Phosphate Transporters of the SLC20 and SLC34 Families
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

The Concise Guide to Pharmacology 2019/20
Edinburgh Research Explorer THE CONCISE GUIDE TO PHARMACOLOGY 2019/20 Citation for published version: Cgtp Collaborators 2019, 'THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Transporters', British Journal of Pharmacology, vol. 176 Suppl 1, pp. S397-S493. https://doi.org/10.1111/bph.14753 Digital Object Identifier (DOI): 10.1111/bph.14753 Link: Link to publication record in Edinburgh Research Explorer Document Version: Publisher's PDF, also known as Version of record Published In: British Journal of Pharmacology General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 28. Sep. 2021 S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2019/20: Transporters. British Journal of Pharmacology (2019) 176, S397–S493 THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Transporters Stephen PH Alexander1 , Eamonn Kelly2, Alistair Mathie3 ,JohnAPeters4 , Emma L Veale3 , Jane F Armstrong5 , Elena Faccenda5 ,SimonDHarding5 ,AdamJPawson5 , Joanna L -

Epistasis-Driven Identification of SLC25A51 As a Regulator of Human
ARTICLE https://doi.org/10.1038/s41467-020-19871-x OPEN Epistasis-driven identification of SLC25A51 as a regulator of human mitochondrial NAD import Enrico Girardi 1, Gennaro Agrimi 2, Ulrich Goldmann 1, Giuseppe Fiume1, Sabrina Lindinger1, Vitaly Sedlyarov1, Ismet Srndic1, Bettina Gürtl1, Benedikt Agerer 1, Felix Kartnig1, Pasquale Scarcia 2, Maria Antonietta Di Noia2, Eva Liñeiro1, Manuele Rebsamen1, Tabea Wiedmer 1, Andreas Bergthaler1, ✉ Luigi Palmieri2,3 & Giulio Superti-Furga 1,4 1234567890():,; About a thousand genes in the human genome encode for membrane transporters. Among these, several solute carrier proteins (SLCs), representing the largest group of transporters, are still orphan and lack functional characterization. We reasoned that assessing genetic interactions among SLCs may be an efficient way to obtain functional information allowing their deorphanization. Here we describe a network of strong genetic interactions indicating a contribution to mitochondrial respiration and redox metabolism for SLC25A51/MCART1, an uncharacterized member of the SLC25 family of transporters. Through a combination of metabolomics, genomics and genetics approaches, we demonstrate a role for SLC25A51 as enabler of mitochondrial import of NAD, showcasing the potential of genetic interaction- driven functional gene deorphanization. 1 CeMM Research Center for Molecular Medicine of the Austrian Academy of Sciences, Vienna, Austria. 2 Laboratory of Biochemistry and Molecular Biology, Department of Biosciences, Biotechnologies and Biopharmaceutics, -

Supplementary Table 1
Supplementary Table 1. 492 genes are unique to 0 h post-heat timepoint. The name, p-value, fold change, location and family of each gene are indicated. Genes were filtered for an absolute value log2 ration 1.5 and a significance value of p ≤ 0.05. Symbol p-value Log Gene Name Location Family Ratio ABCA13 1.87E-02 3.292 ATP-binding cassette, sub-family unknown transporter A (ABC1), member 13 ABCB1 1.93E-02 −1.819 ATP-binding cassette, sub-family Plasma transporter B (MDR/TAP), member 1 Membrane ABCC3 2.83E-02 2.016 ATP-binding cassette, sub-family Plasma transporter C (CFTR/MRP), member 3 Membrane ABHD6 7.79E-03 −2.717 abhydrolase domain containing 6 Cytoplasm enzyme ACAT1 4.10E-02 3.009 acetyl-CoA acetyltransferase 1 Cytoplasm enzyme ACBD4 2.66E-03 1.722 acyl-CoA binding domain unknown other containing 4 ACSL5 1.86E-02 −2.876 acyl-CoA synthetase long-chain Cytoplasm enzyme family member 5 ADAM23 3.33E-02 −3.008 ADAM metallopeptidase domain Plasma peptidase 23 Membrane ADAM29 5.58E-03 3.463 ADAM metallopeptidase domain Plasma peptidase 29 Membrane ADAMTS17 2.67E-04 3.051 ADAM metallopeptidase with Extracellular other thrombospondin type 1 motif, 17 Space ADCYAP1R1 1.20E-02 1.848 adenylate cyclase activating Plasma G-protein polypeptide 1 (pituitary) receptor Membrane coupled type I receptor ADH6 (includes 4.02E-02 −1.845 alcohol dehydrogenase 6 (class Cytoplasm enzyme EG:130) V) AHSA2 1.54E-04 −1.6 AHA1, activator of heat shock unknown other 90kDa protein ATPase homolog 2 (yeast) AK5 3.32E-02 1.658 adenylate kinase 5 Cytoplasm kinase AK7 -

Frontiersin.Org 1 April 2015 | Volume 9 | Article 123 Saunders Et Al
ORIGINAL RESEARCH published: 28 April 2015 doi: 10.3389/fnins.2015.00123 Influx mechanisms in the embryonic and adult rat choroid plexus: a transcriptome study Norman R. Saunders 1*, Katarzyna M. Dziegielewska 1, Kjeld Møllgård 2, Mark D. Habgood 1, Matthew J. Wakefield 3, Helen Lindsay 4, Nathalie Stratzielle 5, Jean-Francois Ghersi-Egea 5 and Shane A. Liddelow 1, 6 1 Department of Pharmacology and Therapeutics, University of Melbourne, Parkville, VIC, Australia, 2 Department of Cellular and Molecular Medicine, University of Copenhagen, Copenhagen, Denmark, 3 Walter and Eliza Hall Institute of Medical Research, Parkville, VIC, Australia, 4 Institute of Molecular Life Sciences, University of Zurich, Zurich, Switzerland, 5 Lyon Neuroscience Research Center, INSERM U1028, Centre National de la Recherche Scientifique UMR5292, Université Lyon 1, Lyon, France, 6 Department of Neurobiology, Stanford University, Stanford, CA, USA The transcriptome of embryonic and adult rat lateral ventricular choroid plexus, using a combination of RNA-Sequencing and microarray data, was analyzed by functional groups of influx transporters, particularly solute carrier (SLC) transporters. RNA-Seq Edited by: Joana A. Palha, was performed at embryonic day (E) 15 and adult with additional data obtained at University of Minho, Portugal intermediate ages from microarray analysis. The largest represented functional group Reviewed by: in the embryo was amino acid transporters (twelve) with expression levels 2–98 times Fernanda Marques, University of Minho, Portugal greater than in the adult. In contrast, in the adult only six amino acid transporters Hanspeter Herzel, were up-regulated compared to the embryo and at more modest enrichment levels Humboldt University, Germany (<5-fold enrichment above E15). -

Strand Breaks for P53 Exon 6 and 8 Among Different Time Course of Folate Depletion Or Repletion in the Rectosigmoid Mucosa
SUPPLEMENTAL FIGURE COLON p53 EXONIC STRAND BREAKS DURING FOLATE DEPLETION-REPLETION INTERVENTION Supplemental Figure Legend Strand breaks for p53 exon 6 and 8 among different time course of folate depletion or repletion in the rectosigmoid mucosa. The input of DNA was controlled by GAPDH. The data is shown as ΔCt after normalized to GAPDH. The higher ΔCt the more strand breaks. The P value is shown in the figure. SUPPLEMENT S1 Genes that were significantly UPREGULATED after folate intervention (by unadjusted paired t-test), list is sorted by P value Gene Symbol Nucleotide P VALUE Description OLFM4 NM_006418 0.0000 Homo sapiens differentially expressed in hematopoietic lineages (GW112) mRNA. FMR1NB NM_152578 0.0000 Homo sapiens hypothetical protein FLJ25736 (FLJ25736) mRNA. IFI6 NM_002038 0.0001 Homo sapiens interferon alpha-inducible protein (clone IFI-6-16) (G1P3) transcript variant 1 mRNA. Homo sapiens UDP-N-acetyl-alpha-D-galactosamine:polypeptide N-acetylgalactosaminyltransferase 15 GALNTL5 NM_145292 0.0001 (GALNT15) mRNA. STIM2 NM_020860 0.0001 Homo sapiens stromal interaction molecule 2 (STIM2) mRNA. ZNF645 NM_152577 0.0002 Homo sapiens hypothetical protein FLJ25735 (FLJ25735) mRNA. ATP12A NM_001676 0.0002 Homo sapiens ATPase H+/K+ transporting nongastric alpha polypeptide (ATP12A) mRNA. U1SNRNPBP NM_007020 0.0003 Homo sapiens U1-snRNP binding protein homolog (U1SNRNPBP) transcript variant 1 mRNA. RNF125 NM_017831 0.0004 Homo sapiens ring finger protein 125 (RNF125) mRNA. FMNL1 NM_005892 0.0004 Homo sapiens formin-like (FMNL) mRNA. ISG15 NM_005101 0.0005 Homo sapiens interferon alpha-inducible protein (clone IFI-15K) (G1P2) mRNA. SLC6A14 NM_007231 0.0005 Homo sapiens solute carrier family 6 (neurotransmitter transporter) member 14 (SLC6A14) mRNA. -

Transcriptomic Gene Signatures Associated with Persistent Airflow Limitation
Hekking et al Revised manuscript ERJ-02298-2016 Transcriptomic gene signatures associated with persistent airflow limitation in patients with severe asthma P.P. Hekking1, M.J. Loza2, S. Pavlidis3, B. De Meulder4, D. Lefaudeux4, F. Baribaud2, C. Auffray4, A.H. Wagener1, P. Brinkman1, R. Lutter1, A.T. Bansal5, A.R. Sousa6, S. Bates6, Y. Pandis3, L.J. Fleming3, D.E. Shaw7, S.J. Fowler8, Y. Guo3, A. Meiser3, K. Sun3, J. Corfield9, P. Howarth10, E.H. Bel1, I.M. Adcock11, K.F. Chung11, R. Djukanovic10, P.J. Sterk1, and the U-BIOPRED Study Group* 1: Respiratory Medicine, Academic Medical Centre, Amsterdam, the Netherlands; 2: Janssen research and development; Johnsen & Johnsen, Springhouse, US; 3: Data Science Institute, Imperial College, London, UK; 4: European Institute for Systems Biology and Medicine, CIRI UMR5308, CNRS-ENS- UCBL-INSERM, Université de Lyon, France; 5: Acclarogen Ltd, Cambridge, UK; 6: Discovery Medicine, GlaxoSmithKline, Brentford, UK; 7: Respiratory Research Unit, University of Nottingham, UK; 8: Centre for Respiratory Medicine and Allergy, Institute of Inflammation and Repair, University of Manchester and University Hospital of South Manchester, Manchester Academic Health Sciences Centre, UK; 9: Areteva, Nottingham, UK; 10: NIHR Southampton Centre for Biomedical Research, University of Southampton, UK; 11: National Heart & Lung institute - Imperial College, London, UK;*A list of the U-BIOPRED study group can be found in the online supplement Corresponding author: Pieter-Paul Hekking, Academic Medical Centre (AMC), Department of Respiratory Medicine, F5-260 1105 AZ, Amsterdam, the Netherlands Telephone: +31 (0) 20 566 1660 Fax: +31 (0) 20 566 9001 E-mail: [email protected] 1 Hekking et al Take home message Persistent airflow limitation in severe asthma is associated with a mechanism in which IL-13 and remodeling are involved. -

Impact of SLC20A1 on the Wnt/Β‑Catenin Signaling Pathway in Somatotroph Adenomas
3276 MOLECULAR MEDICINE REPORTS 20: 3276-3284, 2019 Impact of SLC20A1 on the Wnt/β‑catenin signaling pathway in somatotroph adenomas JIANHUA LI1,2, WEI DONG3, ZHENYE LI4, HONGYUN WANG1, HUA GAO1 and YAZHUO ZHANG1,4 1Key Laboratory of Central Nervous System Injury Research, Beijing Neurosurgical Institute, Capital Medical University, Beijing 100070; 2Department of Neurosurgery, Binzhou People's Hospital, Binzhou, Shandong 256610; 3Department of Neurosurgery, Tangshan People's Hospital, Tangshan, Hebei 063001; 4Beijing Tiantan Hospital, Capital Medical University, Beijing 100070, P.R. China Received February 5, 2019; Accepted July 12, 2019 DOI: 10.3892/mmr.2019.10555 Abstract. Studies have revealed that genetic and functional was 86.4±5.7, 75.6±4.4 and 67.5±3.8%, respectively (P<0.05). aberrations of oncogenes, tumor-suppressor genes, signaling ELISA analysis demonstrated the growth hormone (GH) pathways and receptors are among the most prominent events levels in the Sh-B-SLC20A1 and Sh‑C‑SLC20A1 groups to be in pituitary tumorigenesis, and a potent biomarker would 34.7±10.4 and 54.6±14.4%, respectively, of that of control GH3 be helpful for early diagnosis, subsequent treatment and cells (P<0.05). The transmembrane invasion assay revealed that disease control. The present study investigated the expression knocking down SLC20A1 significantly suppressed cell invasion signatures of solute carrier family 20 member 1, also known in the Sh-B-SLC20A1 and Sh‑C‑SLC20A1 groups. RT-qPCR as phosphate transporter 1 (SLC20A1) and the Wnt/β-catenin and western blotting demonstrated that Sh-B-SLC20A1 and signaling pathway in 52 patients with somatotroph adenomas. -

1.18 Thesis Hypothesis 70 1.19 Thesis Aims and Structure 72
COLLEGE OF MEDICINE, BIOLOGICAL SCIENCES AND PSYCHOLOGY SCHOOL OF MEDICINE DEPARTMENT OF INFECTION, IMMUNITY & INFLAMMATION Microparticles as biomarkers of early changes leading to Cardiovascular disease in chronic kidney disease © Nima Abbasian This thesis submitted for the degree of Doctor of Philosophy at the University of Leicester- 2015 Abstract Microparticles as biomarkers of early changes leading to cardiovascular disease in chronic kidney disease Nima Abbasian Hyperphosphataemia in patients with advanced chronic kidney disease (CKD) is thought to be an important contributor to cardiovascular risk, in part because of endothelial cell (EC) dysfunction induced by inorganic phosphate (Pi). Such patients also have an elevated circulating concentration of pro-coagulant endothelial microparticles (MPs), leading to a pro-thrombotic state, which may contribute to acute occlusive events. It is hypothesised that hyperphosphataemia leads to MP formation from ECs via an elevation of intracellular Pi, which directly inhibits phosphoprotein phosphatases, triggering a global increase in phosphorylation and cytoskeletal changes. Using cultured human endothelial cells (EAhy926), incubation with elevated extracellular Pi (2.5mM) led to a rise in intracellular Pi concentration within 90min. This was mediated by PiT-1/slc20a1 Pi transporters; and led to global accumulation of Tyr- and Ser-Thr phosphorylated proteins, a marked increase in cellular Tropomyosin-3, plasma membrane blebbing and release of 0.1 – 1 micron diameter MPs. The effect of Pi was independent of oxidative stress or apoptosis. Similarly, global inhibition of phosphoprotein phosphatases with orthovandate or fluoride also yielded a global protein phosphorylation response and rapid release of MPs. The Pi-induced MPs expressed VE-cadherin and superficial phosphatidylserine, and in a thrombin generation assay were significantly more pro-coagulant than particles derived from cells incubated in medium with a physiological level of Pi (1mM). -
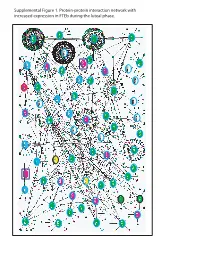
Supplemental Figure 1. Protein-Protein Interaction Network with Increased Expression in Fteb During the Luteal Phase
Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during luteal phase. LEGENDS TO SUPPLEMENTAL FIGURES Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with increased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. Genes encoding proteins shown as large ovals highlighted in blue were exclusively found in the first comparison (Manuscript Figure 2), whereas those highlighted in red were only found in the second comparison (Manuscript Figure 3). Genes encoding proteins shown as large ovals highlighted in black were found in both comparisons. The color of each node indicates the ontology of the corresponding protein as determined by the Online Predicted Human Interaction Database (OPHID) link with the NAViGaTOR software. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with decreased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. -

The Concise Guide to Pharmacology 2019/20: Transporters
University of Dundee The Concise Guide to Pharmacology 2019/20 CGTP Collaborators; Alexander, Stephen P. H.; Kelly, Eamonn; Mathie, Alistair; Peters, John A.; Veale, Emma L. Published in: British Journal of Pharmacology DOI: 10.1111/bph.14753 Publication date: 2019 Document Version Publisher's PDF, also known as Version of record Link to publication in Discovery Research Portal Citation for published version (APA): CGTP Collaborators, Alexander, S. P. H., Kelly, E., Mathie, A., Peters, J. A., Veale, E. L., ... Davies, J. A. (2019). The Concise Guide to Pharmacology 2019/20: Transporters. British Journal of Pharmacology, 176 (S1), S397- S493. https://doi.org/10.1111/bph.14753 General rights Copyright and moral rights for the publications made accessible in Discovery Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from Discovery Research Portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain. • You may freely distribute the URL identifying the publication in the public portal. Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Download date: 07. Dec. 2019 S.P.H. Alexander et al. The Concise -

Expression of Intestinal Transporter Genes in Beagle Dogs
308 EXPERIMENTAL AND THERAPEUTIC MEDICINE 5: 308-314, 2013 Expression of intestinal transporter genes in beagle dogs SOO-MIN CHO1*, SUNG-WON PARK1,2*, NA‑HYUN KIM1, JIN-A PARK1, HEE YI1, HEE-JUNG CHO1, KI-HWAN PARK3, INGYUN HWANG4 and HO-CHUL SHIN1 1Department of Veterinary Pharmacology and Toxicology, College of Veterinary Medicine, Konkuk University, Seoul 143‑701; 2Toxicology and Chemistry Division, Animal Plant and Fisheries Quarantine and Inspection Agency, Anyang 430‑824; 3Department of Food Science & Technology, Chung‑Ang University, Ansung 456‑756; 4Food Chemical Residues Division, Korea Food & Drug Administration, Osong 363-951, Republic of Korea Received August 8, 2012; Accepted October 12, 2012 DOI: 10.3892/etm.2012.777 Abstract. This study was performed to produce a transcrip- 5% of all human genes are associated with transporters which tional database of the intestinal transporters of beagle dogs. is consistent with the biological significance of transporters Total RNA was isolated from the duodenum and the expres- and their roles in cell homeostasis. The identification and sion of various mRNAs was measured using GeneChip® characterization of drug transporters has provided a scientific oligonucleotide arrays. A total of 124 transporter genes were basis for understanding drug delivery and disposition, the detected. Genes for fatty acid, peptide, amino acid and glucose molecular mechanisms of drug interactions and inter‑indi- and multidrug resistance/multidrug resistance-associated vidual/inter‑species differences (3). Various types of xenobiotic protein (MDR/MRP) transport were expressed at relatively or drug transporters have been identified as being important higher levels than the other transporter types. The dogs exhib- as barriers against toxic compounds and influx pumps to take ited abundant mRNA expression of the fatty acid transporters up nutrients into the body.