Spinal Muscular Atrophy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
Spinal Muscular Atrophy
Spinal Muscular Atrophy U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES National Institutes of Health Spinal Muscular Atrophy What is spinal muscular atrophy? pinal muscular atrophy (SMA) is a group Sof hereditary diseases that progressively destroys motor neurons—nerve cells in the brain stem and spinal cord that control essential skeletal muscle activity such as speaking, walking, breathing, and swallowing, leading to muscle weakness and atrophy. Motor neurons control movement in the arms, legs, chest, face, throat, and tongue. When there are disruptions in the signals between motor neurons and muscles, the muscles gradually weaken, begin wasting away and develop twitching (called fasciculations). What causes SMA? he most common form of SMA is caused by Tdefects in both copies of the survival motor neuron 1 gene (SMN1) on chromosome 5q. This gene produces the survival motor neuron (SMN) protein which maintains the health and normal function of motor neurons. Individuals with SMA have insufficient levels of the SMN protein, which leads to loss of motor neurons in the spinal cord, producing weakness and wasting of the skeletal muscles. This weakness is often more severe in the trunk and upper leg and arm muscles than in muscles of the hands and feet. 1 There are many types of spinal muscular atrophy that are caused by changes in the same genes. Less common forms of SMA are caused by mutations in other genes including the VAPB gene located on chromosome 20, the DYNC1H1 gene on chromosome 14, the BICD2 gene on chromosome 9, and the UBA1 gene on the X chromosome. The types differ in age of onset and severity of muscle weakness; however, there is overlap between the types. -

A Novel De Novo 20Q13.32&Ndash;Q13.33
Journal of Human Genetics (2015) 60, 313–317 & 2015 The Japan Society of Human Genetics All rights reserved 1434-5161/15 www.nature.com/jhg ORIGINAL ARTICLE Anovelde novo 20q13.32–q13.33 deletion in a 2-year-old child with poor growth, feeding difficulties and low bone mass Meena Balasubramanian1, Edward Atack2, Kath Smith2 and Michael James Parker1 Interstitial deletions of the long arm of chromosome 20 are rarely reported in the literature. We report a 2-year-old child with a 2.6 Mb deletion of 20q13.32–q13.33, detected by microarray-based comparative genomic hybridization, who presented with poor growth, feeding difficulties, abnormal subcutaneous fat distribution with the lack of adipose tissue on clinical examination, facial dysmorphism and low bone mass. This report adds to rare publications describing constitutional aberrations of chromosome 20q, and adds further evidence to the fact that deletion of the GNAS complex may not always be associated with an Albright’s hereditary osteodystrophy phenotype as described previously. Journal of Human Genetics (2015) 60, 313–317; doi:10.1038/jhg.2015.22; published online 12 March 2015 INTRODUCTION resuscitation immediately after birth and Apgar scores were 9 and 9 at 1 and Reports of isolated subtelomeric deletions of the long arm of 10 min, respectively, of age. Birth parameters were: weight ~ 1.56 kg (0.4th–2nd chromosome 20 are rare, but a few cases have been reported in the centile), length ~ 40 cm (o0.4th centile) and head circumference ~ 28.2 cm o fi literature over the past 30 years.1–13 Traylor et al.12 provided an ( 0.4th centile). -

The DNA Sequence and Comparative Analysis of Human Chromosome 20
articles The DNA sequence and comparative analysis of human chromosome 20 P. Deloukas, L. H. Matthews, J. Ashurst, J. Burton, J. G. R. Gilbert, M. Jones, G. Stavrides, J. P. Almeida, A. K. Babbage, C. L. Bagguley, J. Bailey, K. F. Barlow, K. N. Bates, L. M. Beard, D. M. Beare, O. P. Beasley, C. P. Bird, S. E. Blakey, A. M. Bridgeman, A. J. Brown, D. Buck, W. Burrill, A. P. Butler, C. Carder, N. P. Carter, J. C. Chapman, M. Clamp, G. Clark, L. N. Clark, S. Y. Clark, C. M. Clee, S. Clegg, V. E. Cobley, R. E. Collier, R. Connor, N. R. Corby, A. Coulson, G. J. Coville, R. Deadman, P. Dhami, M. Dunn, A. G. Ellington, J. A. Frankland, A. Fraser, L. French, P. Garner, D. V. Grafham, C. Grif®ths, M. N. D. Grif®ths, R. Gwilliam, R. E. Hall, S. Hammond, J. L. Harley, P. D. Heath, S. Ho, J. L. Holden, P. J. Howden, E. Huckle, A. R. Hunt, S. E. Hunt, K. Jekosch, C. M. Johnson, D. Johnson, M. P. Kay, A. M. Kimberley, A. King, A. Knights, G. K. Laird, S. Lawlor, M. H. Lehvaslaiho, M. Leversha, C. Lloyd, D. M. Lloyd, J. D. Lovell, V. L. Marsh, S. L. Martin, L. J. McConnachie, K. McLay, A. A. McMurray, S. Milne, D. Mistry, M. J. F. Moore, J. C. Mullikin, T. Nickerson, K. Oliver, A. Parker, R. Patel, T. A. V. Pearce, A. I. Peck, B. J. C. T. Phillimore, S. R. Prathalingam, R. W. Plumb, H. Ramsay, C. M. -

The Main Molecular Bases of Amyotrophic Lateral Sclerosis: an Integrating Review Leonardo Ricardo Pizani1, Patricia Ucelli Simioni1,2
REVIEW ARTICLE The Main Molecular Bases of Amyotrophic Lateral Sclerosis: An Integrating Review Leonardo Ricardo Pizani1, Patricia Ucelli Simioni1,2 1Department of Biomedical Science, Faculty of Americana, FAM, Americana, SP, Brazil, 2Institute of Biosciences, Universidade Estadual Paulista, UNESP, Rio Claro, SP, Brazil ABSTRACT Amyotrophic lateral sclerosis (ALS) is a progressive and fatal neurodegenerative disease that affects the lower and upper motor neurons. Its etiology is unknown, despite several studies that point to risk factors and genetic for the disease. It does not have a definitive treatment and the diagnosis, most of the time, is time consuming and demands varied criteria for adequate definition and classification. In the search for new treatments, gene therapy with gene insertion aims to reduce the impact of ALS on the patient. The study of molecular basis as the root cause of the disease becomes necessary to advance the discovery of effective treatment and a rapid diagnosis, aiming at improving the quality of life of the ALS patients. Therefore, the present work had the objective to bring an update of the literature on ALS, as well as to describe the main molecular bases involved in the causative/ causative process of this disease. Key words: Amyotrophic lateral sclerosis, motor neurons, nervous system diseases BACKGROUND World Federation of Neurology, the diagnosis should be made through clinical examination, electromyography, assessment myotrophic lateral sclerosis (ALS) is a neurodegenerative of neurogenic abnormalities and progression of the clinical [3] disease of the lower motor nervous system (LMNS) and picture, and differential diagnosis. According to the upper motor nervous System(UMNS), which affects diagnosis and degree of degeneration of motor neurons, the A diagnosis can be subclassified as: Definitive ALS, probable the cerebral cortex, brain stem, and spinal cord, being classified according to the initially compromised neurological region. -

Chromatin Conformation Links Distal Target Genes to CKD Loci
BASIC RESEARCH www.jasn.org Chromatin Conformation Links Distal Target Genes to CKD Loci Maarten M. Brandt,1 Claartje A. Meddens,2,3 Laura Louzao-Martinez,4 Noortje A.M. van den Dungen,5,6 Nico R. Lansu,2,3,6 Edward E.S. Nieuwenhuis,2 Dirk J. Duncker,1 Marianne C. Verhaar,4 Jaap A. Joles,4 Michal Mokry,2,3,6 and Caroline Cheng1,4 1Experimental Cardiology, Department of Cardiology, Thoraxcenter Erasmus University Medical Center, Rotterdam, The Netherlands; and 2Department of Pediatrics, Wilhelmina Children’s Hospital, 3Regenerative Medicine Center Utrecht, Department of Pediatrics, 4Department of Nephrology and Hypertension, Division of Internal Medicine and Dermatology, 5Department of Cardiology, Division Heart and Lungs, and 6Epigenomics Facility, Department of Cardiology, University Medical Center Utrecht, Utrecht, The Netherlands ABSTRACT Genome-wide association studies (GWASs) have identified many genetic risk factors for CKD. However, linking common variants to genes that are causal for CKD etiology remains challenging. By adapting self-transcribing active regulatory region sequencing, we evaluated the effect of genetic variation on DNA regulatory elements (DREs). Variants in linkage with the CKD-associated single-nucleotide polymorphism rs11959928 were shown to affect DRE function, illustrating that genes regulated by DREs colocalizing with CKD-associated variation can be dysregulated and therefore, considered as CKD candidate genes. To identify target genes of these DREs, we used circular chro- mosome conformation capture (4C) sequencing on glomerular endothelial cells and renal tubular epithelial cells. Our 4C analyses revealed interactions of CKD-associated susceptibility regions with the transcriptional start sites of 304 target genes. Overlap with multiple databases confirmed that many of these target genes are involved in kidney homeostasis. -

Expanding the Phenotypes of the Pro56ser Vapb Mutation: Proximal Sma with Dysautonomia
ABSTRACT: The phenotype of 16 members of a family affected by a late-onset, dominant, progressive, motor and autonomic disorder is de- scribed. The VAPB (Pro56Ser) mutation was detected in Brazilian families with different phenotypes of motor neuron disorders. In this family, proximal and axial muscle weakness and atrophy, associated with abdominal protru- sion, defined the motor phenotype. Death occurred in 10–15 years due to respiratory insufficiency. Tone and tendon reflexes were decreased and a distal tremor was common. Sensation was preserved. Autonomic abnormal- ities were also present, including choking, chronic intestinal constipation, sexual dysfunction, and sudomotor abnormalities, and on nerve morphology there was involvement of unmyelinated fibers. Electromyography disclosed ongoing denervation and reinnervation. Isolated dysfunction of motor and autonomic neurons is unusual among the spinal muscular atrophies. On this basis, this condition seems to represent a new category of disease. Muscle Nerve 34: 731–739, 2006 EXPANDING THE PHENOTYPES OF THE PRO56SER VAPB MUTATION: PROXIMAL SMA WITH DYSAUTONOMIA VANESSA D. MARQUES, MD,1 AMILTON A. BARREIRA, MD, PhD,1 MARY B. DAVIS, PhD,2 PATRICK M. ABOU-SLEIMAN, PhD,2 WILSON A. SILVA, Jr., PhD,3,4 MARCO A. ZAGO, MD, PhD,3 CLAUDIA SOBREIRA, MD, PhD,1 VALE´ RIA FAZAN, MD, PhD,5 and WILSON MARQUES, Jr., MD, PhD1 1 Department of Neurology, School of Medicine of Ribeira˜o Preto, University of Sa˜o Paulo, Av. Bandeirantes, 3900 Ribeira˜o Preto, Sa˜o Paulo, 14049-900, Brazil 2 Neurogenetics Unit, -

Widespread Aggregation of Mutant VAPB Associated with ALS Does Not
Qiu et al. Molecular Neurodegeneration 2013, 8:1 http://www.molecularneurodegeneration.com/content/8/1/1 RESEARCH ARTICLE Open Access Widespread aggregation of mutant VAPB associated with ALS does not cause motor neuron degeneration or modulate mutant SOD1 aggregation and toxicity in mice Linghua Qiu1*, Tao Qiao1, Melissa Beers1,2, Weijia Tan1, Hongyan Wang1, Bin Yang1,3 and Zuoshang Xu1,4,5* Abstract Background: A proline-to-serine substitution at position-56 (P56S) of vesicle-associated membrane protein-associated protein B (VAPB) causes a form of dominantly inherited motor neuron disease (MND), including typical and atypical amyotrophic lateral sclerosis (ALS) and a mild late-onset spinal muscular atrophy (SMA). VAPB is an integral endoplasmic reticulum (ER) protein and has been implicated in various cellular processes, including ER stress, the unfolded protein response (UPR) and Ca2+ homeostasis. However, it is unclear how the P56S mutation leads to neurodegeneration and muscle atrophy in patients. The formation of abnormal VAPB-positive inclusions by mutant VAPB suggests a possible toxic gain of function as an underlying mechanism. Furthermore, the amount of VAPB protein is reported to be reduced in sporadic ALS patients and mutant SOD1G93A mice, leading to the hypothesis that wild type VAPB plays a role in the pathogenesis of ALS without VAPB mutations. Results: To investigate the pathogenic mechanism in vivo, we generated human wild type (wtVAPB) and mutant VAPB (muVAPB) transgenic mice that expressed the transgenes broadly in the CNS. We observed robust VAPB-positive aggregates in the spinal cord of muVAPB transgenic mice. However, we failed to find an impairment of motor function and motor neuron degeneration. -

VAPB ER-Aggregates, a Possible New Biomarker in ALS Pathology
cells Article VAPB ER-Aggregates, A Possible New Biomarker in ALS Pathology Maria Piera L Cadoni 1 , Maria Luigia Biggio 1, Giannina Arru 1, Giannina Secchi 1, Nicola Orrù 2, Maria Grazia Clemente 1, GianPietro Sechi 1 , Alfred Yamoah 3, Priyanka Tripathi 3, Sandro Orrù 2, Roberto Manetti 1 and Grazia Galleri 1,* 1 Department of Medical Surgical and Experimental Sciences, University of Sassari, Viale San Pietro 8, 07100 Sassari, Italy; [email protected] (M.P.L.C.); [email protected] (M.L.B.); [email protected] (G.A.); [email protected] (G.S.); [email protected] (M.G.C.); [email protected] (G.P.S.); [email protected] (R.M.) 2 Department of Medical Sciences and Public Health, University of Cagliari, S. P. Monserrato—Sestu km 0,700, 09042 Monserrato, Italy; [email protected] (N.O.); [email protected] (S.O.) 3 Institute of Neuropathology, RWTH Aachen University Medical School, Pauwelsstr. 30, 52074 Aachen, Germany; [email protected] (A.Y.); [email protected] (P.T.) * Correspondence: [email protected]; Tel.: +39-079-228419 Received: 25 November 2019; Accepted: 30 December 2019; Published: 9 January 2020 Abstract: A point mutation (P56S) in the gene-encoding vesicle-associated membrane-protein-associated protein B (VAPB) leads to an autosomal-dominant form of amyotrophic lateral sclerosis (ALS), classified as ALS-8. The mutant VAPB is characterized by ER-associated aggregates that lead to a complete reorganization of ER structures. Growing evidences suggest VAPB involvement in ALS pathomechanisms. In fact, numerous studies demonstrated VAPB alteration also in sporadic ALS (sALS) and showed the presence of its aggregates when others ALS-related gene are mutant. -

Host Vesicle Fusion Protein VAPB Contributes to the Nuclear Egress Stage of Herpes Simplex Virus Type-1 (HSV-1) Replication
cells Article Host Vesicle Fusion Protein VAPB Contributes to the Nuclear Egress Stage of Herpes Simplex Virus Type-1 (HSV-1) Replication Natalia Saiz-Ros 1, Rafal Czapiewski 1 , Ilaria Epifano 2 , Andrew Stevenson 2, Selene K. Swanson 3, Charles R. Dixon 1 , Dario B. Zamora 1, Marion McElwee 2, Swetha Vijayakrishnan 2, Christine A. Richardson 4 , Li Dong 2, David A. Kelly 1 , Lior Pytowski 1 , Martin W. Goldberg 4, Laurence Florens 3 , Sheila V. Graham 2,* and Eric C. Schirmer 1,* 1 The Wellcome Centre for Cell Biology, University of Edinburgh, Edinburgh EH9 3BF, UK; [email protected] (N.S.-R.); [email protected] (R.C.); [email protected] (C.R.D.); [email protected] (D.B.Z.); [email protected] (D.A.K.); [email protected] (L.P.) 2 MRC-University of Glasgow Centre for Virus Research, Institute of Infection, Immunity and Inflammation, College of Medical, Veterinary and Life Sciences, University of Glasgow, Glasgow G61 1QH, UK; [email protected] (I.E.); [email protected] (A.S.); [email protected] (M.M.); [email protected] (S.V.); [email protected] (L.D.) 3 Stowers Institute for Medical Research, Kansas City, MO 64110, USA; [email protected] (S.K.S.); [email protected] (L.F.) 4 School of Biological and Biomedical Sciences, Durham University, Durham DH1 3LE, UK; [email protected] (C.A.R.); [email protected] (M.W.G.) * Correspondence: [email protected] (E.C.S.); [email protected] (S.V.G.); Tel: +44-(0)1316507075 (E.C.S.); +44-(0)1413306256 (S.V.G.) Received: 22 October 2018; Accepted: 31 January 2019; Published: 3 February 2019 Abstract: The primary envelopment/de-envelopment of Herpes viruses during nuclear exit is poorly understood. -

A Mutation in the Vesicle-Trafficking Protein VAPB Causes Late-Onset
Am. J. Hum. Genet. 75:822–831, 2004 A Mutation in the Vesicle-Trafficking Protein VAPB Causes Late-Onset Spinal Muscular Atrophy and Amyotrophic Lateral Sclerosis Agnes L. Nishimura,1 Miguel Mitne-Neto,1 Helga C. A. Silva,1,2 Antoˆnio Richieri-Costa,3 Susan Middleton,4 Duilio Cascio,5 Fernando Kok,1 Joa˜o R. M. Oliveira,1 Tom Gillingwater,4 Jeanette Webb,4 Paul Skehel,4 and Mayana Zatz1 1Human Genome Research Center, Department of Biology, Biosciences Institute, Sa˜o Paulo University, and 2Anesthesiology, Pain, and Intensive Care Department, Medical School of the Federal University of Sa˜o Paulo, Sa˜o Paulo; 3Genetics Service, Hospital of Rehabilitation of Craniofacial Anomalies, Sa˜o Paulo University, Bauru, Brazil; 4Division of Neuroscience, University of Edinburgh, Edinburgh; and 5Institute for Genomics and Proteomics, Molecular Biology Institute, University of California–Los Angeles Department of Energy (UCLA-DOE), Los Angeles Motor neuron diseases (MNDs) are a group of neurodegenerative disorders with involvement of upper and/or lower motor neurons, such as amyotrophic lateral sclerosis (ALS), spinal muscular atrophy (SMA), progressive bulbar palsy, and primary lateral sclerosis. Recently, we have mapped a new locus for an atypical form of ALS/ MND (atypical amyotrophic lateral sclerosis [ALS8]) at 20q13.3 in a large white Brazilian family. Here, we report the finding of a novel missense mutation in the vesicle-associated membrane protein/synaptobrevin-associated membrane protein B (VAPB) gene in patients from this family. Subsequently, the same mutation was identified in patients from six additional kindreds but with different clinical courses, such as ALS8, late-onset SMA, and typical severe ALS with rapid progression. -
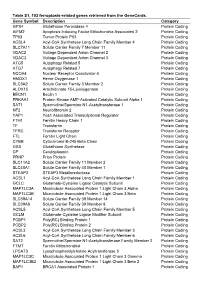
Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein