Annual Report 2016 for YEAR 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Regeltillämpning På Kommunal Nivå Undersökning Av Sveriges Kommuner 2020
Regeltillämpning på kommunal nivå Undersökning av Sveriges kommuner 2020 Kalmar län Handläggningstid i veckor (Serveringstillstånd) Kommun Handläggningstid 2020 Handläggningstid 2016 Serveringstillstånd Borgholm 3 7 Kalmar 3 3 Hultsfred 4 5 Högsby 4 5 Emmaboda 6 8 Medelvärde Nybro 6 8 handläggningstid 2020 Torsås 6 6 Sverige: 5,7 veckor Vimmerby 6 Gruppen: 5,7 veckor Västervik 6 6 Medelvärde Mönsterås 8 6 handläggningstid 2016 Mörbylånga 8 5 Sverige: 6,0 veckor Oskarshamn 8 8 Gruppen: 6,1 veckor Handläggningstid i veckor (Bygglov) Kommun Handläggningstid 2020 Handläggningstid 2016 Bygglov Högsby 1 4 Nybro 1 4 Kalmar 2 2 Borgholm 4 3 Västervik 4 4 Medelvärde Emmaboda 5 8 handläggningstid 2020 Oskarshamn 5 5 Sverige: 4,0 veckor Mönsterås 6 5 Gruppen: 3,8 veckor Torsås 6 5 Medelvärde Hultsfred 5 handläggningstid 2016 Mörbylånga 3 Sverige: 4,0 veckor Vimmerby 5 Gruppen: 4,4 veckor Servicegaranti (Bygglov) Servicegaranti Dagar Digitaliserings- Servicegaranti Dagar Kommun Bygglov 2020 2020 grad 2020 2016 2016 Borgholm Nej 0,5 Ja Emmaboda Nej 0,5 Nej Hultsfred Nej Högsby Ja 42 0 Ja 42 Servicegaranti 2020 Kalmar Ja 28 1 Ja 28 Sverige: 19 % Ja Mönsterås Nej 1 Ja 28 Gruppen: 33 % Ja Mörbylånga Nej Digitaliseringsgrad 2020 Nybro Nej 0 Sverige: 0,52 Oskarshamn Ja 35 0 Nej Gruppen: 0,5 Torsås Nej 0,5 Nej Servicegaranti 2016 Vimmerby Nej Sverige: 30 % Ja Västervik Nej 1 Nej Gruppen: 36 % Ja Tillståndsavgifter (Serveringstillstånd) Kommun Tillståndsavgift 2020 Tillståndsavgift 2016 Serveringstillstånd Mönsterås 6 000 6 000 Oskarshamn 7 600 7 600 Hultsfred -
Oskarshamn 1 and 2 in Sweden
General data in accordance with the requirements in article 37 of the Euratom Treaty Dismantling of the nuclear reactors Oskarshamn 1 and 2 in Sweden 11th May 2017 2 About this report The present document has been compiled and completed by the Swedish Radiation Safety Authority (SSM), mainly based on information provided by the license holder, OKG AB. The purpose of the document is to serve as information for the European Commission, and to fulfil the requirements of Article 37 of the Euratom Treaty. SSM has controlled that the general data provides the necessary information and that it follows the guideline in annex 3 of the recommendation of the application of Article 37 of the Euratom Treaty 2010/635/Euratom. The report has been approved by the Head of Section Ove Nilsson and has been registered by the authority with document number SSM20017-333-2. On the 11th of May 2017 SSM approved to submit the report to the Swedish Government in order to be submitted to the European Commission. 3 4 Summary The recommendation of the European Commission of 11 October 2010 on the application of Article 37 of the Euratom Treaty (2010/635/Euratom) requires each member state to provide the Commission with general data related to for instance dismantling of nuclear reactors, which will make it possible to determine whether the implementation of the activities is likely to result in radioactive contamination of the water, soil or airspace of another member state. This report describes the consequences of decommissioning two boiling water reactors and the common waste handling building at the Oskarshamn Nuclear Power Plant. -

Hultsfred Högsby Mönsterås Nybro Oskarshamn
544800 549800 554800 559800 564800 569800 574800 579800 15°45'0"E 15°50'0"E 15°55'0"E 16°0'0"E 16°5'0"E 16°10'0"E 16°15'0"E 16°20'0"E Lillesjövägen Skiren GLIDE number: N/A Activation ID: EMSR-009 Product N.: 03Ruda, v1 F i Saxtorp n n s j e ö g v L n ä ä Ruda - SWEDEN v i e V l g g ö l e j e ä t v e F l s s ö n i a e sj n n l j Finsjöväg s Flood - 07/07/2012 d il ö L lle en jö v i v a L ille L ä v ä s g Reference Map - Overview ä e g jö n g e v e ä n g Production date: 11/07/2012 n e L n ille sj ö N v " ä 0 g ' 0 e 2 n ° 0 0 7 5 0 L 0 9 9 N " 4 n il 4 0 l ' 5 e L e 5 0 3 g s 3 2 il ° 6 ä l j illesjö 6 7 e ö L v v äge 5 n s v ö j j ä s ö g v le e il ä n L g e L n ill L esjöv i äg l en l Mörlunda e s Lillesjövägen j ö ägen v Lillesjöv ä n g ge e ä n v sjö le Lil Lillesjövägen n e Lillesjövägen Li äg lle öv sj sj öv ille äg L Hultsfred en Lillesjövägen Oskarshamn 0 0 0 0 9 9 9 9 4 4 Cartographic Information 3 3 6 6 1:60,000 Full color ISO A1, medium resolution (200 dpi) Lillesjövägen n Å e 0 1.25 2.5 5 s g vä ä km ge v ö n j n Finsjö s e Lillesjövägen vä n F g g i ins Map Coordinate System: WGS 1984 UTM Zone 33N vä en jövägen en ö F väg sj Finsjö le Lil Graticule: WGS 84 geographical coordinates il lesjö ± L väg en Lillesjövägen en jöväg Bockara Fins en Legend Åsvä väg Emån gen Ås General Information Transportation Artificial Area N " 0 ' 5 Area of Interest Primary Road Built-Up Area 1 ° 7 5 N " Secondary Road Hydrology 0 ' District of City 5 n 1 ° e 7 5 g Water Bodies 0 0 0 ä 0 Local Road 9 v 9 4 ö 4 j 4 s 4 3 3 n 6 i 6 Other Point of -
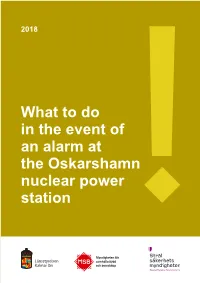
What to Do in the Event of an Alarm at the Oskarshamn Nuclear Power Station the “Important Public Announcement” Signal
2018 What to do in the event of an alarm at the Oskarshamn nuclear power station The “Important public announcement” signal Important public announcement 14 14 7 sec 7 7 Danger has passed 30–40 sec long signal What to do if the alarm sounds If you are outside You will be warned via the “Important public announcement” signal (VMA). Tone 7 seconds, silence 14 seconds, tone 7 seconds, etc. • Go inside. You have better protection inside than outside. 2 If you are inside You will receive the alarm signal as the RDS receiver activates and Sveriges Radio P4 reads an announcement. • Shut doors, windows and ventilation. This will keep out contaminated air. • Listen to Sveriges Radio P4 Kalmar. The station will broadcast news about what has happened and what you need to do. • Help others. Bring persons in need of protection indoors. • Stay inside. Do not go outside before the announcement that danger has passed has been made on Sveriges Radio P4 Kalmar. Protect animals • Keep pets indoors. • Listen to Sveriges Radio P4 Kalmar for advice about grazing animals, pigs and other domestic animals. Measures that may become necessary: • Bring in animals that are outside, the first priority being milk cows. • If possible, shut doors and windows of animal stalls and barns containing fodder. • Avoid using water from shallow open bodies of water or ditches. Important public announcement (VMA) If you were not at home when a VMA was broadcast, you can obtain information on what has happened at www.svt.se and SVT Text-TV, page 100, as long as a VMA situation is ongoing. -
Guideprogram "Naturupplevelser 2021 I Kalmar Läns Skyddade Natur
Naturupplevelser i Kalmar läns skyddade natur 2021 Covid information Eftersom det även i år är ett annorlunda år så ber vi om att ni till våra guidningar anmäler er till guiderna som anges i programmet. Välkommen ut i naturen! Till de flesta guidningarna är det obligatorisk anmälan till Tillsammans med många duktiga aktörer från guiden, antalet personer på guidningarna varierar bero- hela länet erbjuder Länsstyrelsen Kalmar län ende på guidning och guide. Var vänlig att respektera dig upplevelser utöver det vanliga. Här finns detta. guidade vandringar, slåttergillen, båtturer, Som ni förstår så kan förutsättningarna för vår guidningar äventyr i sommarnatten, närkontakt med fort ändras, så vi hoppas att ni har överseende med detta. ovanliga växter och djur och framför allt Har du frågor kring en guidning, kontakta guiden så får du – en stor portion äkta engagemang för vår klart besked om vad som gäller. gemensamma skyddade natur. Med förhoppningar om den fin guidning och en skön Varmt välkomna ut! stund ute i vår fantaskiska natur. Ängshök Circus pygargus Vandringarna och arrangemangen sker i samverkan mellan Länsstyrelsen Kalmar län, Länsstyrelsen Jönköpings län, Kalmar läns museum, Rumskulla hembygdsförening, Tjust naturskyddsförening, Sevedebygdens naturskyddsförening, Trollsländeföreningen, Mönsterås kommun, Biologiska Sällskapet i Oskarshamn, Nybro kommun, Västerviks museum, Station Linné, länets naturum samt lokala naturguider över hela länet. Sjön Allgunnen Ängshök Foto: Martin Lagerlöf Foto: Mats Wallin Vindskydden på Blå jungfrun Foto: Oskar Lind ”Efter den sista mödosamma stigningen upp mot toppen så sitter jag här. Jag smeker med handen över några skrovliga ristningar i stenen bredvid mig. Det är en hälsning från en av alla de som arbetade med stenbrytningen här ute i början av förra seklet. -

ESPON PROFECY Annex 16. Case Study Report. Vimmerby (Sweden)
PROFECY – Processes, Features and Cycles of Inner Peripheries in Europe (Inner Peripheries: National territories facing challenges of access to basic services of general interest) Applied Research Final Report Annex 16 Case Study Report Vimmerby (Sweden) Version 07/12/2017 This Applied Research Project is conducted within the framework of the ESPON 2020 Cooperation Programme, partly financed by the European Regional Development Fund. The ESPON EGTC is the Single Beneficiary of the ESPON 2020 Cooperation Programme. The Single Operation within the programme is implemented by the ESPON EGTC and co-financed by the European Regional Development Fund, the EU Member States and the Partner States, Iceland, Liechtenstein, Norway and Switzerland. This delivery does not necessarily reflect the opinion of the members of the ESPON 2020 Monitoring Committee. Authors Anna Berlina, Gunnar Lindberg and John Moodie - Nordregio (Sweden) Advisory Group Project Support Team: Barbara Acreman and Zaira Piazza (Italy), Eedi Sepp (Estonia), Zsolt Szokolai, European Commission. ESPON EGTC: Marjan van Herwijnen (Project Expert), Laurent Frideres (HoU E&O), Ilona Raugze (Director), Piera Petruzzi (Outreach), Johannes Kiersch (Financial Expert). Information on ESPON and its projects can be found on www.espon.eu. The web site provides the possibility to download and examine the most recent documents produced by finalised and ongoing ESPON projects. This delivery exists only in an electronic version. © ESPON, 2017 Printing, reproduction or quotation is authorised provided the source is acknowledged and a copy is forwarded to the ESPON EGTC in Luxembourg. Contact: [email protected] a PROFECY – Processes, Features and Cycles of Inner Peripheries in Europe ESPON 2020 i Table of contents Abbreviations ............................................................................................................................ -

Möten I Parken
Möten i parken Magdalena Jonsson, Veronica Olofsson KALMAR LÄNS MUSEUM Kulturhistorisk rapport 2014 Möten i parken Meddelandeserien nr 2014:13 ISSN-nummer 0348-8748 Utgiven av Länsstyrelsen Kalmar län Ansvarig avd/enhet Kulturmiljöenheten Författare Magdalena Jonsson, Veronica Olofsson Omslagsbild Stadsparken Kalmar Fotograf omslagsbild Liselotte Jumme Tryckt hos Kalmar läns museum Upplaga 13 ex MÖTEN I paRKEN 3 Innehåll Förord 5 Inledning och syfte 7 Stadsparker 9 Stadsparken i Oskarhamn 11 Presentation av parken 11 Historik 11 Parken idag 20 Parken i framtiden 29 Parkens värden 31 Bevarande-, vård- och informationsinsatser 33 Stadsparken i Kalmar 35 Presentation av parken 35 Historik 36 Parken idag 45 Parken i framtiden 49 Parkens värden 51 Bevarande-, vård- och informationsinsatser 52 Jämförelsen mellan stadsparkerna 54 Folkparker 55 Folkets park i Oskarshamn 57 Presentation av parken 57 Historik 57 Folkparksminnen 64 Parken idag 67 Parken i framtiden 71 Parkens värden 72 Bevarande-, vård- och informations insatser 73 Folkets park i Kalmar 75 Presentation av parken 75 Historik 75 Parken idag 83 Parken i framtiden 85 Parkens värden 88 Bevarande-, vård- och informationsinsatser 89 Jämförelse mellan folkparkerna 90 Avslutningsvis 91 Källor 93 4 MÖTEN I paRKEN MÖTEN I paRKEN 5 Förord 6 MÖTEN I paRKEN Stadsparken i Oskarshamn hösten 2013. MÖTEN I paRKEN 7 Inledning och syfte På uppdrag av Länsstyrelsen i Kalmar län har De privatpersoner som intervjuats är slump- Bebyggelseenheten på Kalmar läns museum ar- vis utvalda till exempel genom att personer i betat med projektet ”Möten i parken”. Arbetet parken eller i verksamheter i anslutning till par- har utförts under hösten 2013 av antikvarierna ken tillfrågats. -

The Swedish Hip Arthroplasty Register Annual Report 2017
Swedish Hip Arthroplasty Register Annual Report 2017 We cannot be held liable for any errors that may occur in printing, information and/or data files. Publisher: Ola Rolfson ISBN (English pdf version): 978-91-984239-4-5 ISSN 1654-5982 Swedish Hip Arthroplasty Register Annual Report 2017 Johan Kärrholm Maziar Mohaddes Daniel Odin Johanna Vinblad Cecilia Rogmark Ola Rolfson 4 SWEDISH HIP ARTHROPLASTY REGISTER 2017 Contents 1 Introduction 6 2 Data quality and validation process 8 2.1 Completeness analysis 8 2.2 Completeness analysis per unit 8 2.3 PROM programme, data quality 10 2.4 Missing variables 10 2.5 Validation processes 10 3 Epidemiology, availability, and gender aspects 15 3.1 Total hip arthroplasty in Sweden 15 3.2 County council production and geographical inequality 16 3.3 Gender division, elective patients 16 3.4 Gender division, fracture patients 19 4 Register development, improvement work and research 22 4.1 Implant manufacturer application 22 4.2 From worst to above the national average through systematic improvement work 22 4.4 Long-term results following total hip arthroplasty 24 5 Register work from an international perspective 26 5.1 International studies 26 5.2 ISAR Congress 2018 27 6 Primary prosthesis 28 6.1 Demographics 28 6.2 Diagnosis 28 6.3 BMI and ASA classification 28 6.4 Prosthesis selection 29 6.5 Most common prostheses 29 6.6 Articulation 33 6.7 Implant combinations 33 6.8 Surgical approach 33 7 Primary prosthesis – in-depth analyses 42 7.1 ‘New’ primary prosthesis 42 8 Reoperation 49 8.1 Definition and trends -

Verksamhetsberättelse 2008
VERKSAMHETSBERÄTTELSE 2008 SVENSKA FOTBOLLFÖRBUNDET INNEHÅLL Förbundsmötet 2009 ...................................................... 1 Inledning ............................................................................. 2 Organisationen ................................................................ 6 Internationella uppdrag................................................. 9 Nämndrapporter ............................................................10 Kommittérapporter .......................................................12 Representantskapets rapport ....................................24 Swedbank Arena .............................................................25 Herrlandslaget .................................................................26 Damlandslaget ...............................................................28 UEFA U21-EM 2009 ........................................................30 Årets bästa svenska Årsredovisning fotbollsspelare Förvaltningsberättelse .................................................31 Zlatan Ibrahimovic och Frida Östberg tilldelades Ekonomisk redovisning ................................................33 2008 Guldbollen res- Revisionsberättelse ........................................................49 pektive Diamantbollen som årets bästa svenska Förslag verksamhetsplan och budget 2009 .........50 fotbollsspelare. Zlatan Resultatanalys 2008 .......................................................52 blev därmed historisk som den förste att vinna tre Resultat och statistik .....................................................54 -

Nulägesbeskrivning
Bilaga 1 Nulägesbeskrivning Arbetsmaterial - juli 2020 Arbetsmaterial - juli 2020 Innehåll 1. Kommunal avfallsorganisation ....................................................................................... 4 2. Beskrivning av KSRR:s verksamhetsområde ................................................................ 5 2.1 Geografiskt läge och infrastruktur .................................................................................5 Bilaga 1 1 Bilaga 2.2 Befolkning ...........................................................................................................................6 2.3 Näringslivsstruktur .............................................................................................................7 3. Avfallsmängder .................................................................................................................. 8 3.1 Avfall som omfattas av kommunalt renhållningsansvar ..........................................8 3.2 Avfall som omfattas av producentansvar ....................................................................9 3.4 Jämförelse med andra kommuner...............................................................................10 3.5 Mat-och restavfallets sammansättning ........................................................................11 Ska detta vara med? ................................................................................................................12 Hör till 3.4 ...................................................................................................................................12 -

Feasibility Studies - Osthammar, Nykoping, Oskarshamn, Tierp, Hultsfred and Alvkarleby
SE0100208 Technical Report TR-01-16 Feasibility Studies - Osthammar, Nykoping, Oskarshamn, Tierp, Hultsfred and Alvkarleby Summary Report Svensk Karnbranslehantering AB June 2001 Svensk Karnbranslehantering AB Swedish Nuclear Fuel and Waste Management Co Box 5864 SE-102 40 Stockholm Sweden Tel 08-459 84 00 +46 8 459 84 00 Fax 08-661 57 19 +46 8 661 57 19 S 9 I 4 S PLEASE BE AWARE THAT ALL OF THE MISSING PAGES IN THIS DOCUMENT WERE ORIGINALLY BLANK Preface Svensk Karnbranslehantering AB (Swedish Nuclear Fuel and Waste Management Com- pany), SKB, has carried out feasibility studies on a municipal scale as a part of the siting programme for the deep repository for spent nuclear fuel. Final reports describing the results of the six feasibility studies in Osthammar, Nykoping, Oskarshamn, Tierp, Alv- karleby and Hultsfred were submitted during the autumn and winter of 2000/2001. With this as a basis, the siting work can now proceed to the next phase - site investigations. In this stage, investigations that include test drilling will be conducted on at least two sites. In December 2000, SKB published the report "Integrated account of method, site selec- tion and programme prior to the site investigation phase," in which SKB stipulates where they want to conduct site investigations and how they will be carried out. The report is being reviewed by the Swedish Nuclear Power Inspectorate during the first half of 2001. Before the site investigations can be initiated, the go-ahead is required from the national safety authorities, the Government, and concerned municipalities and landowners. SKB projects that the it will be possible to commence the site investigations in 2002. -

Landstingslistor För Vänsterpartiet Kalmar
Landstingslistor Vänsterpartiet Kalmar län 2018-2022 Kalmar 1. Linda Fleetwood, Kalmar, lärare/landstingsråd 2. Ragnar Olsson, Kalmar, lärare 3. Josefin Hellvin, Kalmar, undersköterska 4. Ylva Bengtsson, Mörbylånga, pensionär 5. Gylfi Saemundsson, Kalmar, pensionär 6. Sara Kånåhols, Borgholm, egenföretagare 7. Martin Ottosson, Borgholm, 8. Maria Persson Engman, Kalmar, omsorgsassistent 9. Michael Ben Larbi Palmqvist, Kalmar, industriarbetare 10. Anita Strömberg, Nybro, undersköterska 11. Jens Körge, Kalmar, skärgårdskapten 12. Karin Olsson, Mörbylånga, egenföretagare 13. Per Gawelund, Kalmar, sjuksköterska Öland 1. Martin Ottosson, Borgholm, 2. Ylva Bengtsson, Mörbylånga, pensionär 3. Sara Kånåhols, Borgholm, egenföretagare 4. Linda Fleetwood, Kalmar, lärare/landstingsråd 5. Gylfi Saemundsson, Kalmar, pensionär 6. Karin Olsson, Mörbylånga, egenföretagare 7. Lars-Erik Larsson, Borgholm 8. Eva Sigfridsson, Borgholm 9. Erik Cardfelt, Mörbylånga, egenföretagare 10. Maria Persson Engman, Kalmar, omsorgsassistent 11. Ulf Lafveskans, Borgholm 12. Josefin Hellvin, Kalmar, undersköterska 13. Sten-Olof Söderlund, Mörbylånga Nybro/Emmaboda/Torsås 1. Linda Fleetwood, Kalmar, lärare/landstingsråd 2. Jonny Andersson, Nybro, pensionär 3. Anita Strömberg, Nybro, undersköterska 4. Jens Stenman, Vimmerby, demokratiutvecklare 5. Pia Eriksson, Nybro, trätekniker 6. Nicke Grozdanovski, Emmaboda, skolbibliotekarie 7. Lena Gustavsson, Torsås, pensionär 8. Bassel Darkashli, Nybro, fritidsledare 9. Gunilla Modin, Torsås 10. Ali Mobaraki, Nybro, lärare 11. Carina