Multivariable Analysis for Complete Resection Rate of 10-20 Mm Non-Metastatic Rectal Neuroendocrine Tumors: a Retrospective Clinical Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
SGS-Safeguards 04910- Minimum Wages Increased in Jiangsu -EN-10
SAFEGUARDS SGS CONSUMER TESTING SERVICES CORPORATE SOCIAL RESPONSIILITY SOLUTIONS NO. 049/10 MARCH 2010 MINIMUM WAGES INCREASED IN JIANGSU Jiangsu becomes the first province to raise minimum wages in China in 2010, with an average increase of over 12% effective from 1 February 2010. Since 2008, many local governments have deferred the plan of adjusting minimum wages due to the financial crisis. As economic results are improving, the government of Jiangsu Province has decided to raise the minimum wages. On January 23, 2010, the Department of Human Resources and Social Security of Jiangsu Province declared that the minimum wages in Jiangsu Province would be increased from February 1, 2010 according to Interim Provisions on Minimum Wages of Enterprises in Jiangsu Province and Minimum Wages Standard issued by the central government. Adjustment of minimum wages in Jiangsu Province The minimum wages do not include: Adjusted minimum wages: • Overtime payment; • Monthly minimum wages: • Allowances given for the Areas under the first category (please refer to the table on next page): middle shift, night shift, and 960 yuan/month; work in particular environments Areas under the second category: 790 yuan/month; such as high or low Areas under the third category: 670 yuan/month temperature, underground • Hourly minimum wages: operations, toxicity and other Areas under the first category: 7.8 yuan/hour; potentially harmful Areas under the second category: 6.4 yuan/hour; environments; Areas under the third category: 5.4 yuan/hour. • The welfare prescribed in the laws and regulations. CORPORATE SOCIAL RESPONSIILITY SOLUTIONS NO. 049/10 MARCH 2010 P.2 Hourly minimum wages are calculated on the basis of the announced monthly minimum wages, taking into account: • The basic pension insurance premiums and the basic medical insurance premiums that shall be paid by the employers. -

The Regeneration of Millennium Ancient City by Beijing-Hangzhou
TANG LEI, QIU JIANJUN, ‘FLOWING’: The Regeneration of Millennium ancient city , 47 th ISOCARP Congress 2011 ‘FLOWING’: The Regeneration of Millennium ancient city by Beijing-Hangzhou Grand Canal ——Practice in Suqian, Jiangsu, China 1 The Millennium ancient city - Suqian Overview 1.1 City Impression Suqian, A millennium ancient city in China, Great Xichu Conqueror Xiangyu's hometown, Birthplace of Chuhan culture, Layers of ancient cities buried. Yellow River (the National Mother River 5,464km) and Beijing-Hangzhou Grand Canal (the National Wisdom River 1794km, declaring the World Cultural Heritage) run through it. With Luoma, Hongze Lake, it has "Two Rivers Two Lakes" unique spatial characteristics. Nowadays Suqian is meeting the challenge of leapfrog development and ‘Livable Cities’ transformation.The city area is 8555 square kilometers and the resident population is 4,725,100. In 2009 its GDP was RMB 82.685 billion, per capita GDP was RMB 1.75 million. It’s industrial structure is19.3:46.3:34.4, level of urbanization is 37.7% 1.2 Superiority Evaluation (1) industrial structure optimized continuously, overall strength increased significantly. (2) people's lives condition Improved. Urban residents per capita disposable income was 12000, increased 11.6% per year; Farmer’s per capita net income was 6,000, increased 8.9% per year. (3) City’s carrying capacity has improved significantly. infrastructure had remarkable results; the process of industrialization and urbanization process accelerated. (4) Good ecological environment. Good days for 331 days, good rate is 90.4%. (5) Profound historical accumulation. the ancient city, the birthplace of Chu and Han culture, the history of mankind living fossil 1.3 Development Opportunities (1) Expansion of the Yangtze River Delta. -
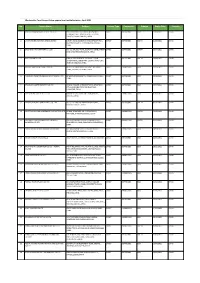
Apparel & Textile Factory List
Woolworths Food Group-Active apparel and textile factories- April 2021 No. Factory Name Address Factory Type Commodity Scheme Expiry Date Country 1 JIANGSU HONGMOFANG TEXTILE CO., LTD EAST CIFU ROAD, EAST RUISHENG AVENUE,, DIRECT SOFTGOODS BSCI 23/04/2021 CHINA ECONOMIC DEVELOPMENT ZONE, SHUYANG COUNTY,,SUQIAN,JIANGSU,,CHINA 2 LIANYUNGANG ZHAOWEN SHOES LIMITED 2 BEIHAI ROAD,ECONOMIC DEVELOPMENT AREA, DIRECT SOFTGOODS SMETA 11/05/2021 CHINA GUANNAN COUNTY,,LIANYUNGANG,JIANGSU,, CHINA 3 ZHUCHENG YIXIN GARMENT CO., LTD NO. 321 SHUNDU ROAD,,ECONOMIC DEVELOPMENT DIRECT SOFTGOODS SMETA 13/07/2021 CHINA ZONE,,ZHUCHENG,SHANDONG,,CHINA 4 HRX FASHION CO LTD 1000 METERS SOUTH OF GUOCANG TOWN DIRECT SOFTGOODS SMETA 25/08/2021 CHINA GOVERNMENT,,WENSHANG COUNTY, JINING CITY, JINING,SHANDONG,,CHINA 5 PUJIANG KINGSHOW CARPET CO LTD NO.75-1 ZHEN PU ROAD, PU JIANG, ZHE JIANG, DIRECT HARDGOODS BSCI 24/12/2021 CHINA CHINA,,PUJIANG,ZHEJIANG,,CHINA 6 YANGZHOU TENGYI SHOES MANUFACTURE CO., LTD. 13 WEST HONGCHENG RD,,,FANGXIANG,JIANGSU,, DIRECT SOFTGOODS BSCI 22/10/2021 CHINA CHINA 7 ZHAOYUAN CASTTE GARMENT CO LTD PANJIAJI VILLAGE, LINGLONG TOWN,,ZHAOYUAN DIRECT SOFTGOODS BSCI 06/07/2021 CHINA CITY, SHANDONG PROVINCE,ZHAOYUAN, SHANDONG,,CHINA 8 RUGAO HONGTAI TEXTILE CO LTD XINJIAN VILLAGE, JIANGAN TOWN,,RUGAO, DIRECT HARDGOODS BSCI 07/12/2021 CHINA JIANGSU,,CHINA 9 NANJING BIAOMEI HOMETEXTILES CO.,LTD NO.13 ERST WUCHU ROAD,HENGXI TOWN,,, DIRECT SOFTGOODS SMETA 04/11/2021 CHINA NANJING,JIANGSU,,CHINA 10 NANTONG YAOXING HOUSEWARE PRODUCTS CO.,LTD NO.999, TONGFUBEI RD., CHONGCHUAN, DIRECT HARDGOODS SMETA 24/09/2021 CHINA NANTONG,,NANTONG,JIANGSU,,CHINA 11 CHAOZHOU CHAOAN ZHENGYUN CERAMICS QIAO HU VILLAGE, CHAOAN, CHAOZHOU CITY, DIRECT HARDGOODS SMETA 19/05/2021 CHINA INDUSTRIAL CO LTD GUANGDONG, CHINA,,CHAOZHOU,GUANGDONG,, CHINA 12 YANTAI PACIFIC HOME FASHION FUSHAN MILL NO. -

Transmissibility of Hand, Foot, and Mouth Disease in 97 Counties of Jiangsu Province, China, 2015- 2020
Transmissibility of Hand, Foot, and Mouth Disease in 97 Counties of Jiangsu Province, China, 2015- 2020 Wei Zhang Xiamen University Jia Rui Xiamen University Xiaoqing Cheng Jiangsu Provincial Center for Disease Control and Prevention Bin Deng Xiamen University Hesong Zhang Xiamen University Lijing Huang Xiamen University Lexin Zhang Xiamen University Simiao Zuo Xiamen University Junru Li Xiamen University XingCheng Huang Xiamen University Yanhua Su Xiamen University Benhua Zhao Xiamen University Yan Niu Chinese Center for Disease Control and Prevention, Beijing City, People’s Republic of China Hongwei Li Xiamen University Jian-li Hu Jiangsu Provincial Center for Disease Control and Prevention Tianmu Chen ( [email protected] ) Page 1/30 Xiamen University Research Article Keywords: Hand foot mouth disease, Jiangsu Province, model, transmissibility, effective reproduction number Posted Date: July 30th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-752604/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 2/30 Abstract Background: Hand, foot, and mouth disease (HFMD) has been a serious disease burden in the Asia Pacic region represented by China, and the transmission characteristics of HFMD in regions haven’t been clear. This study calculated the transmissibility of HFMD at county levels in Jiangsu Province, China, analyzed the differences of transmissibility and explored the reasons. Methods: We built susceptible-exposed-infectious-asymptomatic-removed (SEIAR) model for seasonal characteristics of HFMD, estimated effective reproduction number (Reff) by tting the incidence of HFMD in 97 counties of Jiangsu Province from 2015 to 2020, compared incidence rate and transmissibility in different counties by non -parametric test, rapid cluster analysis and rank-sum ratio. -

Study of the Allocation of Regional Flood Drainage Rights In
International Journal of Environmental Research and Public Health Article Study of the Allocation of Regional Flood Drainage Rights in Watershed Based on Entropy Weight TOPSIS Model: A Case Study of the Jiangsu Section of the Huaihe River, China Kaize Zhang 1,2, Juqin Shen 3, Han Han 1,* and Jinglai Zhang 4 1 Business School, Hohai University, Nanjing 211100, China; [email protected] 2 Department of Ecosystem Science and Management, The Pennsylvania State University, State College, PA 16802, USA 3 College of Agricultural Engineering, Hohai University, Nanjing 210098, China; [email protected] 4 Department of Chemistry, College of Chemistry and Chemical Engineering, Henan University, Kaifeng 475001, China; [email protected] * Correspondence: [email protected] Received: 13 June 2020; Accepted: 10 July 2020; Published: 13 July 2020 Abstract: During the flood season, various regions in a watershed often have flood drainage conflicts, when the regions compete for flood drainage rights (FDR). In order to solve this problem, it is very necessary to study the allocation of FDR among various regions in the watershed. Firstly, this paper takes fairness, efficiency and sustainable development as the allocation principles, and comprehensively considers the differences of natural factors, social development factors, economic development factors and ecological environment factors in various regions. Then, an indicator system for allocation of FDR among regions in the watershed is established. Secondly, an entropy weight Technique for Order Preference by Similarity to Ideal Solution (TOPSIS) model is used to construct the FDR allocation model among regions in the watershed. Based on a harmony evaluation model, a harmony evaluation and comparison are carried out on the FDR allocation schemes under three different allocation principles. -

A Comprehensive Evaluation of the Construction of Innovation Cities In
International Conference on Applied Science and Engineering Innovation (ASEI 2015) A Comprehensive Evaluation of the Construction of Innovation Cities in Xuzhou City Based on Principal Component Analysis Rong xiaohong Institute of information management, Xuzhou College of IndustrialTechnology, Xuzhou, 221140, China. [email protected] Keywords: innovative city; evaluation index; principal component analysis; Abstract. The evaluation of innovation cities assesses the realization level of innovative cities through the evaluation of the comprehensive innovative level. In this paper, the author builds an innovative city competitiveness evaluation index system based on the theoretical analysis, and evaluates Xuzhou city and other 12 prefecture-level cities the innovation capacity through principal component analysis. Alterations made recommendations based on the evaluation results, in order to provide the ability to provide innovative Xuzhou basis for decision making. 1. Introduction In the 21st century, innovation has become the first driver of a country or region’s economic development. Thus "innovative city" has become the focus of academic at home and abroad. Chard Florida[1] has done the city innovation ability evaluation of the United States from the empirical aspects, he adopts the index mainly includes high-tech, innovative, and human resources. EIS[2] thought that an core indicators of innovative city innovation ability included technology, talent and tolerance, which thus created the innovation capability index evaluation method.In the domestic, from the subjective and objective view, Fengxia[3] gives a new urban construction process of evaluation index should at least include ideas, the level of science and technology, system, macro environment and cultural atmosphere and so on five categories of innovation index. -

Research on the Spatial Difference of Public Goods Supply Performance in Jiangsu Province Based on DEA and Malmquist Index
International Journal of Scientific Engineering and Science Volume 3, Issue 12, pp. 30-32, 2020. ISSN (Online): 2456-7361 Research on the Spatial Difference of Public Goods Supply Performance in Jiangsu Province Based on DEA and Malmquist Index Yang Jialiang School of Finance and Economics, Jiangsu University Abstract— With the development of Jiangsu, the improvement of the use of public goods supply performance is very important for Jiangsu's economic development. This paper first uses data envelopment analysis to analyze and evaluate the public goods supply performance in Jiangsu region in 2015, and then uses Malmquist index method to analyze the serial data of 13 cities in Jiangsu Province from 2010 to 2015. The study found that Jiangsu’s public goods supply performance is generally good, but there are still large differences between cities, reflected in scale returns, scale efficiency, and technical efficiency. Based on the results of DEA analysis and Malmquist index analysis of the use of public goods supply performance in cities in Jiangsu Province, this article proposes relevant countermeasures to improve performance. Keywords— Public goods supply; performance; DEA analysis; Malmquist index. performance of the public good and the economic benefits it I. INTRODUCTION brings. That is, DEA analysis method and Malmquist index The existence of public goods is of great significance to the were used to evaluate the performance of Jiangsu public market mechanism, because public goods are non-exclusive goods. and non-competitive, and there is a "free rider" motivation in the consumption of public goods. Economic agglomeration TABLE 1: input and output indicators of Jiangsu in 2015 and the supply of local public goods promote each other, and Input Output Industrial Area Year Fixed assets Economic the supply of local public goods plays a great role in power investment activity promoting regional economic development. -

Final Chien and Wu Formatted
The Transformation of China’s Urban Entrepreneurialism: The Case Study of the City of Kunshan By Shiuh-Shen Chien, National Taiwan University Fulong Wu, University College London Abstract This article examines the formation and transformation of urban entrepreneurialism in the context of China’s market transition. Using the case study of Kunshan, which is ranked as one of the hundred “economically strongest county-level jurisdictions” in the country, the authors argue that two phases of urban entrepreneurialism—one from the 1990s until 2005, and another from 2005 onward—can be roughly distinguished. The first phase of urban entrepreneurialism was more market driven and locally initiated in the context of territorial competition. The second phase of urban entrepreneurialism involves greater intervention on the part of the state in the form of urban planning and top-down government coordination and regional collaboration. The evolution of Kunshan’s urban entrepreneurialism is not a result of deregulation or the retreat of the state. Rather, it is a consequence of reregulation by the municipal government with the goal of territorial consolidation. Introduction There is no doubt that local authorities the world over play a crucial role in promoting economic development in the context of globalization (Harvey 1989; Brenner 2003; Ward 2003; Jessop and Sum 2000). On the one hand, globalization may cause huge unexpected job loss when investors decide to shut down their companies and move out. Capital flight may also create opportunities in a different site. To deal with these challenges and opportunities, local authorities become entrepreneurial in improving their regions, in the hopes of accommodating more business investment and attracting more quality human capital. -

HIV-1 Diversity in Infected Individuals in Suzhou and Suqian, China
Qin et al. SpringerPlus (2016) 5:886 DOI 10.1186/s40064-016-2378-z RESEARCH Open Access HIV‑1 diversity in infected individuals in Suzhou and Suqian, China Chenhao Qin1†, Ping Zhang1†, Weiguang Zhu2, Fangyuan Hao3, Aiping Gu1, Ping Fen1, Xueming Zhu1 and Hong Du1* Abstract Jiangsu is one province with severe HIV-1 epidemic in China. However, the molecular epidemiological characteriza- tions of HIV-1 in many cities of Jiangsu remain unclear. A molecular epidemiological investigation was performed based on 38 HIV-positive samples collected from Suzhou and Suqian during 2011–2013. Five HIV-1 genomic frag- ments, p17, pol, vif-vpr, vpr-env, and C2V3 were amplified and sequenced from these samples. HIV-1 group M subtype of each sample was determined by phylogenetic analyses with the standard reference sequences. Among these infected individuals, 81.6 % (31/38) self-reported to be infected via sexual contacts, including 50.0 % (19/38) via heterosexual contact and 31.6 % (12/38) via homosexual contact. Among 34 samples with available pol or vif-env sequence, 19 (55.9 %) CRF01_AE, 7 (20.6 %) CRF07_BC, 3 (8.8 %) CRF08_BC, and 5 (14.7 %) inter-subtype recombinants were identified. No pure B, ′B and C subtypes were found in this cohort. The five recombinants contain one B/C, three CRF01/B and one CRF01/B/C recombinants. These results suggest that CRF01_AE was the most predominant HIV-1 group M subtype and CRF01_AE-involved recombinants were the major recombinant forms. Comparison showed that there was no obvious difference in HIV-1 group M subtype distribution between Jiangsu (including Suzhou and Suqian) and the surrounding provinces (e.g., Shanghai, Anhui, and Shandong). -

Can Higher Education, Economic Growth and Innovation Ability Improve Each Other?
sustainability Article Can Higher Education, Economic Growth and Innovation Ability Improve Each Other? Haiying Xu 1 , Wei-Ling Hsu 1,* , Teen-Hang Meen 2 and Ju Hua Zhu 3 1 School of Urban and Environmental Science, Huaiyin Normal University, Huai’an 223300, China; [email protected] 2 Department of Electronic Engineering, National Formosa University, Yunlin 632, Taiwan; [email protected] 3 Department of Civil, Environmental and Architectural Engineering, Korea University, Seoul 02841, Korea; [email protected] * Correspondence: [email protected] Received: 25 February 2020; Accepted: 22 March 2020; Published: 23 March 2020 Abstract: This study argues that the coupling between higher education, economic growth, and innovation ability is of great significance for regional sustainable development. Through the experience of Jiangsu Province in China, this study establishes a coupling coordination evaluation index system and applies the coupling coordination model to evaluate interactive relationships among the three. It finds that during 2007–2017, the level of coupling of 13 prefecture-level cities in Jiangsu was increasing over time, which fully verified the previous scholars’ view that the three can improve each other over a long period. However, this study finds that there are obvious differences within Jiangsu. Inadequate investment in higher education has become a crucial constraint on sustainable economic growth in northern and central Jiangsu, which are backward regions of Jiangsu. By contrast, in southern Jiangsu, which is the advanced region of Jiangsu, although the resources of higher education are abundant the growth of innovation ability cannot support sustained economic growth well. Thus, the quality of higher education should be improved to meet the needs of the innovation-based economy. -

World Bank Document
, , ;. * i- t t NCt, . , 5 , , '" C ' i z ; , i 4 'C's-"; + . j? g ,- t Public Disclosure Authorized if .i1; Jr-"In0 V ;It ' ¢q * ? 'IZO . , --9n 2} '? ' > 3' -; - * *C '6 ' ijt ' .. ' jj' '2,'5 rii ', iii; ;j i!.,,i, . 8, j jC' j;' CC'~~~~~~~~~~~~~~~~V Public Disclosure Authorized (C it- 'C '! ' . ' itCC. CCCC . C CC : iCCCC :.,X:. ; '.. ;StC I; CC.C. " ( " C Ji .~ .4 j I X ,' CC.js.,%* i r ' 3mgi;-, s 3, ,',t i ;. a i ,t js;-?. ;,. j$ii ,". - 34 343,4 (C '33 C'~~~is I rC~ C~C~rI /t 'CC CC'C' (0C~~ It ~ ~t~Z t Sd C ~C CC~ CC~~ ~ ~ ~ ~ ~~~~~~~~~~~~~~~4.4 Public Disclosure Authorized Public Disclosure Authorized TABLE OF CONTENTS 1.0 GENERAL SITUATION 1.1 ENVIRONMENTIMPACT ASSESMENT PROCESS 1.2 COMPILATIONBASIS OF THE ENVIRONMENTIMPACT REPORTON THE PROJECTAND THE ENVIRONMENT ASSESMENT STANDARDS 1.3 ENVIRONMENTIMPACT ASSESMENT OBJECT 2.0 GENERAL SITUATIONOF THE PROJECT 2.1 PROJECTPURPOSE 2.2 PROJECTCOMPOSITION 2.3 CONSTRUCTIONSCALE AND STANDARDOF THE PROJECT 2.4 MAJOR WORKS 2.5 INVESTMENTAND RAISINGFUNDS 2.6 IMPLEMENTATIONPLAN 3.0 GENERAL SITUATION OF ENVIRONMENT 3.1 METEOROLOGY 3.2 LANDFORMAND GEOMORPHOLOGY 3.3 ECONOMY 3.4 TRANSPORT 3.5 HISTORYAND CULTURE 4.0 CURRENT SITUATION OF ENVIRONMENT QUALITY 4.1 CURRENTSITUATION OF ATMOSPHERIC ENVIRONMENT QUALITY 4.2 CURRENTSITUATION OF WATER ENVIRONMENT QUALITY 4.3 CURRENTSITUATION OF ACOUSTICENVIRONMENT 4.4 CURRENTSITUATION OF ECOLOGICAL ENVIRONMENT QUALITY 5.0 ENVIRONMENT IMPACT OF THE PROJECT AND POLLUTION PREVENTION AND MITIGATION MEASURES 5.1 ENVIRONMENTIMPACT TYPES 5.2 SOCIAL IMPACT 5.3 -

Debt Analysis of Prefecture-Level City Lgs in Zhejiang and Jiangsu Provinces
Local Government China Debt analysis of prefecture-level city LGs in Zhejiang and Jiangsu provinces Content Summary Summary .......................................... 1 ▪ Situated in the lower reaches of the Yangtze River and bordering the municipality of Shanghai, both Zhejiang province (AA-/Stable) and Jiangsu province The variance of debt ratios among (A+/Stable) are coastal provinces in eastern China (AA/Stable) and adjacent to Zhejiang's LGs is smaller and overall each other. They are major economic provinces in China with vigorous economic debt levels are lower than their peers development and economic strength in the front rank of the country. They have the in Jiangsu province ........................... 3 highest and second-highest gross domestic production (GDP) per capita among Hidden debt makes up the bulk of Chinese provincial-level regions (excluding direct-administered municipalities). broad debt in Jiangsu prefecture-level LGs and their hidden debt burden is ▪ According to our analysis of government debt (including direct debt and hidden generally higher than LGs in Zhejiang debt) of 11 prefecture-level local governments (LGs) in Zhejiang province and 13 ......................................................... 4 prefecture-level LGs in Jiangsu province; we believe these prefecture-level LGs as a whole have a strong ability to support debt repayment. This is backed by their Debt growth varies more, and we see advanced economies and solid budgetary revenues. Our calculations show that higher growth in debt-to-GDP ratio debt ratios of most of the prefecture-level LGs in the two provinces were lower than among prefecture-level LGs in the nation-wide local governments' average in 2019. Zhejiang than Jiangsu .....................