IRC) Panyijiar County, Unity State South Sudan Comprehensive Emergency Response in South Sudan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
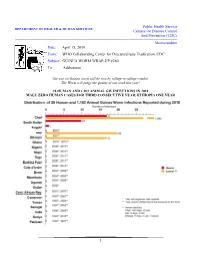
1 Public Health Service Centers for Disease Control and Prevention (CDC) Memorandum Date: April 15, 2019 From: WHO Coll
Public Health Service DEPARTMENT OF HEALTH & HUMAN SERVICES Centers for Disease Control And Prevention (CDC) Memorandum Date: April 15, 2019 From: WHO Collaborating Center for Dracunculiasis Eradication, CDC Subject: GUINEA WORM WRAP-UP #260 To: Addressees The war on Guinea worm will be won by village-to-village combat. The Worm will judge the quality of our work this year! 28 HUMAN AND 1,102 ANIMAL GW INFECTIONS IN 2018 MALI: ZERO HUMAN CASES FOR THIRD CONSECUTIVE YEAR; ETHIOPIA ONE YEAR 1 Chad reported 96% of all Guinea worms remaining Table 1 in the world in 2018, with 1,040 infected dogs (328 Number of Province District villages), 17 human cases (11 villages) and 25 infected dogs infected cats (20 villages), in a total of 340 villages Chari Baguirmi Mandelia 150 Bailli 129 with one or more Guinea worm infections in Chad Bousso 72 in 2018. Two villages in Salamat Province had 4 Massenya 44 and 3 human cases, respectively. The Guinea worm Dourbali 39 Kouno 21 infected dogs occurred in 21 districts of 7 provinces. Sub Total 455 Moyen Chari Sarh 160 The status of interventions against Guinea worm Kyabe 120 infections in Chad as of the end of 2018 is Danamadji 70 summarized in Figure 3. Chad’s GWEP Korbol 50 implemented monthly Abate treatments in 83 Biobe 9 villages under active surveillance by the end of Sub Total 409 Mayo Kebbi Est Guelendeng 2018, compared to 21 VAS in October-December 142 Bongor 1 2017, and it applied Abate in response to specific Sub Total 143 contamination events in 71 villages, vs. -

[email protected], Area Mapped Logcluster Office, UNOCHA Compound and Jebel Kajur, Juba South Sudan
Sani Mingyeir Sullu Oubbe Wada`ah Djiri Bajouggi Karaw Balla Nyama Ludung Margibba Arga Gertobak Dalia Zulumingtong Gostoweir El Rahad Gyaga Manawashi En Nahud Duraysah Kurbi Karbab Godoba Silo Arid Limo Menawashei Tebeldina Kurto Kulme Gabir Futajiggi Shurab Zulata Tanako Burbur Seingo Kalamboa Uraydimah Kass Attib Deleig Kalu Dilu Shearia Shaqq Bunzuga al Gawa Galgani Duma Garoula Tangya Korgusa Garsila Kagko Khamis Abu zor Amar Seilo Ballah Umm Marabba Gedid Mogara Dauro Shalkha Harun Tumbo Qawz Beringil Lerwa Baya Saq an Na`am Buhera Sineit Goldober Singeiwa Agra Nyala Labado Sereiwa Baddal Sigeir Dilling Kirarow Tumko Umm Sa Disa Um Kurdus Shaqq Girbanat Kasoleri Buronga Gerger Saheib Mabrouka al Huja El Lait Bendisi Diri Tono Abu Mukjar Ambara Deimbo Buddu El doma Gartaga Abou Sufyan Dalami Artala Shuwayy Rashad El Roseires Um Sarir @Adid Al Muturwed Dashi Wad Abu Kubum Dago Ed Damazin Tetene Keikei Hassib Gheid Renk Nurlei Um Boim Î Damba El kharaba West Lasirei Luma Solwong Murr Njumbeil Agi Abu Ghazal Qubba Girru Ajala Um La`ota Abu Marlenga Ma'aliah 1 Jawazat Karinka Hajar Wajage Markundi Al Marwahah Abu Ma'aliah 2 Banda Dimbala 25°0'0"E 26°0'0"E 27°0'0"E 28°0'0"E 29°0'0"E 30°0'0"EUmm 31°0'0"E 32°0'0"E 33°0'0"E 34°0'0"E 35°0'0"E 36°0'0"E Timassi Ajura heitan Abu Edd el Faki Jibaiha Lujugo Milmeidi Gettin Ibrahim 42Bakau Fursan Kukur Kosua Dambar p Lagawa Sali Kulaykili Abu @ Tabanu Agabullah Adilla Wisko War e ho u se Aradeiba Gereida Manasis Anja C ap a ci t i e s 20 11 Katayla Muhajiriye Abu `Ud Heiban Um- 68Akoc Dukhun Gueighrin -

Central Unity FSL Cluster Response Strategy for 2017
Central Unity FSL Cluster Response Strategy for 2017 Recent contextual development in Central Unity: According to the most recent IPC analysis, released on February 20, 2017, approximately 4.9 million (about 42% of population) people are estimated to be severely food insecure (IPC Phases 3, 4, and 5), from February to April 2017. This is projected to increase to 5.5 million people, (47% of the national population) at the height of the 2017 lean season in July. Table: May – July 2017 IPC projection of food insecurity % of Crisis, Mid-2017 Emergency & State Population Minimal Stressed Crisis Emergency Catastrophe Humanitarian (NBS) Catastrophe Central Equatoria 1,398,316 435,000 470,000 465,000 30,000 - 35.4% Eastern Equatoria 1,010,188 300,000 325,000 310,000 75,000 - 38.1% Jonglei 1,822,086 140,000 485,000 930,000 265,000 - 65.6% Lakes 1,113,716 200,000 415,000 465,000 145,000 - 54.8% Northern Bahr el Ghazal 1,418,111 145,000 410,000 465,000 420,000 - 62.4% Unity 1,124,916 105,000 385,000 430,000 215,000 90,000 65.3% Upper Nile 1,258,323 395,000 395,000 405,000 95,000 - 39.7% Warrap 1,448,812 330,000 665,000 255,000 75,000 - 22.8% Western Bahr el Ghazal 545,565 70,000 190,000 135,000 135,000 - 49.5% Western Equatoria 705,821 340,000 245,000 120,000 5,000 - 17.7% Total 11,845,855 2,460,000 3,985,000 3,980,000 1,460,000 90,000 46.7% The magnitude of these food insecure populations is unprecedented. -

Initial Rapid Needs Assessment (IRNA) Questionnaire, Adior and Nyang-Yirol East, 3 July 2014
IRNA Reporting format – Draft V.1 18 Sept 2012 Initial Rapid Needs Assessment (IRNA) Questionnaire, Adior and Nyang-Yirol East, 3rd July 2014 1 IRNA Reporting format – Draft V.1 18 Sept 2012 Situation Overview Following the Dec 15 2013 political and security incidents in Juba, fighting ensued, in Juba and eventually other parts of the country between Government and AGFs in which, according to the UN thousands of people were killed and thousands more displaced, the majority of them into UN bases. In Jongolei where many civilians were also killed amidst the fighting, about 100,000 also sought refuge in Awerial County in the Lakes where humanitarian agencies are responding to their needs. Although difficult in the beginning, more than 40 humanitarian partners including 5 UN agencies are now responding to the needs of the IDPs in the areas of WASH, Health & Nutrition, NFIs & ES, FSL, Education and Protection. The operation is going on generally smoothly with no major gaps or challenges, and relocation to the new site given by the authorities has now begun. Active hostilities between the government and opposition forces ensued in the months following and in may such locations there have been displacements and human causalities, as well as the destruction, burning and looting of property. In Panyijar County in Unity State fighting between government and opposition forces lead to the destruction of property and livelihoods as well as displacement of civilian populations. RRC in Rumbek received reports that 300 Nuer households had fled fighting and hunger in Panyijar to take refuge in Nyang and Adior Payams in Yirol East County where the two tribes have ties through historical inter-marriage. -

Isaiah Abraham
Tribute To Isaiah Abraham Compiled By of Liberation The PAANLUEL WËL Dark [email protected] Ages http://paanluelwel2011.wordpress.com/ Isaiah Abraham in his own words AU force extension in Darfur, a victory to NCP not to SPLM By Isaiah Abraham* Mar 14, 2006 The drama that led to the extension of African Peacekeeping Forces in Darfur has nothing to do with the Sudan as a whole or SPLM as a party as propagated by those who are against the marginalized people of the Sudan. Darfur is bleeding and should have been saved. The man at the helm of this ‘victory’ is none other than Dr. Lam Akol Ajawin, the Sudanese Foreign Minister from the SPLM Party. Although it is not that easy to satisfy all interests in a coalition the least an astute politician could do or could have done was to compromise not his/her fall back base, no matter the enticement or attraction the players in that political scene. The Minister went out full blast to contradict his boss, President Salva Kiir Mayardit and his colleague in the Government of Southern Sudan (GOSS) Mama Rebecca de Mabior. President Salva was unequivocally pressed that NCP partner is not serious in its willingness to resolve Darfur crisis. Did anybody hear the President or other Southern politicians or the Southern public unease about UN peacekeeping forces intervention in Darfur? Where there demonstrations in the Southern cities in condemnation of the United States or the United Nations or Jan Pronk? Certainly there weren’t and there will not be any protest against presence of UN in any part of the Sudan. -
Unity State SOUTH SUDAN
COMMUNITY CONSULTATION REPORT Unity State SOUTH SUDAN Bureau for Community Security South Sudan Peace and Small Arms Control and Reconciliation Commission United Nations Development Programme European Union The Bureau for Community Security and Small Arms Control under the Ministry of Interior is the Gov- ernment agency of South Sudan mandated to address the threats posed by the proliferation of small arms and community insecurity to peace and development. The South Sudan Peace and Reconciliation Commission is mandated to promote peaceful co-existence amongst the people of South Sudan and advises the Government on matters related to peace. The United Nations Development Programme in South Sudan, through the Community Security and Arms Control Project, supports the CSSAC Bureau strengthen its capacity in the area of community secu- rity and arms control at the national, state and county levels. The consultation process was led by the Government of South Sudan, with support from the European Union. Cover photo: Community members in Abiemnhom sketch their county map on the ground using locally available materials. © CSAC/UNDP COMMUNITY CONSULTATION REPORT Unity State South Sudan Published by South Sudan Bureau for Community Security and Small Arms Control South Sudan Peace and Reconciliation Commission United Nations Development Programme MAY 2012 JUBA, SOUTH SUDAN CONTENTS Acronyms ........................................................................................................................... i Foreword .......................................................................................................................... -

S/2015/902 Security Council
United Nations S/2015/902 Security Council Distr.: General 23 November 2015 Original: English Report of the Secretary-General on South Sudan (covering the period from 20 August to 9 November 2015) I. Introduction 1. The present report is submitted pursuant to Security Council resolution 2241 (2015), by which the Council extended the mandate of the United Nations Mission in South Sudan (UNMISS) until 15 December 2015 and requested me to report on the implementation of the mandate within 45 days. The present report provides an update to my previous report dated 21 August 2015 (S/2015/655) and covers developments from 20 August to 9 November. II. Political developments South Sudan peace process 2. Following the signing in Addis Ababa on 17 August of the Agreement on the Resolution of the Conflict in the Republic of South Sudan by the leaders of the Sudan People’s Liberation Movement/Army in Opposition (SPLM/A in Opposition) and the former detainees, international and regional partners intensified efforts to persuade the President, Salva Kiir, to sign the peace agreement within the 15-day period granted for additional consultations. During a ceremony on 26 August in Juba, the President signed the agreement in the presence of regional leaders and other representatives of the international community. The Government distributed detailed reservations concerning 16 provisions of the agreement. 3. Subsequently, within the 72-hour deadline, the President and the former Vice- President, Riek Machar, each decreed a permanent ceasefire, instructing their forces to cease all military operations, to remain in their current positions and to return fire only in self-defence. -
Unity State SOUTH SUDAN
COMMUNITY CONSULTATION REPORT Unity State SOUTH SUDAN Bureau for Community Security South Sudan Peace and Small Arms Control and Reconciliation Commission United Nations Development Programme European Union The Bureau for Community Security and Small Arms Control under the Ministry of Interior is the Gov- ernment agency of South Sudan mandated to address the threats posed by the proliferation of small arms and community insecurity to peace and development. The South Sudan Peace and Reconciliation Commission is mandated to promote peaceful co-existence amongst the people of South Sudan and advises the Government on matters related to peace. The United Nations Development Programme in South Sudan, through the Community Security and Arms Control Project, supports the CSSAC Bureau strengthen its capacity in the area of community secu- rity and arms control at the national, state and county levels. The consultation process was led by the Government of South Sudan, with support from the European Union. Cover photo: Community members in Abiemnhom sketch their county map on the ground using locally available materials. © CSAC/UNDP COMMUNITY CONSULTATION REPORT Unity State South Sudan Published by South Sudan Bureau for Community Security and Small Arms Control South Sudan Peace and Reconciliation Commission United Nations Development Programme MAY 2012 JUBA, SOUTH SUDAN CONTENTS Acronyms ........................................................................................................................... i Foreword .......................................................................................................................... -

The Conflict in Unity State Describing Events Through 1 July 2015
The Conflict in Unity State Describing events through 1 July 2015 Over the last two months, a Sudan People’s Liberation Army (SPLA) offensive swept through southern Unity state, razing villages, killing civilians, taking cattle, and abducting women. Initially, it seemed as if the offensive had effectively destroyed the Sudan People’s Liberation Army in Opposition (SPLA-IO) as an organized military force in Unity state. In April and May 2015, the SPLA pushed south from Bentiu, the state capital, rapidly overrunning SPLA-IO positions in Guit and Koch counties, before attacking Leer county. These attacks displaced more than a hundred thousand civilians. SPLA forces also pushed northeast from Lakes state, and attacked SPLA-IO positions and villages in Mayendit and Panyijar counties. Having driven the SPLA-IO from southern Unity—the wellspring of rebel support in the state—much of the SPLA involved in the offensive withdrew to Bentiu, before attacking Panakuac, the main SPLA-IO military base on the Sudanese border, and routing the rebels, who fled into Sudan. During the SPLA’s southern offensive, the SPLA-IO generally chose not to engage, and its soldiers slipped into the bush. After the SPLA’s withdrawal, the SPLA-IO rapidly retook the territory it had conceded, and by the end of June, was again present in Leer and Guit counties, as well as in the southern counties of Mayendit and Panyijar. In its campaign in southern Unity, the SPLA were aided by Bul Nuer fighters, recruited by Matthew Puljang, and promised a share in the spoils of war. In mid-June, the state government issued an announcement, which warned that anyone not aligned with the SPLA-IO should move their cattle to Bentiu.