/21
HEALTH SECTOR SEMI-ANNUAL BUDGET MONITORING REPORT FINANCIAL YEAR 2020/21 MAY 2021 Ministry of Finance, Planning and Economic Development P.O. Box 8147, Kampala www.finance.go.ug MOFPED #DoingMore Health Sector: Semi-Annual Budget Monitoring Report - FY 2020/21 A HEALTH SECTOR SEMI-ANNUAL BUDGET MONITORING REPORT FINANCIAL YEAR 2020/21 MAY 2021 MOFPED #DoingMore Ministry of Finance, Planning and Economic Development TABLE OF CONTENTS ABBREVIATIONS AND ACRONYMS .............................................................................iv FOREWORD.........................................................................................................................vi EXECUTIVE SUMMARY ..................................................................................................vii CHAPTER 1: INTRODUCTION .........................................................................................1 1.1 Background ........................................................................................................................1 CHAPTER 2: METHODOLOGY........................................................................................2 2.1 Scope ..................................................................................................................................2 2.2 Methodology ......................................................................................................................3 2.2.1 Sampling .........................................................................................................................3 -

Nakawa Division Grades
DIVISION PARISH VILLAGE STREET AREA GRADE NAKAWA BUGOLOBI BLOCK 1 TO24 LUTHULI 4TH CLOSE 2-9 1 NAKAWA BUGOLOBI BLOCK 1 TO25 LUTHULI 1ST CLOSE 1-9 1 NAKAWA BUGOLOBI BLOCK 1 TO26 LUTHULI 5TH CLOSE 1-9 1 NAKAWA BUGOLOBI BLOCK 1 TO27 LUTHULI 2ND CLOSE 1-10 1 NAKAWA BUGOLOBI BLOCK 1 TO28 LUTHULI RISE 1 NAKAWA BUGOLOBI BUNGALOW II MBUYA ROAD 1 NAKAWA BUGOLOBI BUNGALOW II MIZINDALO ROAD 1 NAKAWA BUGOLOBI BUNGALOW II MPANGA CLOSE 1 NAKAWA BUGOLOBI BUNGALOW II MUZIWAACO ROAD 1 NAKAWA BUGOLOBI BUNGALOW II PRINCESS ANNE DRIVE 1 NAKAWA BUGOLOBI BUNGALOW II ROBERT MUGABE ROAD. 1 NAKAWA BUGOLOBI BUNGALOW II BAZARRABUSA DRIVE 1 NAKAWA BUGOLOBI BUNGALOW II BINAYOMBA RISE 1 NAKAWA BUGOLOBI BUNGALOW II BINAYOMBA ROAD 1 NAKAWA BUGOLOBI BUNGALOW II BUGOLOBI STREET 1 NAKAWA BUGOLOBI BUNGALOW II FARADAY ROAD 1 NAKAWA BUGOLOBI BUNGALOW II FARADY ROAD 1 NAKAWA BUGOLOBI BUNGALOW II HUNTER CLOSE 1 NAKAWA BUGOLOBI BUNGALOW II KULUBYA CLOSE 1 NAKAWA BUGOLOBI BUNGALOW I BANDALI RISE 1 NAKAWA BUGOLOBI BUNGALOW I HANLON ROAD 1 NAKAWA BUGOLOBI BUNGALOW I MUWESI ROAD 1 NAKAWA BUGOLOBI BUNGALOW I NYONDO CLOSE 1 NAKAWA BUGOLOBI BUNGALOW I SALMON RISE 1 NAKAWA BUGOLOBI BUNGALOW I SPRING ROAD 1 NAKAWA BUGOLOBI BUNGALOW I YOUNGER AVENUE 1 NAKAWA BUKOTO I KALONDA KISASI ROAD 1 NAKAWA BUKOTO I KALONDA SERUMAGA ROAD 1 NAKAWA BUKOTO I MUKALAZI KISASI ROAD 1 NAKAWA BUKOTO I MUKALAZI MUKALAZI ROAD 1 1 NAKAWA BUKOTO I MULIMIRA OFF MOYO CLOSE 1 NAKAWA BUKOTO I NTINDA- OLD KIRA ZONE NTINDA- OLD KIRA ROAD 1 NAKAWA BUKOTO I OLD KIRA ROAD BATAKA ROAD 1 NAKAWA BUKOTO I OLD KIRA ROAD LUTAYA -
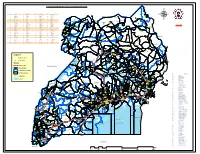
Legend " Wanseko " 159 !
CONSTITUENT MAP FOR UGANDA_ELECTORAL AREAS 2016 CONSTITUENT MAP FOR UGANDA GAZETTED ELECTORAL AREAS FOR 2016 GENERAL ELECTIONS CODE CONSTITUENCY CODE CONSTITUENCY CODE CONSTITUENCY CODE CONSTITUENCY 266 LAMWO CTY 51 TOROMA CTY 101 BULAMOGI CTY 154 ERUTR CTY NORTH 165 KOBOKO MC 52 KABERAMAIDO CTY 102 KIGULU CTY SOUTH 155 DOKOLO SOUTH CTY Pirre 1 BUSIRO CTY EST 53 SERERE CTY 103 KIGULU CTY NORTH 156 DOKOLO NORTH CTY !. Agoro 2 BUSIRO CTY NORTH 54 KASILO CTY 104 IGANGA MC 157 MOROTO CTY !. 58 3 BUSIRO CTY SOUTH 55 KACHUMBALU CTY 105 BUGWERI CTY 158 AJURI CTY SOUTH SUDAN Morungole 4 KYADDONDO CTY EST 56 BUKEDEA CTY 106 BUNYA CTY EST 159 KOLE SOUTH CTY Metuli Lotuturu !. !. Kimion 5 KYADDONDO CTY NORTH 57 DODOTH WEST CTY 107 BUNYA CTY SOUTH 160 KOLE NORTH CTY !. "57 !. 6 KIIRA MC 58 DODOTH EST CTY 108 BUNYA CTY WEST 161 OYAM CTY SOUTH Apok !. 7 EBB MC 59 TEPETH CTY 109 BUNGOKHO CTY SOUTH 162 OYAM CTY NORTH 8 MUKONO CTY SOUTH 60 MOROTO MC 110 BUNGOKHO CTY NORTH 163 KOBOKO MC 173 " 9 MUKONO CTY NORTH 61 MATHENUKO CTY 111 MBALE MC 164 VURA CTY 180 Madi Opei Loitanit Midigo Kaabong 10 NAKIFUMA CTY 62 PIAN CTY 112 KABALE MC 165 UPPER MADI CTY NIMULE Lokung Paloga !. !. µ !. "!. 11 BUIKWE CTY WEST 63 CHEKWIL CTY 113 MITYANA CTY SOUTH 166 TEREGO EST CTY Dufile "!. !. LAMWO !. KAABONG 177 YUMBE Nimule " Akilok 12 BUIKWE CTY SOUTH 64 BAMBA CTY 114 MITYANA CTY NORTH 168 ARUA MC Rumogi MOYO !. !. Oraba Ludara !. " Karenga 13 BUIKWE CTY NORTH 65 BUGHENDERA CTY 115 BUSUJJU 169 LOWER MADI CTY !. -

Acknowledgement: the Authors Are Grateful for Financial Support from the Netherlands Ministry of Agriculture, Nature and Food Qu
PARTNERSHIPS FOR HEALTHY DIETS AND NUTRITION IN URBAN AFRICAN FOOD SYSTEMS – EVIDENCE AND STRATEGIES “THE KANYANYA FOOD CHALLENGE – FOOD SYSTEMS MAPPING” PROGRESS REPORT DELIVERABLE WP1: NOURICITY - KAMPALA Vincent Linderhof, Youri Dijkxhoorn (both Wageningen Economic Research), Joel Onyango (BoP innovation centre), Andrea Fongar (Bioversity International), and Martha Nalweyiso Date of the report 31-12-2019 Acknowledgement: The authors are grateful for financial support from the Netherlands Ministry of Agriculture, Nature and Food Quality (grant number BO-43-003.02-009 as part of LEAP-Agri program), and the flagship program Food Systems for Healthier Diets of the CGIAR program Agriculture for Nutrition and Health (A4NH). 1 | The Kanyanya food challenge Contents Glossary ............................................................................................................................ 3 List of figures ..................................................................................................................... 5 List of tables ...................................................................................................................... 6 1 Introduction ................................................................................................................. 7 2 Desk study ................................................................................................................... 8 1.1 2.1 Description of Kampala .................................................................................... 8 -

Kampala City
KAMPALA CITY Stimulus Paper PASCAL International Exchanges Dr. Joseph Oonyu and Dr. Josephine Esaete, School of Education College of Education and External Studies, Makerere University __________________________________________________________________________ 2 Kampala City has evolved from a small town of 8 km through a “City of Seven hills” at independence in 1962 to one of the fastest growing cities in Africa. Today Kampala City occupies more than twenty five hills that include Makerere Hill on which the country‟s biggest and oldest university is located (Kibirige, 2006). The hills have steep slopes separated by wide valleys. The city derives its name from the land of “Impala” (antelope) that roamed the area before it was taken over for human settlement. The first administrative post was set up at Old Kampala Hill by Lord Lugard (British Administrator) in 1890 covering an area of 0.68 km2. It was gazetted into a town council in 1906 with an area of 8 km2 and was extended to cover an area of approximately 195 km2 in 1968. In 1962, Kampala replaced Entebbe as the capital of Uganda. Despite its proximity (32 km) to the equator, the city has a moderate climate, largely because of its altitude (about 1,220 m). Kampala City is located in the central region of the country, which experienced the first contact with European Missionaries and Arab traders at the turn of the previous century. The City today has grown into a commercial, educational, cultural and administrative centre of Uganda with an approximate population of 2.5 million people. Considering that the population was 330,700 in 1969, 1,208,544 million in 2002, and 1,811.794 in 2010, this signals rapid urbanization in the country. -
Owned Spaces and Shared Places
UGANDA Owned Spaces and Shared Places: Refugee Access to Livelihoods and Housing, Land, and Property in Uganda September 2019 Cover photo: Kyaka II refugee settlement. © IMPACT/2019 About REACH REACH Initiative facilitates the development of information tools and products that enhance the capacity of aid actors to make evidence-based decisions in emergency, recovery and development contexts. The methodologies used by REACH include primary data collection and in-depth analysis, and all activities are conducted through inter-agency aid coordination mechanisms. REACH is a joint initiative of IMPACT Initiatives, ACTED and the United Nations Institute for Training and Research - Operational Satellite Applications Programme (UNITAR-UNOSAT). For more information please visit our website: www.reach-initiative.org. You can contact us directly at: [email protected] and follow us on Twitter @REACH_info. About Norwegian Refugee Council The Norwegian Refugee Council is an independent humanitarian organisation working to protect the rights of displaced and vulnerable people during crises. NRC provides assistance to meet immediate humanitarian needs, prevent further displacement and contribute to durable solutions. NRC is Norway’s largest international humanitarian organisation and widely recognised as a leading field-based displacement agency within the international humanitarian community. NRC is a rights-based organisation and is committed to the humanitarian principles of humanity, neutrality, independence and impartiality. Refugee Access to Livelihoods and Housing, Land, and Property in Uganda – September 2019 AWKNOWLEDGEMENTS REACH Initiative and NRC would like to thank the government of Uganda’s Office of the Prime Minister (OPM) and the United Nations Commissioner for Refugees (UNHCR) for their assistance in designing and guiding this assessment.