Patellofemoral SMCA 2014 Handout
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
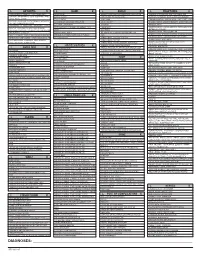
ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -
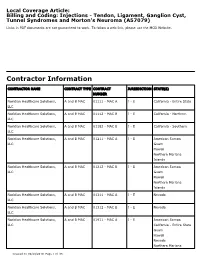
Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079)
Local Coverage Article: Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, A and B MAC 01111 - MAC A J - E California - Entire State LLC Noridian Healthcare Solutions, A and B MAC 01112 - MAC B J - E California - Northern LLC Noridian Healthcare Solutions, A and B MAC 01182 - MAC B J - E California - Southern LLC Noridian Healthcare Solutions, A and B MAC 01211 - MAC A J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01212 - MAC B J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01311 - MAC A J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01312 - MAC B J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01911 - MAC A J - E American Samoa LLC California - Entire State Guam Hawaii Nevada Northern Mariana Created on 09/28/2019. Page 1 of 33 CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Islands Article Information General Information Original Effective Date 10/01/2019 Article ID Revision Effective Date A57079 N/A Article Title Revision Ending Date Billing and Coding: Injections - Tendon, Ligament, N/A Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma Retirement Date N/A Article Type Billing and Coding AMA CPT / ADA CDT / AHA NUBC Copyright Statement CPT codes, descriptions and other data only are copyright 2018 American Medical Association. -

Plica: Pathologic Or Not? J
Plica: Pathologic or Not? J. Whit Ewing, MD Abstract A fold that occurs within a joint is referred to as a plica synovialis. Three such pli- in which the only finding to explain cae are seen with regularity within the human knee joint. These folds are normal the symptoms is the presence of a structures that represent remnants of mesenchymal tissue and/or septa formed thickened, hypertrophic plica. during embryonic development of the knee joint, and can be seen during arthro- Chronic anteromedial knee pain and scopic inspection of the knee joint. Controversy exists within the orthopaedic com- a sense of tightness in the subpatellar munity as to whether a plica can develop pathologic changes sufficient to cause region on squatting are the common disabling knee symptoms. The author defines the clinical syndrome, describes the complaints expressed by patients arthroscopic appearance of pathologic plica, and outlines nonsurgical and surgi- found to have a pathologic plica. The cal methods of management of this uncommon condition. ligamentum mucosum is not a J Am Acad Orthop Surg 1993;1:117-121 source of these types of symptoms. Additional symptoms are snapping sensations, buckling, knee pain on A plica synovialis is a membranous commonly referred to as a medial shelf sitting, and pain with repetitive fold or ridge found in the synovial or medial plica. This shelflike fold of activity.4 Recurrent effusions and lining of a joint. Three such folds are synovial membrane extends from the locking of the knee joint are not typi- found with regularity in the human infrapatellar fat pad to the medial wall cal in patients with this syndrome. -

Diagnosing & Treating Non-Traumatic Knee Pain
ORTHOPEDIC PRIMARY CARE: Diagnosing & Treating Non-Traumatic Knee Pain © Jackson Orthopaedic Foundation www.jacksonortho.org Acknowledgement This lecture was originally developed as part of Orthopedic Primary Care, a six-month continuing education program presented yearly by the Jackson Orthopaedic Foundation, a non-profit organization in Oakland, California. More information at: OrthoPrimaryCare.Info www.jacksonortho.org Disclosure Statement of Unapproved/Investigative Use • This presentation contains no discussion of the unapproved/investigative use of any commercial product or device. www.jacksonortho.org Disclosure Statement of Financial Interest Neither Dr. Benham nor Dr. Geier has any financial interests/arrangements or affiliations with one or more organizations that could be perceived to have real or apparent conflicts of interest in the context of the subject of this presentation. www.jacksonortho.org Learning Objectives • At the conclusion of this presentation, participants will be able to 1. Identify likely causes of non-traumatic, non-arthritic knee pain based on presentation and history. 2. Appropriately apply specialty exam techniques and order diagnostic imaging as needed to definitively diagnose non-traumatic, non-arthritic knee pain. 3. Implement appropriate treatment plans to include integrative and pharmaceutical modalities. The use and effects of the following pharmaceutical types will be discussed: acetaminophen, NSAIDs, injectable corticosteroids and topical analgesics. www.jacksonortho.org Learning Objectives • At the conclusion of this presentation, participants will be able to 1. Identify likely causes of non-traumatic, non-arthritic knee pain based on presentation and history. 2. Appropriately apply specialty exam techniques and order diagnostic imaging as needed to definitively diagnose non-traumatic, non-arthritic knee pain. -

Nontraumatic Knee Pain: Hawks, MD Nellis Family Medicine Residency Program, a Diagnostic & Treatment Guide Nellis Air Force Base, Nev (Drs
Carlton J. Covey, MD, FAAFP; Matthew K. Nontraumatic knee pain: Hawks, MD Nellis Family Medicine Residency Program, A diagnostic & treatment guide Nellis Air Force Base, Nev (Drs. Covey and Hawks); Uniformed Services University of the Health Little has been written about nontraumatic nonarthritic Sciences, Bethesda, Md knee pain in adults. This article seeks to fill that void with (Dr. Covey) practical tips and an at-a-glance resource. [email protected] The authors reported no potential conflict of interest relevant to this article. The opinions and assertions CASE u Jane T, age 42, comes to see you because of right knee contained herein are the Practice pain that she’s had for about 6 months. She denies any trau- private views of the authors and are not to be construed recommendationS ma. ms. T describes the pain as vague and poorly localized, as official or as reflecting the views of the US Air Force › Consider radiography for but worse with activity. She says she started a walking/running Medical Department or the a patient with patellofemoral program 9 months ago, when she was told she was overweight US Air Force at large. pain syndrome if (body mass index, 29). She has lost 10 pounds since then, ms. T examination reveals an says, and hopes to lose more by continuing to exercise. upon effusion, the patient is age further review, you find that ms. T has had increasing pain 50 years or older, or the while ascending and descending stairs and that the pain is also condition does not improve exacerbated when she stands after prolonged sitting. -

Medial Abrasion Syndrome: a Neglected Cause of Knee Pain in Middle and Old Age Shaw-Ruey Lyu, MD, Phd, Ching-Chih Lee, MD, Phd, and Chia-Chen Hsu, MD
Medial Abrasion Syndrome: A Neglected Cause of Knee Pain in Middle and Old Age Shaw-Ruey Lyu, MD, PhD, Ching-Chih Lee, MD, PhD, and Chia-Chen Hsu, MD Abstract: Knee pain is a prevailing health problem of middle and old INTRODUCTION age. Medial plica-related medial abrasion syndrome (MAS), although a hronic knee pain is a prevalent health problem of middle 1 well-known cause of knee pain in younger individuals, has rarely been C and old age. It has been found to be significantly associ- investigated in older individuals. This prospective study was conducted ated with lower quality of life and is a major public health 2–4 to investigate the prevalence and clinical manifestations of this syn- issue. Effective prevention and early treatment of knee pain drome as a cause of knee pain in middle and old age. The outcomes of at these ages has a major influence on healthy aging in the 5 arthroscopic treatment for this syndrome were also evaluated. population. In the younger population, knee pain can have A total of 232 knees of 169 patients >40 years of age (41–82, many possible causes, with medial plica syndrome always 6 median: 63 years old) suffering from chronic knee pain were analyzed. mentioned in the differential diagnosis ; in contrast, osteoar- The clinical diagnosis, predisposing factors, presenting symptoms, and thritis (OA) is regarded as the most common cause of knee pain physical signs were investigated. The sensitivity and specificity of each in middle-aged and older people in addition to trauma-related parameter of the clinical presentation for the diagnosis of MAS were conditions, such as meniscus and/or ligament injury, crystal- evaluated after confirmation by arthroscopy. -

Essentials of Musculoskeletal Care 5 © 2016 American Academy of Orthopaedic Surgeons SECTION 6 Knee and Lower Leg
PAIN DIAGRAM Knee and Lower Leg Osteoarthritis of the hip and thigh Iliotibial band syndrome (see Hip and Patellofemoral instability Thigh section) Osteochondritis dissecans (see Pediatric Orthopaedics section) Fracture (intercondylar) Plica syndrome Collateral ligament Collateral ligament tear (LCL) tear (MCL) Osteonecrosis of the Patellofemoral pain Lateral femoral condyle Patellar fracture Meniscal tear Medial (lateral) Meniscal tear Patellar tendinitis (medial) Patellar tendon rupture Fracture Anterior (tibial plateau) Bursitis Lateral (prepatellar) Quadriceps tendon rupture Quadriceps tendinitis Distal femoral fracture Tibiofemoral fracture (Fractures About the Knee) Collateral ligament tear (MCL) Lateral Medial Popliteal cyst Meniscal tear (medial) Arthritis Bursitis Medial gastrocnemius (pes anserine bursitis) tear Medial Posterior 640 Essentials of Musculoskeletal Care 5 © 2016 American Academy of Orthopaedic Surgeons SECTION 6 Knee and Lower Leg 640 Pain Diagram 686 Bursitis of the Knee 715 Home Exercise 739 Patellofemoral Pain 642 Anatomy 690 Procedure: Pes Program for Medial 743 Home Exercise Gastrocnemius Tear Program for 643 Overview of the Knee Anserine Bursa and Lower Leg Injection 717 Meniscal Tear Patellofemoral Pain Plica Syndrome 651 Home Exercise 692 Claudication 722 Home Exercise 746 Program for Knee 694 Collateral Ligament Program for Meniscal 749 Home Exercise Conditioning Tear Tear Program for Plica Syndrome 657 Physical Examination 698 Home Exercise 724 Osteonecrosis of the of the Knee and Program for Collateral -

Nontraumatic Knee Pain a Diagnostic & Treatment Guide Carlton J
Nontraumatic Knee Pain A Diagnostic & Treatment Guide Carlton J. Covey, MD, FAAFP, Matthew K. Hawks, MD Little has been written about nontraumatic nonarthritic knee pain in adults. This article fills that void with practical tips and an at-a-glance resource. prActice Jane, age 42, presents with right knee pain that she’s had for about recommendAtionS six months. She denies any trauma. Jane describes the pain as “vague • Consider radiography for a and poorly localized” but worse with activity. She says she started a patient with patellofemoral pain walking/running program nine months ago, when she was told she syndrome if examination reveals was overweight (BMI, 29). She has lost 10 pounds since then and an effusion, the patient is age 50 hopes to lose more by continuing to exercise. Further review reveals or older, or the condition does not that Jane has experienced increasing pain while ascending and de- improve after eight to 12 weeks of scending stairs and that the pain is also exacerbated when she stands treatment. C after prolonged sitting. • Order plain radiography for all If Jane were your patient, what would you include in a physical patients with patellofemoral examination, and how would you diagnose and treat her? instability to assess for osseous trauma/deformity; consider MRI if nee pain is a common presentation in primary care. While you suspect significant soft-tissue traumatic knee pain is frequently addressed in the medical damage or the patient does not literature, little has been written about chronic nontrau- respond to conservative therapy. C K matic nonarthritic knee pain such as Jane’s. -

Prevalence of Pathologic Plica Following Anterior Cruciate Ligament Injury Deniz Aydın1 , Barış Polat2
DOI: 10.5152/cjms.2020.2133 Original Article Prevalence of Pathologic Plica Following Anterior Cruciate Ligament Injury Deniz Aydın1 , Barış Polat2 1Department of Orthopaedic Surgery, Near East University, School of Medicine, Nicosia, Cyprus 2Department of Orthopaedic Surgery, Dr. Burhan Nalbantoğlu Public Hospital, Nicosia, Cyprus ORCID iDs of the authors: D.A. 0000-0003-4148-1421; B.P. 0000-0001-8229-6412. Cite this article as: Aydın D, Polat B. Prevalence of Pathologic Plica Following Anterior Cruciate Ligament Injury. Cyprus J Med Sci 2020; 5(4): 327-32. BACKGROUND/AIMS The present study was designed to determine the relationship between the time from anterior cruciate ligament injury to operation as well as the presence of pathologic plica. We also assessed the relationship between the presence of pathologic plica and plica-associ- ated cartilage injury as well as preoperative anterior knee pain. MATERIAL and METHODS All the data for this retrospective observational study was obtained from hospital records and arthroscopy videos. Preoperative com- plaints, such as giving-way episodes, anterior knee pain, and knee locking, and intraoperative findings, such as the presence and ab- sence of the pathologic plica, cartilage injury, and meniscus lesion were evaluated. Patients operated within 3 mon of the injury and those operated ≥ 3 mon after the injury were classified into Group 1 and Group 2, respectively. RESULTS We enrolled 76 patients; group 1 included 46 patients, and group 2 comprised 30 patients; all the patients underwent anterior cruciate ligament reconstruction. The rate of preoperative anterior knee pain and pathologic plica formation was significantly higher in group 2 (p<0.05) as compared to that in group 1. -

Knee Health Promotion Option for Osteoarthritic Knee: Cartilage Regeneration Is Possible
21 Knee Health Promotion Option for Osteoarthritic Knee: Cartilage Regeneration is Possible S.R. Lyu1, D.S. Liu2, C.E. Tseng1, H.S. Wang3 and L.K. Chau2 1Tzu-Chi Dalin General Hospital, Tzu-Chi University, 2Chung Cheng University, 3Yang-Ming University Taiwan 1. Introduction Although articular hyaline cartilage was typically considered having no or low potential for regeneration (Zhang L et al., 2009), some still thought that it does have the capacity to grow and remodel extensively during pre- and post-natal development and after trauma (Onyekwelu I et al., 2009). Both direct and indirect evidence of articular cartilage regeneration have been observed by some authors after correction of varus deformity for osteoarthritis of the knee (Kanamiya T et al., 2002; Koshino T et al., 2003). Moreover, unlike the first impression of a more or less static tissue, articular cartilage shows a slow turnover. Anabolic and catabolic pathways were thought to be very much intermingled in articular cartilage (Aigner T et al., 2006). Thus, one of the most important questions in osteoarthritis research is to understand the balance of catabolic and anabolic factors in articular cartilage as this is the key to understand the biology of cartilage maintenance and degeneration. Osteoarthritis (OA) of the knee is the major cause of chronic musculoskeletal pain and is ranked as a main cause of mobility disability in elderly population. It is a disease process of uncertain multifactorial etiology, which eventually affects the entire joint. Various etiologic risk factors have been proposed, but the exact pathogenesis for OA knee is still unknown. Many literatures mentioned medial compartment is more commonly involved than the lateral one and the pathogenesis may be different (Neame R et al., 2004; Nunez M et al., 2008). -

Foot Strike and Injury Rates in Endurance Runners: a Retrospective Study
Foot Strike and Injury Rates in Endurance Runners: A Retrospective Study ADAM I. DAOUD1, GARY J. GEISSLER2, FRANK WANG3, JASON SARETSKY2, YAHYA A. DAOUD4, and DANIEL E. LIEBERMAN1 1Department of Human Evolutionary Biology, Harvard University, Cambridge, MA; 2Department of Athletics, Harvard University, Boston, MA; 3University Health Services, Harvard University, Cambridge, MA; and 4Baylor Health Care System, Institute of Health Care Research and Improvement, Dallas, TX ABSTRACT DAOUD, A. I., G. J. GEISSLER, F. WANG, J. SARETSKY, Y. A. DAOUD, and D. E. LIEBERMAN. Foot Strike and Injury Rates in Endurance Runners: A Retrospective Study. Med. Sci. Sports Exerc., Vol. 44, No. 7, pp. 1325–1334, 2012. Purpose: This retrospective study tests if runners who habitually forefoot strike have different rates of injury than runners who habitually rearfoot strike. Methods: We measured the strike characteristics of middle- and long-distance runners from a collegiate cross-country team and quantified their history of injury, including the incidence and rate of specific injuries, the severity of each injury, and the rate of mild, moderate, and severe injuries per mile run. Results: Of the 52 runners studied, 36 (69%) primarily used a rearfoot strike and 16 (31%) primarily used a forefoot strike. Approximately 74% of runners experienced a moderate or severe injury each year, but those who habitually rearfoot strike had approximately twice the rate of repetitive stress injuries than individuals who habitually forefoot strike. Traumatic injury rates were not significantly different between the two groups. A generalized linear model showed that strike type, sex, race distance, and average miles per week each correlate significantly (P G 0.01) with repetitive injury rates. -

January 1992
Rheumors Volume 3, Number 1 January, 1992 POINTS ON JOINTS The . thigh . bone . connected . to . the . shin . bone . Not all joint region pain is due to arthritis. Several future Points on Joints sections will be devoted to soft tissue (non-joint related) pain. This article will address the knee. ANSERINE BURSITIS: (Latin for goosefoot bursitis) is seen predominately in overweight, middle-aged or elderly women with big legs and osteoarthritis of the knees. Inflammation of the anserine bursa (Latin for sac) produces pain over the inner aspect of the knee about two inches below the joint. Treatment includes rest, corticosteroid injections into the bursa, exercise and weight reduction. PREPATELLAR BURSITIS: This is manifested by swelling over the kneecap and may result from trauma or infection. Frequent kneeling, such as in scrubbing floors, may lead to prepatellar bursitis lending to the name "housemaid's knee". Treatment may include aspiration of the bursae, anti-inflammatory drugs, heat, rest, and injection of steroids. Infection should be treated with an appropriate antibiotic. MEDIAL PLICA SYNDROME: A plica is a normal synovial fold (a folding of the inner lining of the joint) of the knee joint and can be seen under and above the kneecap, and on the medial (inner) aspect of the knee. The inner plica is especially liable to cause pain. The diagnosis must be suspected when other causes of knee pain are excluded. Diagnosis is confirmed by knee arthroscopy. PATELLOFEMORAL PAIN SYNDROME: This syndrome consists of pain, a grinding sensation in the region of the kneecap, and stiffness occurring after prolonged sitting.