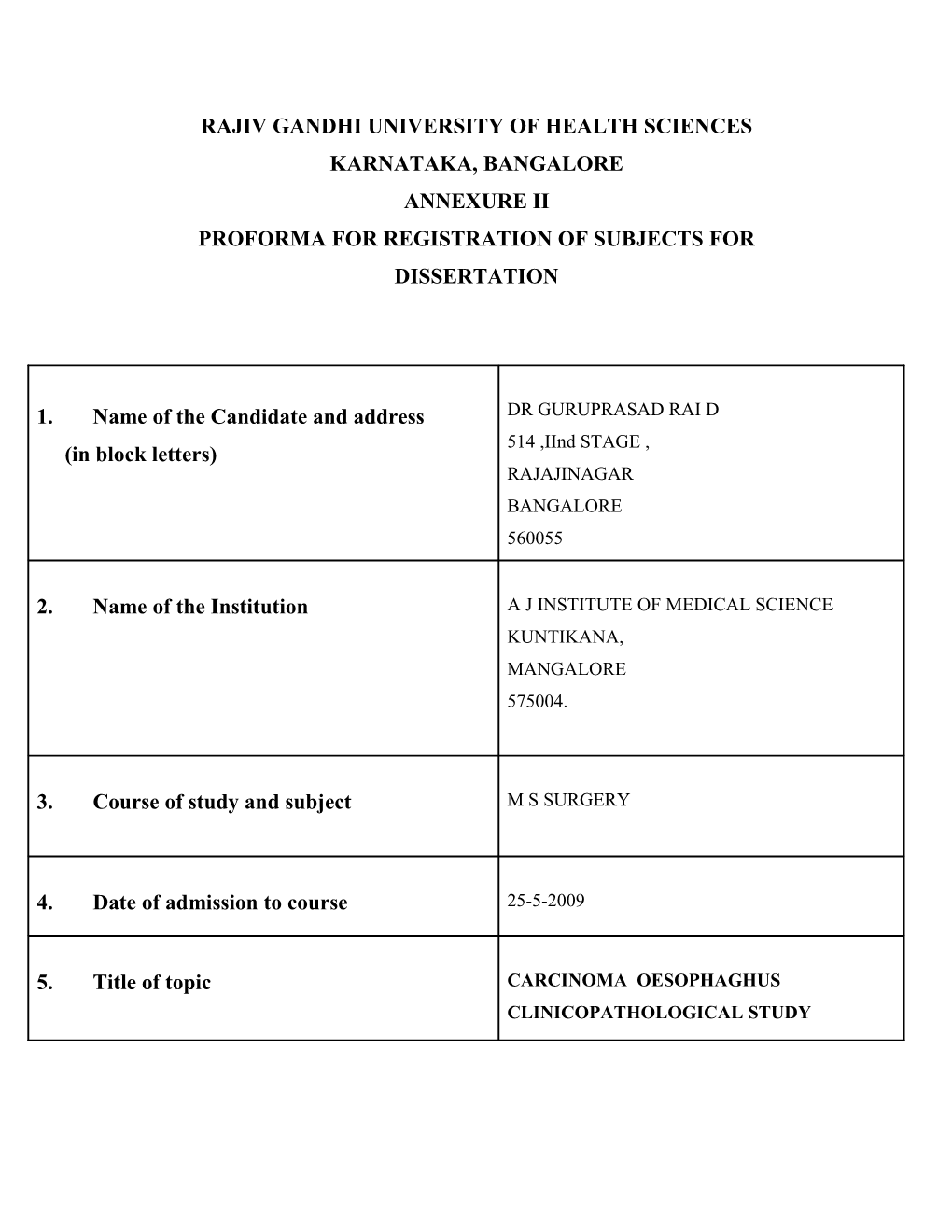
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES KARNATAKA, BANGALORE ANNEXURE II PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1. Name of the Candidate and address DR GURUPRASAD RAI D 514 ,IInd STAGE , (in block letters) RAJAJINAGAR BANGALORE 560055
2. Name of the Institution A J INSTITUTE OF MEDICAL SCIENCE KUNTIKANA, MANGALORE 575004.
3. Course of study and subject M S SURGERY
4. Date of admission to course 25-5-2009
5. Title of topic CARCINOMA OESOPHAGHUS CLINICOPATHOLOGICAL STUDY 6.0 Brief Resume of the intended Work : 6.1 Need for the study :
Cancer of the oesophaghus ranks twelfth among the major cancers in the number of new cases diagnosed and seventh in the number of cancer death. Its high mortality rate makes it a major concern. Overall survival rate 62.5% at 1 year,42.4% at 2 years,30% at 5 years The aim of the study is to review cases of the incidence of squamous cell carcinoma and adenocarcinoma of oesophagus in A J INSTITUTE OF MEDICAL SCIENCE .To study the etiological factors of esophageal carcinoma.Identify the disease presentation, progression, and prognostic factors for esophageal cancer.To study the distribution of these tumours in relation to the age ,gender and site of occurrence. Describe the epidemiology, work-up, and staging of esophageal cancer.Discuss the surgical approach and management of esophageal cancer
6.2 Review of Literature :
I)OESOPHAGUS ANATOMY(10)
The esophagus is a muscular tube passing between the pharynx in the neck and the stomach in the abdomen. It begins at the inferior border of the cricoid cartilage, opposite vertebra CVI, and ends at the cardiac opening of the stomach, opposite vertebra TXI.
The esophagus descends on the anterior aspect of the bodies of the vertebrae, generally in a midline position as it moves through the thorax. As it approaches the diaphragm, it moves anteriorly and to the left, crossing from the right side of the thoracic aorta to eventually assume a position anterior to it. It then passes through the esophageal hiatus, an opening in the muscular part of the diaphragm, at vertebral level TX.
The esophagus has a slight anterior-to-posterior curvature that parallels the thoracic portion of the vertebral column, and is secured superiorly by its attachment to the pharynx and inferiorly by its attachment to the diaphragm.
RELATIONSHIPS TO IMPORTANT STRUCTURES IN THE POSTERIOR MEDIASTINUM
In the posterior mediastinum, the esophagus is related to a number of important structures. The right side is covered by the mediastinal part of the parietal pleura. Posterior to the esophagus, the thoracic duct is on the right side inferiorly, but crosses to the left more superiorly. Also on the left side of the esophagus is the thoracic aorta.
Anterior to the esophagus, below the level of the tracheal bifurcation, are the right pulmonary artery and the left main bronchus.
Importantly, the esophagus passes immediately posteriorly to the left atrium, separated from it only by pericardium.
Inferior to the left atrium, the esophagus is related to the diaphragm.
Structures other than the thoracic duct posterior to the esophagus include portions of the hemiazygos veins, the right posterior intercostal vessels, and, near the diaphragm, the thoracic aorta.
The esophagus is a flexible, muscular tube that can be compressed or narrowed by surrounding structures at four locations
the junction of the esophagus with the pharynx in the neck; in the superior mediastinum where the esophagus is crossed by the arch of aorta; in the posterior mediastinum where the esophagus is compressed by the left main bronchus;
in the posterior mediastinum at the esophageal hiatus in the diaphragm.
ARTERIAL SUPPLY AND VENOUS AND LYMPHATIC DRAINAGE
The arterial supply and venous drainage of the esophagus in the posterior mediastinum involves many vessels. Esophageal arteries arise from the thoracic aorta, bronchial arteries, and ascending branches of the left gastric artery in the abdomen.
Venous drainage involves small vessels returning to the azygos vein, hemiazygos vein, and esophageal branches to the left gastric vein in the abdomen.
Lymphatic drainage of the esophagus in the posterior mediastinum returns to posterior mediastinal and left gastric nodes.
Innervation Innervation of the esophagus, in general, is complex. Esophageal branches arise from the vagus nerves and sympathetic trunks.
Striated muscle fibers in the superior portion of the esophagus originate from the branchial arches and are innervated by branchial efferents from the vagus nerves.
Smooth muscle fibers are innervated by components of the parasympathetic part of the autonomic division of the PNS, visceral efferents from the vagus nerves. These are preganglionic fibers that synapse in the myenteric and submucosal plexuses of the enteric nervous system in the esophageal wall.
Sensory innervation of the esophagus involves visceral afferent fibers originating in the vagus nerves, sympathetic trunks, and splanchnic nerves.
The visceral afferents from the vagus nerves are involved in relaying information back to the central nervous system about normal physiologic processes and reflex activities. They are not involved in the relay of pain recognition.
The visceral afferents that pass through the sympathetic trunks and the splanchnic nerves are the primary participants in detection of esophageal pain and transmission of this information to various levels of the central nervous system.
Esophageal plexus
After passing posteriorly to the root of the lungs, the right and left vagus nerves approach the esophagus. As they reach the esophagus, each nerve divides into several branches that spread over this structure, forming the esophageal plexus There is some mixing of fibers from the two vagus nerves as the plexus continues inferiorly on the esophagus toward the diaphragm. Just above the diaphragm, fibers of the plexus converge to form two trunks:
the anterior vagal trunk on the anterior surface of the esophagus, mainly from fibers originally in the left vagus nerve;
the posterior vagal trunk on the posterior surface of the esophagus, mainly from fibers originally in the right vagus nerve.
The vagal trunks continue on the surface of the esophagus as it passes through the diaphragm into the abdomen
B)PHYSIOLOGY OF THE OESOPHAGHUS :(12) GASTRO-OESOPHAGEAL REFLUX DISEASE
In some people, acid can escape from the stomach into the esophagus. The medical term for this is reflux or gastroesophageal reflux disease (GERD). In many cases, reflux causes symptoms such as heartburn or pain that seems to come from the middle of the chest. In some cases, though, reflux doesn't cause any symptoms at all. People with GERD have a risk of getting adenocarcinoma of the esophagus that is 2 to 16 times normal. The risk goes up based on how long the reflux has been going on and how severe the symptoms are. GERD can also cause Barrett's esophagus, which is linked to an even higher risk (discussed below). About 30% of esophageal cancer can be linked to GERD.
C)PATHOLOGY OF OESOPHAGHUS:
1)HIATUS HERNIA:
A hiatal hernia occurs when a portion of the stomach prolapses through the diaphragmatic esophageal hiatus. Although the existence of hiatal hernia has been described in earlier medical literature, it has come under scrutiny only in the last century or so because of its association with gastroesophageal reflux disease (GERD) and its complications. There is also an association between obesity and the presence of hiatal hernia. By far, most hiatal hernias are asymptomatic and are discovered incidentally. On rare occasion, a life-threatening complication, such as gastric volvulus or strangulation, may present acutely.
2)ACHALASIA CARDIA:
Achalasia is a disorder of the esophagus that prevents normal swallowing.Achalasia affects the esophagus, the tube that carries swallowed food from the back of the throat down into the stomach. A ring of muscle called the lower esophageal sphincter encircles the esophagus just above the entrance to the stomach. This sphincter muscle is normally contracted to close the esophagus. When the sphincter is closed, the contents of the stomach cannot flow back into the esophagus. Backward flow of stomach contents (reflux) can irritate and inflame the esophagus, causing symptoms such as heartburn. The act of swallowing causes a wave of esophageal contraction called peristalsis. Peristalsis pushes food along the esophagus. Normally, peristalsis causes the esophageal sphincter to relax and allow food into the stomach. In achalasia, which means "failure to relax," the esophageal sphincter remains contracted. Normal peristalsis is interrupted and food cannot enter the stomach
3)COCK SCREW OESOPHAGHUS:
A disorder characterised by episodic contractions of the oesophagus. The oesophageal spasms fail to effectively propel food to the stomach.
Symptoms may be confused with angina. Common symptoms include chest pains, epigastric pain, heartburn, pain on swallowing and difficulty swallowing.
4)OESOPHAGEAL WEBS
A web is an abnormal bulge of tissue that causes an area of narrowing in the esophagus. This can lead to a feeling like food gets stuck when it is swallowed. When an esophageal web is found along with anemia, tongue irritation (glossitis), brittle fingernails, and a large spleen it is called Plummer- Vinson syndrome. Another name for this is Paterson-Kelly syndrome. About 1 in 10 patients with this syndrome eventually develop squamous cell cancer of the esophagus.
5)PLUMMER WILSON SYNDROME:
A disorder marked by anemia caused by iron deficiency, and a web-like growth of membranes in the throat that makes swallowing difficult. Having Plummer-Vinson syndrome may increase the risk of developing esophageal cancer. Also called Paterson-Kelly syndrome and sideropenic dysphagia.
6)MALLORY WEISS SYNDROME:
Mallory-Weiss syndrome is bleeding from an arterial blood vessel in the upper gastrointestinal tract, caused by a mucosal gastric tear at or near the point where the esophagus and stomach join. Mallory-Weiss syndrome causes about 5% of all upper gastrointestinal bleeding. The condition was originally diagnosed in alcoholics and is associated with heavy alcohol use, although it can also be found in patients who are not alcoholics. Earlier episodes of heavy hiccupping, vomiting, and retching are reported by about half the patients who are diagnosed with Mallory-Weiss syndrome. It is thought that the tear or laceration occurs when there is a sudden increase in intra- abdominal pressure. Patients with increased pressure in the vein leading into the liver (portal hypertension) are more likely to bleed heavily from an esophageal laceration than those whose blood pressure is normal.
7)BARRETS OESOPHAGHUS:
If reflux of stomach acid into the lower esophagus continues for a long time, it can damage the lining of the esophagus. This causes the squamous cells that usually line the esophagus to be replaced with glandular cells. These glandular cells usually look like the cells that line the stomach and the small intestine, and are more resistant to stomach acid. This condition is known as Barrett's (or Barrett) esophagus. About 10% of people with symptoms of gastroesophageal reflux disease (GERD) have this condition. The longer someone has GERD, the more likely that they have Barrett's esophagus. Most people with Barrett's esophagus have had symptoms of "heartburn," but many have no symptoms at all. Barrett's esophagus increases the risk of adenocarcinoma of the esophagus. This is because the gland cells in Barrett's esophagus can become more abnormal over time until they become dysplasia, a pre-cancerous condition. Dysplasia is graded by how abnormal the cells look like under the microscope. High-grade dysplasia is the most abnormal. People with Barrett's esophagus are anywhere from 30 to 125 times more likely than people without this condition to develop esophageal cancer. Still, many people with Barrett's esophagus do not get esophageal cancer. The exact risk of developing cancer in people with Barrett's esophagus is not known, but researchers estimate it to be only 1 in 200 per year.
D)INVESTIGATIONS : A) BARIUM RADIOLOGY(BARIUM SWALLOW/MEAL) B) UPPER GI ENDDOSCOPY C) HISTOLOGIC DIAGNOSIS – BIOPSY D) COMPUTED TOMOGRAPHY (CT) E) BRONCHOSCOPY F) CHEST X RAY G) U S G ABDOMEN H) P H MANOMETRY
E)CARCINOMA
1)STUDY:
A) Squamous cell carcinoma Age -60–70 years, Sex -Male dominant, lower socioeconomic Group Associations -Head and neck cancer, smoking, alcohol excess and liver dysfunction, radiation exposure, achalasia, poor nutritional status, human papillomavirus (HPV) infection, Helicobacter pylori infection, Plummer–Vinson syndrome, tylosis palmaris, lye ingestion Location -Mostly midesophagus (75% at level of tracheal bifurcation) and with a prominently linear growth pattern and wider nodal spread Symptoms and wider nodal spread- Progressive dysphagia, odynophagia, halitosis, unintentional weight loss,chest pain.
B) Adenocarcinoma Age -50–60 years Sex -Male dominant, middle or upper socioeconomic group Associations Barrett’s esophagus, gastroesophageal reflux disease, hiatus hernia, obesity, scleroderma, family history Location Almost always distal one-third of esophagus (94% entirely subcarinal) and radial growth pattern with early local nodal dissemination Symptoms and wider nodal spread Progressive dysphagia, odynophagia, halitosis, unintentional weight loss, chest pain
2)ETIOLOGY: (8,9)
Age
The chance of getting esophageal cancer is low at younger ages and increases with age. Less than 15% of cases are found in people younger than age 55. Most cases occur in those 65 and older.
Gender
Compared with women, men have a 3-fold higher rate of esophageal cancer.
Gastroesophageal reflux disease
In some people, acid can escape from the stomach into the esophagus. The medical term for this is reflux or gastroesophageal reflux disease (GERD). In many cases, reflux causes symptoms such as heartburn or pain that seems to come from the middle of the chest. In some cases, though, reflux doesn't cause any symptoms at all. People with GERD have a risk of getting adenocarcinoma of the esophagus that is 2 to 16 times normal. The risk goes up based on how long the reflux has been going on and how severe the symptoms are. GERD can also cause Barrett's esophagus, which is linked to an even higher risk (discussed below). About 30% of esophageal cancer can be linked to GERD.
Barrett's esophagus
If reflux of stomach acid into the lower esophagus continues for a long time, it can damage the lining of the esophagus. This causes the squamous cells that usually line the esophagus to be replaced with glandular cells. These glandular cells usually look like the cells that line the stomach and the small intestine, and are more resistant to stomach acid. This condition is known as Barrett's (or Barrett) esophagus. About 10% of people with symptoms of gastroesophageal reflux disease (GERD) have this condition. The longer someone has GERD, the more likely that they have Barrett's esophagus. Most people with Barrett's esophagus have had symptoms of "heartburn," but many have no symptoms at all. Barrett's esophagus increases the risk of adenocarcinoma of the esophagus. This is because the gland cells in Barrett's esophagus can become more abnormal over time until they become dysplasia, a pre- cancerous condition. Dysplasia is graded by how abnormal the cells look like under the microscope. High-grade dysplasia is the most abnormal. People with Barrett's esophagus are anywhere from 30 to 125 times more likely than people without this condition to develop esophageal cancer. Still, many people with Barrett's esophagus do not get esophageal cancer. The exact risk of developing cancer in people with Barrett's esophagus is not known, but researchers estimate it to be only 1 in 200 per year.
Tobacco and alcohol
The use of tobacco products, including cigarettes, cigars, pipes, and chewing tobacco, is a major risk factor for esophageal cancer. The risk goes up with increased use -- the more cigarettes smoked per day and the longer a person uses tobacco, the higher the cancer risk. Someone who smokes at least a pack a day has twice the chance of getting adenocarcinoma of the esophagus than a nonsmoker. The link to squamous cell esophageal cancer is even stronger, with more than half of all cases linked to smoking. The risk of esophageal cancer improves if tobacco use stops.
Drinking alcohol also increases the risk of esophageal cancer. The chance of getting esophageal cancer goes up with higher intake of alcohol. Alcohol affects the risk of the squamous cell type more than the risk of adenocarcinoma. Combining smoking and drinking alcohol raises the risk of esophageal cancer much more than using either alone.
Obesity
People who are overweight or obese have a higher chance of getting adenocarcinoma of the esophagus. This is in part explained by the link between obesity and esophageal reflux.
Diet
A diet high in fruits and vegetables is linked to a lower risk of esophageal cancer. Eating these foods raw has the best effect on risk. Fruits and vegetables provide a number of vitamins and minerals that may help prevent cancer. About 15% of esophageal cancer can be linked to a diet poor in fruits and vegetables. Certain substances in the diet may increase the cancer risk. This may explain the high rate of this cancer in certain parts of the world. There have been suggestions, as yet unproven, that a diet high in processed meat may also increase the chance of developing esophageal cancer. Overeating, which leads to obesity (being extremely overweight), increases the risk of the adenocarcinoma of the esophagus. Frequent drinking of very hot liquids may increase the risk for the squamous cell type of esophageal cancer.
Workplace exposures
Exposure to the solvents used for dry cleaning may lead to a greater risk of esophageal cancer. Dry cleaning workers have a higher rate of esophageal cancer. Exposure to other chemical fumes also may lead to an increased risk of esophageal cancer.
Injury to the esophagus
Lye is a chemical found in strong industrial and household cleaners such as drain cleaners. Lye is a corrosive agent, meaning it can burn and destroy cells. Sometimes small children find a lye-based cleaner and drink from the bottle. The lye causes a severe chemical burn in the esophagus. As the injury heals, the scar tissue can cause an area of the esophagus to become very narrow (called a stricture). People with these strictures have a high rate of the squamous cell type of esophageal cancer as adults. The cancers occur on average about 40 years after the lye was swallowed.
Achalasia
In this disease, the muscle at the lower end of the esophagus (the lower esophageal sphincter) does not relax properly. Food and liquid that are swallowed have trouble passing into the stomach and tend to collect in the esophagus. The esophagus above this muscle becomes dilated (larger). People with achalasia have a risk of esophageal cancer that is at least 15 times normal. About 6% (1 in 20) of all achalasia patients develop squamous cell cancer of the esophagus. On average, the cancers are found about 17 years after the achalasia is diagnosed. Tylosis
This is a rare, inherited disease that causes excess growth of the top layer of skin on the palms of the hands and soles of the feet. People with this condition develop abnormal areas in the lining of the mouth. They also have a very high risk of getting squamous cell cancer of the esophagus. People with tylosis are watched closely to try to find esophageal cancer early. Often this involves regular monitoring with an upper endoscopy (scope with camera placed to view the esophagus). This disorder is linked to a gene on an area of chromosome 17 called TOC.
Esophageal webs
A web is an abnormal bulge of tissue that causes an area of narrowing in the esophagus. This can lead to a feeling like food gets stuck when it is swallowed. When an esophageal web is found along with anemia, tongue irritation (glossitis), brittle fingernails, and a large spleen it is called Plummer-Vinson syndrome. Another name for this is Paterson-Kelly syndrome. About 1 in 10 patients with this syndrome eventually develop squamous cell cancer of the esophagus.
Stomach bacteria
A certain bacteria called H. pylori can cause many stomach problems, including ulcers and even some types of cancer. Infection with this bacteria can be treated with antibiotics plus a drug to stop stomach acid. People who have had treatment to rid the stomach of H. pylori get adenocarcinoma of the esophagus more often than expected. It seems that H. pylori infection can cause the stomach to make less acid. The lower levels of acid mean that the stomach contents are less harmful to the esophagus (in people with reflux). The infection causes many problems in the stomach, but it may actually protect the esophagus.
Other cancers
People who have had certain other cancers, such as lung cancer, mouth cancer, and throat cancer have a high risk of getting esophageal cancer as well. This may be because these cancers are all caused by smoking
3)PATHOPHYSIOLOGY:
Esophageal carcinoma arises in the mucosa. Subsequently, it tends to invade the submucosa and the muscular layer and, eventually, contiguous structures such as the tracheobronchial tree, the aorta, or the recurrent laryngeal nerve. The tumor also tends to metastasize to the periesophageal lymph nodes and, eventually, to the liver, lungs, or both.
The staging of the disease based on tumor invasion of the esophageal wall (T), involvement of lymph nodes (N), and the presence of metastases (M). Unfortunately, by the time the first symptoms manifest, the cancer has already spread to lymph nodes (mediastinal, cervical, celiac) in most patients.
The three ways that cancer spreads in the body are:
Through tissue. Cancer invades the surrounding normal tissue. Through the lymph system. Cancer invades the lymph system and travels through the lymph vessels to other places in the body. Through the blood. Cancer invades the veins and capillaries and travels through the blood to other places in the body.
When cancer cells break away from the primary (original) tumor and travel through the lymph or blood to other places in the body, another (secondary) tumor may form. This process is called metastasis. The secondary (metastatic) tumor is the same type of cancer as the primary tumor.
4)INVESTIGATIONS:
a)GENERAL WORK UP: 1.Hb% is low, which causes generalized weakness. 2.TC,DC,ESR 3.RBS 4.UREA,CREATITINE
b)METASTATIC WORK UP: . 1. Liver function test (LFT): if secondaries in liver occur.
2. Ultra sound is done to rule out liver secondaries, lymph nodes in the porta hepatic, coeliac nodes etc. 3. Chest X ray look for secondaries
c)DIAGNOSTIC WORK UP: 1.Barium swallow demonstrates irregular, persistent, intrinsic filling defect.
2 .Oesophagoscopy to visualize the growth and to take biopsy.
3.Chest x-ray to rule out aspiration pneumonia and mediastinal widening.
4. Bronchoscopy to rule out involvement of bronchus, as in carcinoma middle ⅓.
5.C.T scans of the chest to find out local infiltration
6.PH manometry
5)TREATING CANCER OF THE ESOPHAGUS BY STAGE:(2,3,6,7,14) Chemotherapy Oral or intravenous chemotherapy alone will not cure esophageal cancer, but pre-operative treatments can shrink tumors and increase the probability that cancer can be surgically eradicated. Palliative chemotherapy can relieve symptoms of advanced cancer but will not alter the outcome of the disease. Radiation External beam or internal radiation, delivered by machine or implanted near cancer cells inside the body, is only rarely used as the primary form of treatment. Post-operative radiation is sometimes used to kill cancer cells that couldn't be surgically removed. Palliative radiation is effective in relieving dysphagia in patients who cannot be cured. However, radiation is most useful when combined with chemotherapy as either the definitive treatment or preoperative treatment.
Surgery
Only 40% tumours are resectable Operative mortality now less than 10% Treatment should be in centres who perform operation regularly No place for the occasional operator Preoperative chemotherapy may be beneficial
Operative approaches
Need 10 cm proximal clearance to avoid submucosal spread.
Total gastrectomy via thoracoabdominal approach (Adenocarcinoma) Subtotal two-stage oesophagectomy (Ivor-Lewis) Subtotal three-stage oesophagectomy (McKeown) Transhiatal oesophagectomy
Palliative treatment
Aim to relieve obstruction and dysphagia with minimal morbidity
Oesophageal intubation o Open surgical intubation (Celestin or Mousseau-Barbin tubes) now obsolete o Endoscopic or radiological placement now most commonly practiced o Atkinson tube is the most commonly placed endoscopically o Requires dilatation with risk of oesophageal perforation o Recent increased use of self-expanding stents that require no pre-dilatation o Complications of stents and tubes: . Oesophageal perforation . Tube displacement or migration . Tube blockage due to ingrowth or overgrowth
Laser therapy o Produces good palliation in over 60% of cases o May need to be repeated every 4 to 6 weeks o Associated with oesophageal perforation in about 5% cases External beam radiotherapy Brachytherapy Diathermy
Alcohol injection
II) Socioeconomic Factors and Risk of Esophageal Adenocarcinoma: A Nationwide Swedish(4) Background: The increase in esophageal adenocarcinoma incidence in developed countries remains unexplained.Although low socioeconomic status (SES) is linked to an increased risk of esophageal squamous cell carcinoma (SCC), the relation with adenocarcinoma is uncertain. Results: The risk of both esophageal adenocarcinoma and SCC increased with decreasing SES; unskilled workers had 3.7-fold (95% CI, 1.7-7.7) and 2.1-fold (95% CI, 1.0-4.7) increased risks, respectively, compared with age- and sexcomparable professionals. Adjustment for reflux symptoms, body mass, and tobacco smoking attenuated the excess risk for esophageal adenocarcinoma, whereas adjustment for Helicobacter pylori infection in a subset of the interviewed participants did not influence the results. Life without a partner was associated with a >2- fold increased risk of both histologic types of esophageal cancer, associations that remained even after multiple adjustments. Conclusions: Esophageal adenocarcinoma and SCC are both linked to low SES and a life without a partner.These associations are only partly explained by established risk factors.
III)Precursor Lesions of Esophageal Cancer in High-Risk Populations in Henan Province, China(13) This report discusses precancerous changes in the esophageal mucosa from three points of view: the histopathologic features of the esophageal mucosa in persons known to be at high risk for esophageal carcinoma (EC); the histopathologic features of the esophageal mucosa of asymptomatic persons randomly selected from areas at high and low risk for EC; and a prospective follow-up of a randomly examined group to determine the impact of esophagitis and dysplasia upon subsequent development of EC. Esophagitis was commonly found at endoscopic examination, but there was no difference in frequency of esophagitis in the randomly selected subjects from high- risk and low-risk areas. Although one third of patients with dysplasia developed cancer over a follow-up period of 30 to 78 months, only 4% of those with esophagitis alone developed EC. The authors conclude that dysplasia, diagnosed by cytologic or histologic examination, is a precancerous state, and that esophagitis is a nonspecific pathologic condition of the esophagus, but moderate and severe types of chronic esophagitis might create an environment favorable for the development of esophageal carcinoma.
IV) Functional Esophageal Disorders(5) Functional esophageal disorders represent processes accompanied by typical esophageal symptoms (heartburn, chest pain, dysphagia, globus) that are not explained by structural disorders, histopathology-based motor disturbances, or gastroesophageal reflux disease. Gastroesophageal reflux disease is the preferred diagnosis when reflux esophagitis or excessive esophageal acid exposure is present or when symptoms are closely related to acid reflux events or respond to antireflux therapy. A singular, well-defined pathogenetic mechanism is unavailable for any of these disorders; combinations of sensory and motor abnormalities involving both central and peripheral neural dysfunction have been invoked for some. Treatments remain empirical, although the efficacy of several interventions has been established in the case of functional chest pain. Management approaches that modulate central symptom perception or amplification often are required once local provoking factors (eg, noxious esophageal stimuli) have been eliminated. Future research directions include further determination of fundamental mechanisms responsible for symptoms, development of novel management strategies, and definition of the most cost-effective diagnostic and treatment approaches.
V)Nutritional Risk Factors in Esophageal Cancer(9)
Objective : The present case-control study was undertaken with the objective to study the nutritional risk factors associated with esophageal cancer. Results : Multivariate analysis revealed that the risk of esophageal cancer was 7.81 times (p < 0.01) higher with daily consumption of alcohol. The risk increased to 3.16 times (p < 0.01) with the daily habit of chewing of betel leaf with tobacco. Nearly a two fold risk was observed when the consumption of “other vegetables” was less than four times per week. A 1.95 times (p < 0.01) increase in risk was observed with the daily habit of bidi smoking. Conclusion : Cancers in general are multifactorial in origin, and several environmental interactions are possible. It is not easy to quantify the contribution of diet to cancer risk. However, the results of the present study suggested that nutritional factors do play a role
VI) ASGE guideline: the role of endoscopy in the surveillance of premalignant conditions of the upper GI tract(1) This is one of a series of statements discussing the utilization of gastrointestinal endoscopy in common clinical situations. The Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy prepared this text. In preparing this guideline, a MEDLINE literature search was performed, and additional references were obtained from the bibliographies of the identified articles and from recommendations of expert consultants. When little or no data exist from well- designed prospective trials, emphasis is given to results from large series and reports from recognized experts. Guidelines for appropriate utilization of endoscopy are based on a critical review of the available data and expert consensus. Further controlled clinical studies are needed to clarify aspects of this statement, and revision may be necessary as new data appear. Clinical consideration may justify a course of action at variance to these recommendations.
VII)Factors contributing to deficiencies in cell-mediated immunity in esophageal cancer patients (11) Based on the previous data which indicated a preoperative decrease in cell-mediated immunity (CMI) is associated with the occurrence of infectious complications following surgery on patients with esophageal cancer, we examined possible factors contributing to a decrease in CMI levels. A multiple linear regression analysis was made on data from 76 patients with esophageal cancer and 53 with gastric cancer as the control. In patients with esophageal cancer, both protein-calorie malnutrition (PCM) and age factor contributed to a decrease in CMI, although the contribution of the latter was weak while the stage of the cancer and the grade of dysphagia showed no such contribution. The PCM and stage of the cancer were contributing factors in patients with gastric cancer. Thus, these results indicate that PCM and old age, and not the presence of malignant tumors, play a significant role in deficiency in CMI in patients with esophageal cancer.
VIII) Association of smoking, alcohol drinking and dietary factors with esophageal cancer in high- and low- risk areas of Jiangsu Province, China(8) AIM: To study the main environmental and lifestyle factors that account for the regional differences in esophageal cancer (EC) risk in low- and high-risk areas of Jiangsu Province, China. RESULTS: In the preliminary analysis of the ongoing study, we recruited 291 pairs of cases and controls in Dafeng and 240 pairs of cases and controls in Ganyu, respectively. In both low-risk and high-risk areas, EC was inversely associated with socio-economic status, such as level of education, past economic status and body mass index. However, this disease was more frequent among those who had a family history of cancer or encountered misfortune in the past 10 years. EC was also more frequent among smokers, alcohol drinkers and fast eaters. Furthermore, there was a geographic variation of the associations between smoking, alcohol drinking and EC risk despite the similar prevalence of these risk factors in both low-risk and high-risk areas. The dose-response relationship of smoking and smoking related variables, such as age of the first smoking, duration and amount were apparent only in high-risk areas. On the contrary, a dose-response relationship on the effect of alcohol drinking on EC was observed only in low-risk areas. CONCLUSION: The environmental risk factors, together with genetic factors and gene-environmental interactions might be the main reason for this high-risk gradient in Jiangsu Province, China.
IX) Esophageal Cancer: CT, Endoscopic US, and FDG PET for Assessment of Response to Neoadjuvant Therapy—Systematic Review1(14) PURPOSE: To compare diagnostic accuracy of computed tomography (CT), endoscopic ultrasonography (US), and fluorine 18 fluorodeoxyglucose (FDG) positron emission tomography (PET) for assessment of response to neoadjuvant therapy in patients with esophageal cancer by using a systematic review of the literature. RESULTS: Four studies with CT, 13 with endoscopic US, and seven with FDG PET met inclusion criteria. Percentages of the maximum score in regard to methodological quality ranged from 15% to 100%. Summary ROC analysis could be performed for three studies with CT, four with endoscopic US, and four with FDG PET. The maximum joint values for sensitivity and specificity were 54% for CT, 86% for endoscopic US, and 85% for FDG PET. Accuracy of CT was significantly lower than that of FDG PET (P _ .006) and of endoscopic US (P _ .003). Accuracy of FDG PET and that of endoscopic US were similar (P _ .839). In all patients, CT was always feasible, whereas endoscopic US was not feasible in 6% of the patients, and FDG PET was not feasible in less than 1%. CONCLUSION: CT has poor accuracy for assessment of response to neoadjuvant therapy in patients with esophageal cancer. Endoscopic US and FDG PET have equivalent good accuracy, but endoscopic US is not always feasible after chemotherapy and radiation therapy. FDG PET seems to be a promising noninvasive tool for assessment of neoadjuvant therapy in patients with esophageal cancer
X) Multiple Management Modalities in Esophageal Cancer: Epidemiology, Presentation and Progression, Work-up, and Surgical Approaches (6) Annually, approximately 13,200 people in the U.S. are diagnosed with esophageal cancer and 12,500 die of this malignancy. Of new cases, 9,900 occur in men and 3,300 occur in women. In part I of this two-part series, we explore the epidemiology, presentation and progression, work-up, and surgical approaches for esophageal cancer. In the 1960s, squamous cell cancers made up greater than 90% of all esophageal tumors. The incidence of esophageal adenocarcinomas has risen considerably over the past two decades, such that they are now more prevalent than squamous cell cancer in the western hemisphere.Despite advances in therapeutic modalities for this disease, half the patients are incurable at presentation, and overall survival after diagnosis is grim. Evolving knowledge regarding the etiology of esophageal carcinoma may lead to better preventive methods and treatment options for early stage superficial cancers of the esophagus. The use of endoscopic ultrasound and the developing role of positron emission tomography have led to better diagnostic accuracy in this disease. For years, the standard of care for esophageal cancer has been surgery; there are several variants of the surgical approach. We will discuss combined modality approaches in part II of this series. XI)Guidelines for the management of oesophageal and gastric cancer(2)
These guidelines have developed as a joint project between the Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland, the British Society of Gastroenterology, and the British Association of Surgical Oncology. They have been produced as part of the wider initiative of the British Society of Gastroenterology to provide guidance for clinicians in several areas of clinical practice related to the broad field of gastroenterology. Over the past 10 years there have been many significant changes in the management of oesophageal and gastric cancer. Both diseases have shown remarkable changes in epidemiology with a concentration of tumours adjacent to the oesophagogastric junction. Advances in established investigative techniques and developments in new technology have radically altered the way in which the two diseases can be assessed without the need for surgery. Greater understanding of the natural history has significantly influenced the approach to diagnosis and to treatment options. Appreciation of the fundamental need for multidisciplinary treatment planning has reflected greater recognition by all interested clinicians of the role of the various treatment modalities. The essential role of best supportive care has significantly evolved emphasising the need for a holistic approach to all patients.These guidelines have been written to emphasise these recent developments and to place them in the context of established approaches to enable clinicians to incorporate them into their clinical practice. They have not been written, nor are they intended, to be prescriptive, as such an approach would interfere with clinical judgement. However, they have been produced based on careful review of the available evidence with the recommendations weighted according to the strength of the evidence. As with other similar recommendations, much of the evidence is based on consensus view as in many areas scientific evaluation has not taken place or is not possible. Such limitations are inevitable in some areas of clinical practice. As a result, improvements will be appropriate but such improvements will only be possible once standards such as these have undergone appropriate assessment in prospective audit. These guidelines are thus an initial phase in an audit cycle and will need to be revised after a relatively short period of time.
XII) CHEMOTHERAPY FOLLOWED BY SURGERY COMPARED WITH SURGERY ALONE FOR LOCALIZED ESOPHAGEAL CANCER(7) . Background We performed a multi-institutional randomized trial comparing preoperative chemotherapy followed by surgery with surgery alone for patients with local and operable esophageal cancer.. Results Of the 440 eligible patients with adequate data, 213 were assigned to receive preoperative chemotherapy and 227 to undergo immediate surgery. After a median possible study time of 55.4 months, there were no significant differences between the two groups in median survival: 14.9 months for the patients who received preoperative chemotherapy and 16.1 months for those who underwent immediate surgery (P=0.53). At one year, the survival rate was 59 percent for those who received chemotherapy and 60 percent for those who had surgery alone; at two years, survival was 35 percent and 37 percent, respectively. The toxic effects of chemotherapy were tolerable, and the addition of chemotherapy did not appear to increase the morbidity or mortality associated with surgery. There were no differences in survival between patients with squamous-cell carcinoma and those with adenocarcinoma. Weight loss was a significant predictor of poor outcome (P=0.03). With the addition of chemotherapy, there was no change in the rate of recurrence at locoregional or distant sites. Conclusions Preoperative chemotherapy with a combination of cisplatin and fluorouracil did not improve overall survival among patients with epidermoid cancer or adenocarcinoma of the esophagus. XIII)CARCINOMA OESOPHAGUS; COMPARISON OF VARIOUS TREATMENT MODALITIES(3) Objective: To compare various modalities of treatment in management of carcinoma oesophagus with particular stress on relief of dysphagia due to ca. Results: Of the 33 cases, 29 were operated out of which 11 were subjected to Ivor-lewis procedure, 15 were operated upon through transhiatal approach while in the remaining cases, palliative bypass procedures were done. Conclusion: Surgery (transthoracic + tans hiatal approach) proved to be the only reliable mode of treatment whether supplemented by adjuvant therapy or not, Chemo/radiation as a sole mode of treatment had drastic results.
6.3 Objectives of the study :
1) The aim of the study is to review cases of the incidence of squamous cell carcinoma and adenocarcinoma of oesophagus in A J INSTITUTE OF MEDICAL SCIENCE. 2) To study the etiological factors of esophageal carcinoma. 3) Identify the disease presentation, progression, and prognostic factors for esophageal cancer 4) To study the distribution of these tumours in relation to the age ,gender and site of occurrence. 5) Describe the epidemiology, work-up, and staging of esophageal cancer 6) Discuss the surgical approach and management of esophageal cancer
7.0 Material and Methods : 7.1 Source of data : Study will be done at A J Medical College Hospital The study period is from 01-6-2009 to 31-06-2011.
7.2 Method of Collection of data : INCLUSION CRITERIA:
Patients of all ages, sex or occupation primarily diagnosed in out patients department and later confirmed by radiological /histopathological reports were included in the study.
EXCLUSION CRITERIA :
Patients excluded from study were; 1. Where multiple concurrent tumors were found on CT scan in other parts of GIT. 2. Patients who were bound to be lost in follow up 3. Patients insisting on having treatment from abroad.
7.3 Does the study require any investigations or interventions to be conducted on patients or other humans or animals ? If so please describe briefly. YES A) BARIUM RADIOLOGY(BARIUM SWALLOW/MEAL) B) UPPER GI ENDDOSCOPY C) HISTOLOGIC DIAGNOSIS – BIOPSY D) COMPUTED TOMOGRAPHY (CT) E) BRONCHOSCOPY F) CHEST X RAY G) U S G ABDOMEN H) P H MANOMETRY
7.4 Has ethical clearance been obtained from your institution in case of 7.3 ? YES
8.0 References :
1) American Society For Gastrointestinal Endoscopy ;ASGE Guideline: The Role Of Endoscopy In The Surveillance Of Premalignant Conditions Of The Upper GI Tract; Gastrointest Endosc 1998;48:663-8.
2) Allum WH; Griffin SM; Watson A; Jones D Colin; Guidelines For The Management Of Oesophageal Andgastric Cancer; The British Society Of Gastroenterology, And The British Association Of Surgical Oncology ;Gut 2002;50(Suppl V):V1–V23
3) DR. REHAN-E-KIBRIA ,DR. ASAD MAHMUD MALIK: CARCINOMA OESOPHAGUS; COMPARISON OF VARIOUS TREATMENT MODALITIES
4) Jansson Catarina, L.V. Johansson Anna, Nyre´N Olof, And Lagergren Jesper ; Socioeconomic Factors And Risk Of Esophageal Adenocarcinoma: A Nationwide Swedish Case-Control Study
5) JEAN PAUL GALMICHE; RAY E. CLOUSE; ANDRÁS BÁLINT; IAN J. COOK; PETER J. KAHRILAS; WILLIAM G. PATERSON; Functional Esophageal Disorders 6) KOSHY MARY; ESIASHVILLI NATIA; LANDRY JEROME C; THOMAS JR CHARLES R; MATTHEWS RICHARD H.; Multiple Management Modalities In Esophageal Cancer: Epidemiology, Presentation And Progression, Work-Up, And Surgical Approaches ; The Oncologist 2004;9:137-146
7) KELSEN DAVIDP; ROBERTGINSBERG ; Chemotherapy Followed By Surgery Compared With Surgery Alonefor Localized Esophageal Cancer; (N Engl J Med 1998;339:1979-84.)
8) Ming Wu; Zhao Jin-Kou; Hu Xiao-Shu; Wang Pei-Hua; Chang Lu Yu; Qin;Yin-;Et Al ;Association Of Smoking, Alcohol Drinking And Dietary Factors With Esophageal Cancer In High- And Low-Risk Areas Of Jiangsu Province, China; Pieter Van’t Veer © 2006 The WJG Press
9) Nayar Deepika; Kapil U; Joshi YK, Sundaram KR, Srivastava SP, Shukla NK, Tandon RK ;Nutritional Risk Factors In Esophageal Cancer ;Received : 25.3.1999; Revised : 16.11.1999; Accepted : 15.3.2000. (JAPI 2000; 48 : 781-787)
10)Richard L Drake; Volg Wayne; Mithchell Adam W M ;Gray’s Anatomy For Students
11) Saito Takao; Kuwahara Akihiko; Shimoda Katsuhiro; Kinoshita Tadahiko; Nakamura Akira ; Miyahara Masaki Et Al; Factors Contributing To Deficiencies In Cell-Mediated Immunity In Esophageal Cancer Patients ; 879-55 Oita, Japan Received: 21 December 1990
12) S. Satvinder; Mudan And Kang Jin-Yong ; Epidemiology And Clinical Presentation In Esophageal Cancer Cambridge University Press
13) SONGLIANG QIU AND GUANRUI YANG ;Precursor Lesions Of Esophageal Cancer In High-Risk Populations In Henan Province, China
14) Westerterp Marinke; Westreenen Henderik L. Van; Reitsma Johannes B; Hoekstra Otto S; Stoker Jaap; Fockens Paul;Esophageal Cancer: CT, Endoscopic US, And FDG PET For Assessment Of Response To Neoadjuvant Therapy— Systematic Review; Published Online 10.1148/Radiol.2363041042 Radiology 2005; 236:841–851
9.0 Signature of Candidate :
10.0 Remarks of the guide : 11.0 Name and Designation the: DR DEVIDAS SHETTY of Guide ( in block letters) PROFESSOR A J I M S ,MANGALORE
11.1 Signature:
11.2 Co-Guide (If any)
11.3 Signature
11.4 Head of the Department DR ASHOK HEGDE
11.5 Signature
12.0 Principal : DR RAMESH PAI
12.1 Remarks of the Principal
12.2 Signature TIMELINE
TITLE : CLINICOPATHOLOGICAL STUDY OF CARCINOMA OESOPHAGHUS
Phase Time Period Activity 1. June - 2009 to 1. Idenification of the Problem
December – 2009 2. Review of literature 3. Preparing of Proforma 4. Pilot Study 5. Preparation and submission of synopsis 2. January 2010
To Collection of Data
December 2010 3. January 2011
To Analysis and Discussion of collected data
December 2011 Publication From, Dr. Guruprasad Rai D, Post Graduate in Department of SURGERY A.J. Institute of Medical Science Mangalore
To, The Registrar (Evaluation) Rajiv Gandhi University of Health Sciences Bangalore, Karnataka
(Through Proper Channel)
Sub:- Submission of Synopsis of Dissertation
Respected Sir,
Herewith, I am submitting synopsis of my dissertation work “CLINICOPATHOLOGICAL STUDY OF CARCINOMA OESOPHAGHUS” for registration in M.S. (SURGERY) of A.J. Institute of Medical Science Mangalore. Kindly accept the same and oblige.
Thanking you. Yours faithfully, Place : Mangalore Date : 14.10.2009 (Dr.GURUPRASAD RAI D)
Head of the Department Dr. ASHOK HEGDE Prof. and Head, Department of SURGERY A.J. Institute of Medial Science
DEAN A.J. Institute of Medical Science Mangalore
CONSENT FOR PARTICIPATION IN RESEARCH CLINICOPATHOLOGICAL STUDY OF CARCINOMA OESOPHAGHUS Purpose of study: 1) The aim of the study is to review cases of the incidence of squamous cell carcinoma and adenocarcinoma of oesophagus in and around Mangalore. 2) To study the etiological factors of esophageal carcinoma. 3) Identify the disease presentation, progression, and prognostic factors for esophageal cancer 4) To study the distribution of these tumours in relation to the age ,gender and site of occurrence. 5) Describe the epidemiology, work-up, and staging of esophageal cancer 6) Discuss the surgical approach and management of esophageal cancer
Procedure:
Patients who were having Progressive dysphagia, odynophagia, halitosis, unintentional weight loss,chest pain are examined clinically . Routine investigations barium radiology(barium swallow/meal) ,upper gi endoscopy ,histologic diagnosis – biopsy, computed tomography (ct) , bronchoscopy Chest x ray,u s g abdomen,p h manometry were done on the day presentation.
Risks: No life threatening risks involved in the study.
Benefits: Prospective study to compare the incidence of squamous cell carcinoma and adenocarcinoma of oesophaghus in and around Mangalore
Alternatives: Even if you decide not to participate in the study you will receive usual Standard care
Privacy and Confidentiality: The results of the study may be published for scientific purposes and / or to scientific groups. However you will not be identified. Privacy and confidentiality of the study participants will be ensured.
Institutional Policy The A. J. Institute Of Medical Sciences will provide, within the limitations of the laws of the State of Karnataka, facilities and medical attention to subject who suffer injuries as a result of participating in its projects. In the event you believe that you have suffered any physical injury as result of your participation in this study you may contact Principal Investigator Dr.GURUPRASAD RAI D or DR. DEVIDAS SHETTY, Guide.
Financial incentive for participation:
You will not receive any payment for participating in this study.
Authorisation to publish results:
Results of this study may be published for scientific purposes or presented to scientific groups; however you will not be identified. No indefinable information will be used for publication or dissemination of the study finding. Only, DR. DEVIDAS SHETTY, Guide. and Dr.GURUPRASAD RAI D Post graduate student A.J.Institute Of Medical Sciences, Mangalore-04 ,will have access to the data. Contacts:
If you have any question about the research you may please contact Dr. Ramesh Pai, Principal and Chairman of Ethical Committee, A.J.Institute Of Medical Sciences, Mangalore-04. In case of any emergency you may contact, Dr.GURUPRASAD RAI D,Post Graduate Student, Dept Of SURGERY A.J.Institute Of Medical Sciences, Kuntikana ,Mangalore- 04, Telephone no. 9886730726 or DR. DEVIDAS SHETTY, Guide Professor, A.J.institute Of Medical Sciences, Mangalore
Your decision whether or not to participate in the study will not affect the standard care during your current or future relations with the hospital. You are free to discontinue the study at any time and for any reason.
Statement of consent I volunteer and consent to participate in the study. I have read the consent or it has been read to me. The study has been fully explained to me and I may ask questions at any time.
______Signature or left hand thumb impression of Patient Date
______Signature of investigator / designee obtaining informed consent Date
______Signature (Witness) Date
Proforma Name-
Age-
Sex- Doa- Ip no-
Presenting Complaints
History of presenting complaint:
Progressive dysphagia Odynophagia Halitosis Unintentional weight loss Chest pain
History of past illness
HISTORY OF ANY DRUG INTAKE-yes/no IF PRESENT NATURE OF DRUG- PRESENCE OF ANY ASSOCIATED DISEASE-
Family history
Personal History
Place of birth : Educational status: Illiterate: Religion : Appetite : Thirst :. Sleep : Stool : Urine :
Physical examination
Pulse: B P: mm of Hg Temp:
Pallor cyanosis, icteric. clubbing lymphadenopathy pedal oedema
Systemic Examination
Examination of Respiratory system
Examination of central nervous system
Examination of cardio vascular system
Examination of abdomen
Investigations HAEMOGLOBIN –
a) >11gm%
b) 9-11gm%
c) <9gm%
TOTAL LEUCOCYTE COUNT
DIFFERENTIAL LEUCOCYTE COUNT
Neutrophils
Lymphocytes
Eosinophils
Monocytes ERYTHROCYTE SEDIMENTATION RATE :
BLOOD UREA:
SERUM CREATININE :
BARIUM RADIOLOGY(BARIUM SWALLOW/MEAL)
UPPER GI ENDDOSCOPY GROSS LESIONS ON ENDOSCOPY
Polypoid
Ulcerative
Infiltrative
Nodular
Ulcero infiltrative
Other (specify)
ENDOSCOPIC LEVEL OF TUMOR LOCATION FROM INCISOR TEETH Location of tumor(cm) 15-20 21-25 26-30 31-35 36-oesophagogastric junction oesophagogastric junction unknown
HISTOLOGIC DIAGNOSIS – BIOPSY
Pathological reporting Length of oesophagus: mm Length of stomach (maximum): mm Width of tumour: mm Length of tumour: mm Tumour edge to nearest distal margin: mm Tumour edge to nearest proximal margin: Mm Macroscopic type of tumour: Polypoid
Ulcerative
Infiltrative
Nodular
Ulcero infiltrative
Other (specify)
Type of tumour: Squamous
Adenocarcinoma
Other (specify) Differentiation by predominant area: Well
Moderate
Poor Depth of invasion: Tis high grade dysplasia
Tx No tumor identified
T1 invasion of lamina propria/submucosa
T2 invasion of muscularis propria
T3 invasion beyond muscularis propria
T4 invasion of adjacent structures Lymph nodes groups
COMPUTED TOMOGRAPHY (CT)
BRONCHOSCOPY
CHEST X RAY
U S G ABDOMEN
P H MANOMETRY