Hurricane Katrina, Children, and Pediatric Heroes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Songs from the Granite Hills
THE LIBRARY OF THE UNIVERSITY OF CALIFORNIA LOS ANGELES SONGS FROM THE GRANITE HILLS BY CLARK B. COCHRANE BOSTON THE GORHAM PRESS MCMXVIII COPYRIGHT, 1918, BY CLARK B. COCHRANE All Rights Reserved Made in the United States of America The Gorham Press, Boston, U. S. A. fs CONTENTS PAGE Love Lives Forever: A Medley .... 7 If? 35 On a Picture Set in Gold ...... 36 The Days of Long Ago 40 A Battle Call. 1862 46 Fredericksburg 48 Noon by Lake Sunapee 50 The Builders 52 The Plaint of the Pessimist 54 The Star of the Optimist 57 The Voice of Love Divine 59 A Tryst 62 New England 63 Our Angels 65 Crosses 67 For Don, My Dog 68 A Farewell to Joe English 70 Anabel 75 To Susie 78 The Light Men Use 79 A Reverie 81 The Sweetest Word 83 A Plea for a Heart 84 3 626070 4 Contents PAGE Sonnets 86 The Tryst of the Pilot 95 The White Ticket 97 On the Shore 99 A Plea for Love . 101 SONGS FROM THE GRANITE HILLS LOVE LIVES FOREVER: A MEDLEY Prelude JOVE and Juno, Oberon, From the fields of time have fled; All the gods but Love are gone Realmless, hopeless, listless, dead! When Jehovah claimed His own And the old gods fled away, Love was kindred to His throne And the Master bade him stay. Thor and Odin, Neptune, Pan Not one could the test endure; Love, the dreamer, lives for man Only that his heart was pure. Slaves may rise at Freedom's call, Freemen bound as slaves may be, Empires wax and kingdoms fall, Deserts smile with blade and tree Seas and rivers may dry up, Cities stand where now are seas, Still this god will dine and sup In their cots and palaces! He shall touch the hearts of men With the fire that burns on high, Which if quenched will burn again In the soul that cannot die. -

Hydroski-Foil" Air
Amazing "Hydroski-Foil" Air Boat...it's fast, fast, fast! • When the countdown reaches zero for face diving or air seepage along wings ski. Result: exceptional versatility and this hydroski-foil air boat, one push un- which results in loss of hydrofoil lift. performance. leashes a 3/4 hp booster engine which Remember, a hydrofoil (similar to an Operating a hydroski-foil air boat suc- jumps the boat up on damp-air with airplane wing) produces tremendous lift cessfully can be done most easily by the vapor-trail speeds! The design proved "A- as it speeds along submerged in water. following means: First, adjust forward O.K." over half-foot waves, on land using This is accomplished by a partial separa- ski-foils anywhere, between 14° to 16° wheel attachment, across ice using runner tion of water over the top of the curved angle of attack on water and the stern attachments—with tether line, free- hydrofoil. With water pressure under- ski-foil between 3° and 6°. Second, pivot running, and radio control as well. Most neath the "wing" and a partial vacuum the stern ski-foil straight ahead as you people who have witnessed "damp-air above, tremendous lift is achieved. would a rudder. Clip your tether line flights" of the ski-foil air boat were quite All hydrofoils require some means of leads on the stern and forward strut and inquisitive. adjustment for regulating their running start engine. Hold boat slightly in the Several years ago an article I read about depth in rough and in smooth water. -

Me Jane Tour Playbill-Final
The John F. Kennedy Center for the Performing Arts DAVID M. RUBENSTEIN, Chairman DEBORAH F. RUTTER, President Kennedy Center Theater for Young Audiences on Tour presents A Kennedy Center Commission Based on the book Me…Jane by Patrick McDonnell Adapted and Written by Patrick McDonnell, Andy Mitton, and Aaron Posner Music and Lyrics by Andy Mitton Co-Arranged by William Yanesh Choreographed by Christopher D’Amboise Music Direction by William Yanesh Directed by Aaron Posner With Shinah Brashears, Liz Filios, Phoebe Gonzalez, Harrison Smith, and Michael Mainwaring Scenic Designer Lighting Designer Costume Designer Projection Designer Paige Hathaway Andrew Cissna Helen Q Huang Olivia Sebesky Sound Designer Properties Artisan Dramaturg Casting Director Justin Schmitz Kasey Hendricks Erin Weaver Michelle Kozlak Executive Producer General Manager Executive Producer Mario Rossero Harry Poster David Kilpatrick Bank of America is the Presenting Sponsor of Performances for Young Audiences. Additional support for Performances for Young Audiences is provided by the A. James & Alice B. Clark Foundation; The Morris and Gwendolyn Cafritz Foundation; Paul M. Angell Family Foundation; Anne and Chris Reyes; and the U.S. Department of Education. Funding for Access and Accommodation Programs at the Kennedy Center is provided by the U.S. Department of Education. Major support for educational programs at the Kennedy Center is provided by David M. Rubenstein through the Rubenstein Arts Access Program. The contents of this document do not necessarily represent the policy of the U.S. Department of Education, and you should not assume endorsement by the Federal Government. " Patrons are requested to turn off cell phones and other electronic devices during performances. -

Notable Australians Historical Figures Portrayed on Australian Banknotes
NOTABLE AUSTRALIANS HISTORICAL FIGURES PORTRAYED ON AUSTRALIAN BANKNOTES X X I NOTABLE AUSTRALIANS HISTORICAL FIGURES PORTRAYED ON AUSTRALIAN BANKNOTES Aboriginal and Torres Strait Islander readers are respectfully advised that this book includes the names and images of people who are now deceased. Cover: Detail from Caroline Chisholm's portrait by Angelo Collen Hayter, oil on canvas, 1852, Dixson Galleries, State Library of NSW (DG 459). Notable Australians Historical Figures Portrayed on Australian Banknotes © Reserve Bank of Australia 2016 E-book ISBN 978-0-6480470-0-1 Compiled by: John Murphy Designed by: Rachel Williams Edited by: Russell Thomson and Katherine Fitzpatrick For enquiries, contact the Reserve Bank of Australia Museum, 65 Martin Place, Sydney NSW 2000 <museum.rba.gov.au> CONTENTS Introduction VI Portraits from the present series Portraits from pre-decimal of banknotes banknotes Banjo Paterson (1993: $10) 1 Matthew Flinders (1954: 10 shillings) 45 Dame Mary Gilmore (1993: $10) 3 Charles Sturt (1953: £1) 47 Mary Reibey (1994: $20) 5 Hamilton Hume (1953: £1) 49 The Reverend John Flynn (1994: $20) 7 Sir John Franklin (1954: £5) 51 David Unaipon (1995: $50) 9 Arthur Phillip (1954: £10) 53 Edith Cowan (1995: $50) 11 James Cook (1923: £1) 55 Dame Nellie Melba (1996: $100) 13 Sir John Monash (1996: $100) 15 Portraits of monarchs on Australian banknotes Portraits from the centenary Queen Elizabeth II of Federation banknote (2016: $5; 1992: $5; 1966: $1; 1953: £1) 57 Sir Henry Parkes (2001: $5) 17 King George VI Catherine Helen -

References Cited, Katrina Commoditized
References Cited Airboat Adventures. (n.d.). Hurricane Katrina Tours. Retrieved September 3, 2009 from http://www.airboatadventures.com/hurricane_katrina_tour.htm Alpert, B. (2005, December 3). Disaster tours urged for Congress. The Times-Picayune (New Orleans, LA). Retrieved October 16, 2009 from NewsBank database. Alpert, B. (2006a, January 11). In Congress, vast majority yet to see ruins. The Times-Picayune (New Orleans, LA). Retrieved November 8, 2009 from NewsBank database. Alpert, B. (2006b, March 2). Bipartisan tour brings 32 congressmen to N.O. The Times-Picayune (New Orleans, LA). Retrieved November 8, 2009 from NewsBank database. Alpert, B. (2006c, March 9). 3 more senators coming to see destruction. The Times-Picayune (New Orleans, LA). Retrieved November 8, 2009 from NewsBank database. Appadurai. A. (1986). Introduction: Commodities and the politics of value. In A. Appadurai (Ed.), The social life of things: Commodities in cultural perspective (pp. 6-16). Cambridge, England: Cambridge University Press. Bertrand, G. (2006, January 11). Tours get the message out. The Times-Picayune (New Orleans, LA). Retrieved November 15, 2009 from NewsBank database. Bohannan, P. (1959). The Impact of money on an African subsistence economy. Journal of Economic History, 19, 491-503. Celebration Tours. (n.d.). City of New Orleans and Katrina Recovery Tour. Retrieved November 16, 2009 from http://www.celebrationtoursllc.com/citytour.html DeBerry, J. (2006, May 21). Leave some misery for posterity. The Times-Picayune (New Orleans, LA). Retrieved November 15, 2009 from NewsBank database. Donze, F. (2005, November 15). Lower 9th Ward to open Dec. 1. The Times-Picayune (New Orleans, LA). Retrieved October 16, 2009 from NewsBank database. -

Ohio Shanghai India's Temples
fall/winter 2019 — $3.95 Ohio Fripp Island Michigan Carnival Mardi Gras New Jersey Panama City Florida India’s Temples Southwestern Ontario Shanghai 1 - CROSSINGS find your story here S ome vacations become part of us. The beauty and Shop for one-of-a-kind Join us in January for the 6th Annual Comfort Food Cruise. experiences come home with us and beckon us back. Ohio’s holiday gifts during the The self-guided Cruise provides a tasty tour of the Hocking Hills Hocking Hills in winter is such a place. Breathtaking scenery, 5th Annual Hocking with more than a dozen locally owned eateries offering up their outdoor adventures, prehistoric caves, frozen waterfalls, Hills Holiday Treasure classic comfort specialties. and cozy cabins, take root and call you back again and Hunt and enter to win again. Bring your sense of adventure and your heart to the one of more than 25 To get your free visitor’s guide and find out more about Hocking Hills and you’ll count the days until you can return. prizes and a Grand the Comfort Food Cruise and Treasure Hunt call or click: Explore the Hocking Hills, Ohio’s Natural Crown Jewels. Prize Getaway for 4. 1-800-Hocking | ExploreHockingHills.com find your story here S ome vacations become part of us. The beauty and Shop for one-of-a-kind Join us in January for the 6th Annual Comfort Food Cruise. experiences come home with us and beckon us back. Ohio’s holiday gifts during the The self-guided Cruise provides a tasty tour of the Hocking Hills Hocking Hills in winter is such a place. -

The Titles Below Are Being Released for Record Store
THE TITLES BELOW ARE BEING RELEASED FOR RECORD STORE DAY (v.2.2 updated 4-01) ARTISTA TITOLO FORMATO LABEL LA DONNA IL SOGNO & IL GRANDE ¢ 883 2LP PICTURE WARNER INCUBO ¢ ACID MOTHERS TEMPLE NAM MYO HO REN GE KYO LP SPACE AGE ¢ AL GREEN GREEN IS BLUES LP FAT POSSUM ¢ ALESSANDRO ALESSANDRONI RITMO DELL’INDUSTRIA N°2 LP BTF ¢ ALFREDO LINARES Y SU SONORA YO TRAIGO BOOGALOO LP VAMPISOUL LIVE FROM THE APOLLO THEATRE ¢ ALICE COOPER 2LP WARNER GLASGOW, FEB 19, 1982 SOUNDS LIKE A MELODY (GRANT & KELLY ¢ ALPHAVILLE REMIX BY BLANK & JONES X GOLD & 12" WARNER LLOYD) HERITAGE II:DEMOS ALTERNATIVE TAKES ¢ AMERICA LP WARNER 1971-1976 ¢ ANDREA SENATORE HÉRITAGE LP ONDE / ITER-RESEARCH ¢ ANDREW GOLD SOMETHING NEW: UNREALISED GOLD LP WARNER ¢ ANNIHILATOR TRIPLE THREAT UNPLUGGED LP WARNER ¢ ANOUSHKA SHANKAR LOVE LETTERS LP UNIVERSAL ¢ ARCHERS OF LOAF RALEIGH DAYS 7" MERGE ¢ ARTICOLO 31 LA RICONQUISTA DEL FORUM 2LP COLORATO BMG ¢ ASHA PUTHLI ASHA PUTHLI LP MR. BONGO ¢ AWESOME DRE YOU CAN'T HOLD ME BACK LP BLOCGLOBAL ¢ BAIN REMIXES 12'' PICTURE CIMBARECORD ¢ BAND OF PAIN A CLOCKWORK ORANGE LP DIRTER ¢ BARDO POND ON THE ELLIPSE LP FIRE ¢ BARRY DRANSFIELD BARRY DRANSFIELD LP GLASS MODERN ¢ BARRY HAY & JB MEIJERS THE ARTONE SESSION 10" MUSIC ON VINYL ¢ BASTILLE ALL THIS BAD BLOOD 2LP UNIVERSAL ¢ BATMOBILE BIG BAT A GO-GO 7'' COLORATO MUSIC ON VINYL I MISTICI DELL'OCCIDENTE (10° ¢ BAUSTELLE LP WARNER ANNIVERSARIO) ¢ BECK UNEVENTFUL DAYS (ST. VINCENT REMIX) 7" UNIVERSAL GRANDPAW WOULD (25TH ANNIVERSARY ¢ BEN LEE 2LP COLORATO LIGHTNING ROD DELUXE) ¢ BEN WATT WITH ROBERT WYATT SUMMER INTO WINTER 12'' CHERRY RED ¢ BERT JANSCH LIVE IN ITALY LP EARTH ¢ BIFFY CLYRO MODERNS 7'' COLORATO WARNER ¢ BLACK ARK PLAYERS GUIDANCE 12'' PICTURE VP GOOD TO GO ¢ BLACK LIPS FEAT. -

L the Charlatans UK the Charlatans UK Vs. the Chemical Brothers
These titles will be released on the dates stated below at physical record stores in the US. The RSD website does NOT sell them. Key: E = Exclusive Release L = Limited Run / Regional Focus Release F = RSD First Release THESE RELEASES WILL BE AVAILABLE AUGUST 29TH ARTIST TITLE LABEL FORMAT QTY Sounds Like A Melody (Grant & Kelly E Alphaville Rhino Atlantic 12" Vinyl 3500 Remix by Blank & Jones x Gold & Lloyd) F America Heritage II: Demos Omnivore RecordingsLP 1700 E And Also The Trees And Also The Trees Terror Vision Records2 x LP 2000 E Archers of Loaf "Raleigh Days"/"Street Fighting Man" Merge Records 7" Vinyl 1200 L August Burns Red Bones Fearless 7" Vinyl 1000 F Buju Banton Trust & Steppa Roc Nation 10" Vinyl 2500 E Bastille All This Bad Blood Capitol 2 x LP 1500 E Black Keys Let's Rock (45 RPM Edition) Nonesuch 2 x LP 5000 They's A Person Of The World (featuring L Black Lips Fire Records 7" Vinyl 750 Kesha) F Black Crowes Lions eOne Music 2 x LP 3000 F Tommy Bolin Tommy Bolin Lives! Friday Music EP 1000 F Bone Thugs-N-Harmony Creepin' On Ah Come Up Ruthless RecordsLP 3000 E David Bowie ChangesNowBowie Parlophone LP E David Bowie ChangesNowBowie Parlophone CD E David Bowie I’m Only Dancing (The Soul Tour 74) Parlophone 2 x LP E David Bowie I’m Only Dancing (The Soul Tour 74) Parlophone CD E Marion Brown Porto Novo ORG Music LP 1500 F Nicole Bus Live in NYC Roc Nation LP 2500 E Canned Heat/John Lee Hooker Hooker 'N Heat Culture Factory2 x LP 2000 F Ron Carter Foursight: Stockholm IN+OUT Records2 x LP 650 F Ted Cassidy The Lurch Jackpot Records7" Vinyl 1000 The Charlatans UK vs. -
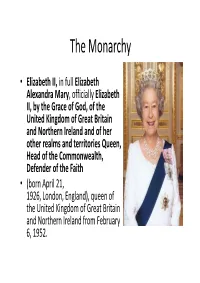
The Monarchy
The Monarchy • Elizabeth II, in full Elizabeth Alexandra Mary , officially Elizabeth II, by the Grace of God, of the United Kingdom of Great Britain and Northern Ireland and of her other realms and territories Queen, Head of the Commonwealth, Defender of the Faith • (born April 21, 1926, London, England), queen of the United Kingdom of Great Britain and Northern Ireland from February 6, 1952. The Role of the Monarchy • Monarchy is the oldest form of government in the United Kingdom. • In a monarchy, a king or queen is Head of State . The British monarchy is known as a constitutional monarchy . This means that, while The Sovereign is Head of State, the ability to make and pass legislation resides with an elected Parliament. • Although the British Sovereign no longer has a political or executive role, he or she continues to play an important part in the life of the nation. • As Head of State, The Monarch undertakes constitutional and representational duties which have developed over one thousand years of history. In addition to these State duties, The Monarch has a less formal role as 'Head of Nation'. The Sovereign acts as a focus for national identity, unity and pride; gives a sense of stability and continuity; officially recognises success and excellence; and supports the ideal of voluntary service. • In all these roles The Sovereign is supported by members of their immediate family. http://www.royal.gov.uk/MonarchUK/HowtheMonarchyworks/HowtheMonarchyworks.aspx Queen and Government • As Head of State The Queen has to remain strictly neutral with respect to political matters, unable to vote or stand for election. -

Meet the Krash Family
Meet the Krash Family “Get in the van, kids! We’re running late!” The Krash family of four is headed to Grandpa Krash’s 90th birthday party, and they’re off to a hectic start. Father Jimmy, 43, is at the wheel, impatient because his two kids (JJ, 17 and Ramona, 7) were slow to get ready to leave and now they’re running behind. On this late November afternoon, they’re traveling down Big River Road - a rural highway - at approximately 65 mph in a minivan, with temperatures dipping down into the 30’s. “Jimmy, slow down – you’re going too fast for these curvy country roads!” Jimmy’s wife Jane is nervous because Jimmy is hurrying more than she thinks is safe. Suddenly, just as they reach a blind curve, a deer darts out into the road causing him to jerk the wheel. Tires screeching on the asphalt, the minivan loses control and rolls down a four-foot embankment, flipping over and landing on its top, with the Krash family still inside. A passing motorist approaches a few minutes later and notices the fresh disturbance in the guardrail. Horrified at the possibility of a recent accident, she stops to investigate and notices the overturned minivan. She yells to the family that she’s getting help and rushes to call 911 for an ambulance, describing the scene as best she can. Folsom County Fire and EMS crews arrive within nine minutes of dispatch, and identify our four patients who are still inside the vehicle. A teenage boy appears to be trapped in the third row of the minivan, but the other three patients are removed while crews work to stabilize the vehicle. -

FWS Hurricane Katrina Fund
Service Works to Save Lives, Provide Aid in Katrina’s Wake Approximately 150 Fish and Wildlife Service employees are assisting other government agencies and relief organizations in the massive Hurricane Katrina recovery effort in southeast Louisiana and along the Mississippi Gulf Coast. In the days since Katrina’s landfall, FWS employees have cleared miles of roads and emergency corridors to speed relief aid to citizens, operated boat rescue missions in New Orleans, supported search and rescue efforts throughout the impacted area, and provided food and lodging for emergency personnel and relief volunteers. “We’re continuing to focus on community assistance activities and support the Federal Emergency Management Agency’s overall recovery effort,” said Matt Hogan, Acting Director of the Service. “Service personnel were in the area within hours of the storm coming ashore and we’ll help as long as we’re needed. Our people live here too.” All Service personnel have been accounted for, although more than 20 employees have lost their homes or been displaced. Preliminary estimates suggest the damage to FWS refuges and facilities in the area affected by Hurricane Katrina now exceeds $90 million, although not all stations have been assessed. Sixteen National Wildlife Refuges and other assorted Service hatcheries, field stations and offices across the region remain closed due to the damage they sustained from the hurricane. The FWS response to the disaster has been rapid, aggressive, and varied. Earlier this week, FWS crews opened roads to Louisiana Heart Hospital and now are providing 200 meals a day to that facility, as well as to 100 Marines assigned to the area. -

2020-RSD-Drops-List.Pdf
THESE RELEASES WILL BE AVAILABLE AUGUST 29TH DROP ARTIST TITLE FORMAT QTY August Marie-Mai Elle et Moi 12” Vinyl 400 August The Trews No Time For Later (Limited Edition) 2XLP 750 August Ron Sexsmith Hermitage (RSD20EX) 12” Vinyl 250 August Milk & Bone Dive 12” Vinyl 250 August You Say Party XXXX (10th Anniversary Limited Edition) 12” LP 200 August Teenage Head Drive In 7” Single 500 August The Neil Swainson Quintet 49th Parallel 500 12” Double August Rascalz Cash Crop 1000 Vinyl 12” Double August Offenbach En Fusion-40th anniversary 500 Vinyl August Ace Frehley Trouble Walkin' LP Penderecki/Don Cherry & The New Eternal August Actions LP 1500 Rhythm August Al Green Green Is Blues Sounds Like A Melody (Grant & Kelly Remix August Alphaville LP by Blank & Jones x Gold & Lloyd) Heritage II: Demos/Alternate Takes 1971- August America LP 1976 August Andrew Gold Something New: Unreleased Gold LP LP RSD August Anoushka Shankar Love Letters EXCL 7" RSD August August Burns Red Bones EXCL August Bastille All This Bad Blood RSD EXCL August Biffy Clyro Moderns LP LP RSD August Billie Eilish Live at Third Man EX 12"RSD August Bob Markley Redemption Song EXCL August Bone Thugs N Harmony Creepin on Ah Come Up RSD EXCL LP RSD August Brian Eno SOUNDTRACK RAMS EXC August Brittany Howard Live at Sound Emporium LP RSD LP RSD August Buffy Sainte-Marie Illuminations EXCL 10" RSD August Buju Banton Trust & Steppa EXCL 7"RSD August Cat Stevens But I Might Die Tonight EXCL August Charli XCX Vroom Vroom EP LP LP RSD August Charlie Parker Jazz at Midnight