(Q36.1;Q24) with a Concurrent Submicroscopic Del(4)(Q23q24) in an Adult with Polycythemia Vera
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Single Nucleotide Polymorphisms Within Calcineurin-Encoding Genes
Annals of Applied Sport Science, vol. 4, no. 2, pp. 01-08, Summer 2016 DOI: 10.18869/acadpub.aassjournal.4.2.1 Original Article www.aassjournal.com www.AESAsport.com ISSN (Online): 2322 – 4479 Received: 06/03/2016 ISSN (Print): 2476–4981 Accepted: 26/06/2016 Single Nucleotide Polymorphisms within Calcineurin-Encoding Genes are Associated with Response to Aerobic Training in Han Chinese Males 1Rong-mei Xu, 2Tao Lu, 2Lingxian Yan, 1Qinghua Song* 1The Center of Physical Health, Henan Polytechnic University, Jiaozuo 454000, Henan Province, China. 2 The Lab of Human Body Science, Henan Polytechnic University, Jiaozuo 454000, Henan Province, China. ABSTRACT Calcineurin, which functions in calcium signaling, is expressed in skeletal and cardiac muscle and has been linked to sensitivity to muscle strength training. It is also proposed to contribute to individual aerobic endurance. To investigate the relationship between calcineurin-encoding genes and aerobic endurance traits, 126 young-adult Han Chinese males were enrolled in an aerobic exercise training study. Participants were genotyped for polymorphisms within the 5 genes (PPP3CA, PPP3CB, PPP3CC, PPP3R1 and PPP3R2) encoding calcineurin using restriction fragment length polymorphism polymerase chain reaction (PCR-RFLP) or matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS). Participants underwent 18 weeks of aerobic exercise training (running). Before and after the training period, maximal oxygen uptake (VO2max) and 12 km/h running economy were measured. Statistical analyses were performed using chi-square test and analysis of variance. The baseline value of VO2max was significantly associated with rs3804423 and rs2850965 loci in the PPP3CA gene (P<0.05). -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Long, Noncoding RNA Dysregulation in Glioblastoma
cancers Review Long, Noncoding RNA Dysregulation in Glioblastoma Patrick A. DeSouza 1,2 , Xuan Qu 1, Hao Chen 1,3, Bhuvic Patel 1 , Christopher A. Maher 2,4,5,6 and Albert H. Kim 1,6,* 1 Department of Neurological Surgery, Washington University School of Medicine in St. Louis, St. Louis, MO 63110, USA; [email protected] (P.A.D.); [email protected] (X.Q.); [email protected] (H.C.); [email protected] (B.P.) 2 Department of Internal Medicine, Washington University School of Medicine in St. Louis, St. Louis, MO 63110, USA; [email protected] 3 Department of Neuroscience, Washington University School of Medicine in St. Louis, St. Louis, MO 63110, USA 4 Department of Biomedical Engineering, Washington University School of Medicine in St. Louis, St. Louis, MO 63110, USA 5 McDonnell Genome Institute, Washington University School of Medicine in St. Louis, St. Louis, MO 63110, USA 6 Siteman Cancer Center, Washington University School of Medicine in St. Louis, St. Louis, MO 63110, USA * Correspondence: [email protected] Simple Summary: Developing effective therapies for glioblastoma (GBM), the most common primary brain cancer, remains challenging due to the heterogeneity within tumors and therapeutic resistance that drives recurrence. Noncoding RNAs are transcribed from a large proportion of the genome and remain largely unexplored in their contribution to the evolution of GBM tumors. Here, we will review the general mechanisms of long, noncoding RNAs and the current knowledge of how these impact heterogeneity and therapeutic resistance in GBM. A better understanding of the molecular drivers required for these aggressive tumors is necessary to improve the management and outcomes Citation: DeSouza, P.A.; Qu, X.; of this challenging disease. -

Cellular and Molecular Signatures in the Disease Tissue of Early
Cellular and Molecular Signatures in the Disease Tissue of Early Rheumatoid Arthritis Stratify Clinical Response to csDMARD-Therapy and Predict Radiographic Progression Frances Humby1,* Myles Lewis1,* Nandhini Ramamoorthi2, Jason Hackney3, Michael Barnes1, Michele Bombardieri1, Francesca Setiadi2, Stephen Kelly1, Fabiola Bene1, Maria di Cicco1, Sudeh Riahi1, Vidalba Rocher-Ros1, Nora Ng1, Ilias Lazorou1, Rebecca E. Hands1, Desiree van der Heijde4, Robert Landewé5, Annette van der Helm-van Mil4, Alberto Cauli6, Iain B. McInnes7, Christopher D. Buckley8, Ernest Choy9, Peter Taylor10, Michael J. Townsend2 & Costantino Pitzalis1 1Centre for Experimental Medicine and Rheumatology, William Harvey Research Institute, Barts and The London School of Medicine and Dentistry, Queen Mary University of London, Charterhouse Square, London EC1M 6BQ, UK. Departments of 2Biomarker Discovery OMNI, 3Bioinformatics and Computational Biology, Genentech Research and Early Development, South San Francisco, California 94080 USA 4Department of Rheumatology, Leiden University Medical Center, The Netherlands 5Department of Clinical Immunology & Rheumatology, Amsterdam Rheumatology & Immunology Center, Amsterdam, The Netherlands 6Rheumatology Unit, Department of Medical Sciences, Policlinico of the University of Cagliari, Cagliari, Italy 7Institute of Infection, Immunity and Inflammation, University of Glasgow, Glasgow G12 8TA, UK 8Rheumatology Research Group, Institute of Inflammation and Ageing (IIA), University of Birmingham, Birmingham B15 2WB, UK 9Institute of -

Protein Interactions in the Cancer Proteome† Cite This: Mol
Molecular BioSystems View Article Online PAPER View Journal | View Issue Small-molecule binding sites to explore protein– protein interactions in the cancer proteome† Cite this: Mol. BioSyst., 2016, 12,3067 David Xu,ab Shadia I. Jalal,c George W. Sledge Jr.d and Samy O. Meroueh*aef The Cancer Genome Atlas (TCGA) offers an unprecedented opportunity to identify small-molecule binding sites on proteins with overexpressed mRNA levels that correlate with poor survival. Here, we analyze RNA-seq and clinical data for 10 tumor types to identify genes that are both overexpressed and correlate with patient survival. Protein products of these genes were scanned for binding sites that possess shape and physicochemical properties that can accommodate small-molecule probes or therapeutic agents (druggable). These binding sites were classified as enzyme active sites (ENZ), protein–protein interaction sites (PPI), or other sites whose function is unknown (OTH). Interestingly, the overwhelming majority of binding sites were classified as OTH. We find that ENZ, PPI, and OTH binding sites often occurred on the same structure suggesting that many of these OTH cavities can be used for allosteric modulation of Creative Commons Attribution 3.0 Unported Licence. enzyme activity or protein–protein interactions with small molecules. We discovered several ENZ (PYCR1, QPRT,andHSPA6)andPPI(CASC5, ZBTB32,andCSAD) binding sites on proteins that have been seldom explored in cancer. We also found proteins that have been extensively studied in cancer that have not been previously explored with small molecules that harbor ENZ (PKMYT1, STEAP3,andNNMT) and PPI (HNF4A, MEF2B,andCBX2) binding sites. All binding sites were classified by the signaling pathways to Received 29th March 2016, which the protein that harbors them belongs using KEGG. -

Variation in Protein Coding Genes Identifies Information
bioRxiv preprint doi: https://doi.org/10.1101/679456; this version posted June 21, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Animal complexity and information flow 1 1 2 3 4 5 Variation in protein coding genes identifies information flow as a contributor to 6 animal complexity 7 8 Jack Dean, Daniela Lopes Cardoso and Colin Sharpe* 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Institute of Biological and Biomedical Sciences 25 School of Biological Science 26 University of Portsmouth, 27 Portsmouth, UK 28 PO16 7YH 29 30 * Author for correspondence 31 [email protected] 32 33 Orcid numbers: 34 DLC: 0000-0003-2683-1745 35 CS: 0000-0002-5022-0840 36 37 38 39 40 41 42 43 44 45 46 47 48 49 Abstract bioRxiv preprint doi: https://doi.org/10.1101/679456; this version posted June 21, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Animal complexity and information flow 2 1 Across the metazoans there is a trend towards greater organismal complexity. How 2 complexity is generated, however, is uncertain. Since C.elegans and humans have 3 approximately the same number of genes, the explanation will depend on how genes are 4 used, rather than their absolute number. -
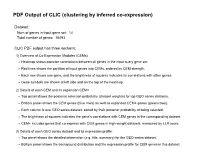
PDF Output of CLIC (Clustering by Inferred Co-Expression)
PDF Output of CLIC (clustering by inferred co-expression) Dataset: Num of genes in input gene set: 14 Total number of genes: 16493 CLIC PDF output has three sections: 1) Overview of Co-Expression Modules (CEMs) Heatmap shows pairwise correlations between all genes in the input query gene set. Red lines shows the partition of input genes into CEMs, ordered by CEM strength. Each row shows one gene, and the brightness of squares indicates its correlations with other genes. Gene symbols are shown at left side and on the top of the heatmap. 2) Details of each CEM and its expansion CEM+ Top panel shows the posterior selection probability (dataset weights) for top GEO series datasets. Bottom panel shows the CEM genes (blue rows) as well as expanded CEM+ genes (green rows). Each column is one GEO series dataset, sorted by their posterior probability of being selected. The brightness of squares indicates the gene's correlations with CEM genes in the corresponding dataset. CEM+ includes genes that co-express with CEM genes in high-weight datasets, measured by LLR score. 3) Details of each GEO series dataset and its expression profile: Top panel shows the detailed information (e.g. title, summary) for the GEO series dataset. Bottom panel shows the background distribution and the expression profile for CEM genes in this dataset. Overview of Co-Expression Modules (CEMs) with Dataset Weighting Scale of average Pearson correlations Num of Genes in Query Geneset: 14. Num of CEMs: 1. 0.0 0.2 0.4 0.6 0.8 1.0 Cpsf3l Polr2b Ints3 Ints7 Ints1 Ints4 Ints9 Ints2 -

Aneuploidy: Using Genetic Instability to Preserve a Haploid Genome?
Health Science Campus FINAL APPROVAL OF DISSERTATION Doctor of Philosophy in Biomedical Science (Cancer Biology) Aneuploidy: Using genetic instability to preserve a haploid genome? Submitted by: Ramona Ramdath In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Science Examination Committee Signature/Date Major Advisor: David Allison, M.D., Ph.D. Academic James Trempe, Ph.D. Advisory Committee: David Giovanucci, Ph.D. Randall Ruch, Ph.D. Ronald Mellgren, Ph.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: April 10, 2009 Aneuploidy: Using genetic instability to preserve a haploid genome? Ramona Ramdath University of Toledo, Health Science Campus 2009 Dedication I dedicate this dissertation to my grandfather who died of lung cancer two years ago, but who always instilled in us the value and importance of education. And to my mom and sister, both of whom have been pillars of support and stimulating conversations. To my sister, Rehanna, especially- I hope this inspires you to achieve all that you want to in life, academically and otherwise. ii Acknowledgements As we go through these academic journeys, there are so many along the way that make an impact not only on our work, but on our lives as well, and I would like to say a heartfelt thank you to all of those people: My Committee members- Dr. James Trempe, Dr. David Giovanucchi, Dr. Ronald Mellgren and Dr. Randall Ruch for their guidance, suggestions, support and confidence in me. My major advisor- Dr. David Allison, for his constructive criticism and positive reinforcement. -

Evolution of Vertebrate Solute Carrier Family 9B
etics & E en vo g lu t lo i y o h n a P r f y Journal of Phylogenetics & Holmes et al., J Phylogen Evolution Biol 2016, 4:3 o B l i a o n l r o DOI: 10.4172/2329-9002.1000167 u g o y J Evolutionary Biology ISSN: 2329-9002 Research Article Open Access Evolution of Vertebrate Solute Carrier Family 9B Genes and Proteins (SLC9B): Evidence for a Marsupial Origin for Testis Specific SLC9B1 from an Ancestral Vertebrate SLC9B2 Gene Roger S Holmes1*,2, Kimberly D Spradling-Reeves2 and Laura A Cox2 1Eskitis Institute for Drug Discovery and School of Natural Sciences, Griffith University, Nathan, QLD, Australia 2Department of Genetics and Southwest National Primate Research Center, Texas Biomedical Research Institute, San Antonio, Texas, USA Abstract SLC9B genes and proteins are members of the sodium/lithium hydrogen antiporter family which function as solute exchangers within cellular membranes of mammalian tissues. SLC9B2 and SLC9B1 amino acid sequences and structures and SLC9B-like gene locations were examined using bioinformatic data from several vertebrate genome projects. Vertebrate SLC9B2 sequences shared 56-98% identity as compared with ~50% identities with mammalian SLC9B1 sequences. Sequence alignments, key amino acid residues and conserved predicted transmembrane structures were also studied. Mammalian SLC9B2 and SLC9B1 genes usually contained 11 or 12 coding exons with differential tissue expression patterns: SLC9B2, broad tissue distribution; and SLC9B1, being testis specific. Transcription factor binding sites and CpG islands within the human SLC9B2 and SLC9B1 gene promoters were identified. Phylogenetic analyses suggested thatSLC9B1 originated in an ancestral marsupial genome from a SLC9B2 gene duplication event. -

Calcineurin a (PPP3CA) (NM 000944) Human Tagged ORF Clone Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for RC219136 Calcineurin A (PPP3CA) (NM_000944) Human Tagged ORF Clone Product data: Product Type: Expression Plasmids Product Name: Calcineurin A (PPP3CA) (NM_000944) Human Tagged ORF Clone Tag: Myc-DDK Symbol: PPP3CA Synonyms: ACCIID; CALN; CALNA; CALNA1; CCN1; CNA1; IECEE; IECEE1; PPP2B Vector: pCMV6-Entry (PS100001) E. coli Selection: Kanamycin (25 ug/mL) Cell Selection: Neomycin This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 5 Calcineurin A (PPP3CA) (NM_000944) Human Tagged ORF Clone – RC219136 ORF Nucleotide >RC219136 representing NM_000944 Sequence: Red=Cloning site Blue=ORF Green=Tags(s) TTTTGTAATACGACTCACTATAGGGCGGCCGGGAATTCGTCGACTGGATCCGGTACCGAGGAGATCTGCC GCCGCGATCGCC ATGTCCGAGCCCAAGGCAATTGATCCCAAGTTGTCGACGACCGACAGGGTGGTGAAAGCTGTTCCATTTC CTCCAAGTCACCGGCTTACAGCAAAAGAAGTGTTTGATAATGATGGAAAACCTCGTGTGGATATCTTAAA GGCGCATCTTATGAAGGAGGGAAGGCTGGAAGAGAGTGTTGCATTGAGAATAATAACAGAGGGTGCATCA ATTCTTCGACAGGAAAAAAATTTGCTGGATATTGATGCGCCAGTCACTGTTTGTGGGGACATTCATGGAC AATTCTTTGATTTGATGAAGCTCTTTGAAGTCGGGGGATCTCCTGCCAACACTCGCTACCTCTTCTTAGG GGACTATGTTGACAGAGGGTACTTCAGTATTGAATGTGTGCTGTATTTGTGGGCCTTGAAAATTCTCTAC CCCAAAACACTGTTTTTACTTCGTGGAAATCATGAATGTAGACATCTAACAGAGTATTTCACATTTAAAC AAGAATGTAAAATAAAGTATTCAGAACGCGTATATGATGCCTGTATGGATGCCTTTGACTGCCTTCCCCT -

Anti-PPP3CA (Aa 1-84) Polyclonal Antibody (DPAB- DC2401) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-PPP3CA (aa 1-84) polyclonal antibody (DPAB- DC2401) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description PPP3CA (protein phosphatase 3, catalytic subunit, alpha isozyme) is a protein-coding gene. Diseases associated with PPP3CA include osteomyelitis, and down syndrome critical region, and among its related super-pathways are Fc epsilon RI signaling pathway and BCR signaling pathway. GO annotations related to this gene include enzyme binding and calcium ion binding. An important paralog of this gene is PPP3CC. Immunogen PPP3CA (NP_000935, 1 a.a. ~ 84 a.a) partial recombinant protein with GST tag. The sequence is MSEPKAIDPKLSTTDRVVKAVPFPPSHRLTAKEVFDNDGKPRVDILKAHLMKEGRLEESVALRIIT EGASILRQEKNLLDIDAP Source/Host Mouse Species Reactivity Human Conjugate Unconjugated Applications WB (Cell lysate), WB (Recombinant protein), ELISA, Size 50 μl Buffer 50 % glycerol Preservative None Storage Store at -20°C or lower. Aliquot to avoid repeated freezing and thawing. GENE INFORMATION Gene Name PPP3CA protein phosphatase 3, catalytic subunit, alpha isozyme [ Homo sapiens (human) ] Official Symbol PPP3CA Synonyms PPP3CA; protein phosphatase 3, catalytic subunit, alpha isozyme; CALN; CCN1; CNA1; CALNA; PPP2B; CALNA1; serine/threonine-protein phosphatase 2B catalytic subunit alpha isoform; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved calcineurin A alpha; CAM-PRP catalytic -

PHF22 (INTS12) (NM 020395) Human Over-Expression Lysate Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for LC412498 PHF22 (INTS12) (NM_020395) Human Over-expression Lysate Product data: Product Type: Over-expression Lysates Description: INTS12 HEK293T cell transient overexpression lysate (as WB positive control) Species: Human Expression Host: HEK293T Expression cDNA Clone TrueORF Clone RC204838 or AA Sequence: Tag: C-Myc/DDK Detection Antibodies: Clone OTI4C5, Anti-DDK (FLAG) monoclonal antibody (TA50011-100) Accession Number: NM_020395, NP_065128 Synonyms: INT12; PHF22; SBBI22 Predicted MW: 48.8 kDa Components: 1 vial of 20 ug lyophilized gene specific transient over-expression cell lysate Storage: The lysate can be shipped at ambient temperature. Upon receiving, store the sample at - 20°C. Lysate samples can be reconstituted with SDS Sample Buffer. Avoid repeated freeze- thaw cycles after reconstitution. Lysate samples are stable for 12 months from date of receipt when stored at -20°C. Preparation: HEK293T cells in 10-cm dishes were transiently transfected withM egaTran Transfection Reagent (TT200002) and 5ug TrueORF cDNA plasmid. Transfected cells were cultured for 48hrs before collection. The cells were lysed in modified RIPA buffer (25mM Tris-HCl pH7.6, 150mM NaCl, 1% NP-40, 1mM EDTA, 1xProteinase inhibitor cocktail mix (Sigma), 1mM PMSF and 1mM Na3VO4), and then centrifuged to clarify the lysate. Protein concentration was measured by BCA kit (Thermo Scientific Inc.). To facilitate transportation and protein, the products are supplied as lyophilized proteins. RefSeq: NP_065128 Locus ID: 57117 Cytogenetics: 4q24 Protein Families: Druggable Genome, Transcription Factors This product is to be used for laboratory only.