Patellofemoral Pain in Athletes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
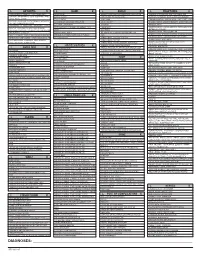
ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -

Hallux Valgus
MedicalContinuing Education Building Your FOOTWEAR PRACTICE Objectives 1) To be able to identify and evaluate the hallux abductovalgus deformity and associated pedal conditions 2) To know the current theory of etiology and pathomechanics of hallux valgus. 3) To know the results of recent Hallux Valgus empirical studies of the manage- ment of hallux valgus. Assessment and 4) To be aware of the role of conservative management, faulty footwear in the develop- ment of hallux valgus deformity. and the role of faulty footwear. 5) To know the pedorthic man- agement of hallux valgus and to be cognizant of the 10 rules for proper shoe fit. 6) To be familiar with all aspects of non-surgical management of hallux valgus and associated de- formities. Welcome to Podiatry Management’s CME Instructional program. Our journal has been approved as a sponsor of Continu- ing Medical Education by the Council on Podiatric Medical Education. You may enroll: 1) on a per issue basis (at $15 per topic) or 2) per year, for the special introductory rate of $99 (you save $51). You may submit the answer sheet, along with the other information requested, via mail, fax, or phone. In the near future, you may be able to submit via the Internet. If you correctly answer seventy (70%) of the questions correctly, you will receive a certificate attesting to your earned credits. You will also receive a record of any incorrectly answered questions. If you score less than 70%, you can retake the test at no additional cost. A list of states currently honoring CPME approved credits is listed on pg. -

Saethre-Chotzen Syndrome
Saethre-Chotzen syndrome Authors: Professor L. Clauser1 and Doctor M. Galié Creation Date: June 2002 Update: July 2004 Scientific Editor: Professor Raoul CM. Hennekam 1Department of craniomaxillofacial surgery, St. Anna Hospital and University, Corso Giovecca, 203, 44100 Ferrara, Italy. [email protected] Abstract Keywords Disease name and synonyms Excluded diseases Definition Prevalence Management including treatment Etiology Diagnostic methods Genetic counseling Antenatal diagnosis Unresolved questions References Abstract Saethre-Chotzen Syndrome (SCS) is an inherited craniosynostotic condition, with both premature fusion of cranial sutures (craniostenosis) and limb abnormalities. The most common clinical features, present in more than a third of patients, consist of coronal synostosis, brachycephaly, low frontal hairline, facial asymmetry, hypertelorism, broad halluces, and clinodactyly. The estimated birth incidence is 1/25,000 to 1/50,000 but because the phenotype can be very mild, the entity is likely to be underdiagnosed. SCS is inherited as an autosomal dominant trait with a high penetrance and variable expression. The TWIST gene located at chromosome 7p21-p22, is responsible for SCS and encodes a transcription factor regulating head mesenchyme cell development during cranial tube formation. Some patients with an overlapping SCS phenotype have mutations in the FGFR3 (fibroblast growth factor receptor 3) gene; especially the Pro250Arg mutation in FGFR3 (Muenke syndrome) can resemble SCS to a great extent. Significant intrafamilial -
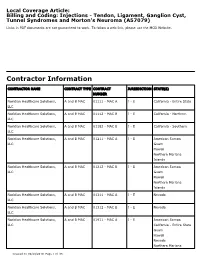
Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079)
Local Coverage Article: Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, A and B MAC 01111 - MAC A J - E California - Entire State LLC Noridian Healthcare Solutions, A and B MAC 01112 - MAC B J - E California - Northern LLC Noridian Healthcare Solutions, A and B MAC 01182 - MAC B J - E California - Southern LLC Noridian Healthcare Solutions, A and B MAC 01211 - MAC A J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01212 - MAC B J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01311 - MAC A J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01312 - MAC B J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01911 - MAC A J - E American Samoa LLC California - Entire State Guam Hawaii Nevada Northern Mariana Created on 09/28/2019. Page 1 of 33 CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Islands Article Information General Information Original Effective Date 10/01/2019 Article ID Revision Effective Date A57079 N/A Article Title Revision Ending Date Billing and Coding: Injections - Tendon, Ligament, N/A Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma Retirement Date N/A Article Type Billing and Coding AMA CPT / ADA CDT / AHA NUBC Copyright Statement CPT codes, descriptions and other data only are copyright 2018 American Medical Association. -

Angular Limb Deformities in Foals: Treatment and Prognosis*
Article #4 CE Angular Limb Deformities in Foals: Treatment and Prognosis* Nicolai Jansson, DVM, PhD, DECVS Skara Equine Hospital Skara, Sweden Norm G. Ducharme, DVM, MSc, DACVS Cornell University ABSTRACT: This article presents an overview of the clinical management of foals with angular limb deformities. Both conservative and surgical treatment options exist; the choice of which to use should be based on the type, severity, and location of the deformity as well as the age of the foal. Conservative measures include controlled exercise, rigid external limb support, and corrective hoof trimming. Surgical treatment modalities comprise tech- niques for manipulating physeal growth and, after physeal closure, various corrective osteotomy or ostectomy methods. The prognosis is generally good if treatment is initi- ated well in advance of physeal closure. ngular limb deformities and their treat- Conservative Treatment ment in foals and young horses constitute In most foals born with mild to moderate a significant part of the orthopedic prob- angular deformities, spontaneous resolution A 2 lems that veterinarians must manage. This article occurs within the first 2 to 4 weeks of life. In discusses the clinical management and prognosis newborn foals, periarticular laxity is the most of these postural deformities. likely cause, and these foals require no special treatment other than a short period of con- TREATMENT trolled exercise. In our opinion, mildly and The absence of controlled studies has moderately affected foals should not be confined impaired the accumulation of scientific data to a stall because exercise is important for nor- guiding the management of angular limb defor- mal muscular development and resolution of the mities in foals (Table 1). -

Conformational Limb Abnormalities and Corrective Farriery for Foals
Conformational Limb Abnormalities and Corrective Farriery for Foals For the past couple of years the general public has questioned the horse industry, and one of the questions is “Are we breeding horses more prone to breakdown with injuries”? It seems that we hear more often now that there are more leg and foot problems than ever before. Is it that we are more aware of conformational deficits and limb deviations, or are there some underlying factors that make our horses prone to injury? To improve, or even just maintain the breed, racing should prove soundness as well as speed and stamina. 1 The male side is usually removed from the bloodline if unable to produce good results at the racetrack. However, the female may have such poor conformation that she never even gets into training, but yet she enters the broodmare band. The generational effect of this must surely lead to an increase in the number of conformational deficits in our foals and yearlings.1 Something that we hear quite often is “Whoever saw the perfect horse”? and “There are plenty of horses with poor conformation that win races”. That doesn’t mean we should not continue to attempt to produce horses with good conformation. There is an acceptable range of deviation from the ideal, and therefore these deformities have to be accepted if it does not jeopardize the overall athletic soundness of the horse. Although mild conformational deficits may not significantly impact soundness, more significant limb deformities cause abnormal limb loading, lameness, gait abnormalities, and interference issues. 2 Developmental deformities of the limb include angular, flexural, and rotational limb deformities. -

Arthrogryposis Multiplex Congenita Part 1: Clinical and Electromyographic Aspects
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.35.4.425 on 1 August 1972. Downloaded from Journal ofNeurology, Neurosurgery, anid Psychiatry, 1972, 35, 425-434 Arthrogryposis multiplex congenita Part 1: Clinical and electromyographic aspects E. P. BHARUCHA, S. S. PANDYA, AND DARAB K. DASTUR From the Children's Orthopaedic Hospital, and the Neuropathology Unit, J.J. Group of Hospitals, Bombay-8, India SUMMARY Sixteen cases with arthrogryposis multiplex congenita were examined clinically and electromyographically; three of them were re-examined later. Joint deformities were present in all extremities in 13 of the cases; in eight there was some degree of mental retardation. In two cases, there was clinical and electromyographic evidence of a myopathic disorder. In the majority, the appearances of the shoulder-neck region suggested a developmental defect. At the same time, selective weakness of muscles innervated by C5-C6 segments suggested a neuropathic disturbance. EMG revealed, in eight of 13 cases, clear evidence of denervation of muscles, but without any regenerative activity. The non-progressive nature of this disorder and capacity for improvement in muscle bulk and power suggest that denervation alone cannot explain the process. Re-examination of three patients after two to three years revealed persistence of the major deformities and muscle Protected by copyright. weakness noted earlier, with no appreciable deterioration. Otto (1841) appears to have been the first to ventricles, have been described (Adams, Denny- recognize this condition. Decades later, Magnus Brown, and Pearson, 1953; Fowler, 1959), in (1903) described it as multiple congenital con- addition to the spinal cord changes. -

Osteotomy Around the Knee: Evolution, Principles and Results
Knee Surg Sports Traumatol Arthrosc DOI 10.1007/s00167-012-2206-0 KNEE Osteotomy around the knee: evolution, principles and results J. O. Smith • A. J. Wilson • N. P. Thomas Received: 8 June 2012 / Accepted: 3 September 2012 Ó Springer-Verlag 2012 Abstract to other complex joint surface and meniscal cartilage Purpose This article summarises the history and evolu- surgery. tion of osteotomy around the knee, examining the changes Level of evidence V. in principles, operative technique and results over three distinct periods: Historical (pre 1940), Modern Early Years Keywords Tibia Osteotomy Knee Evolution Á Á Á Á (1940–2000) and Modern Later Years (2000–Present). We History Results Principles Á Á aim to place the technique in historical context and to demonstrate its evolution into a validated procedure with beneficial outcomes whose use can be justified for specific Introduction indications. Materials and methods A thorough literature review was The concept of osteotomy for the treatment of limb defor- performed to identify the important steps in the develop- mity has been in existence for more than 2,000 years, and ment of osteotomy around the knee. more recently pain has become an additional indication. Results The indications and surgical technique for knee The basic principle of osteotomy (osteo = bone, tomy = osteotomy have never been standardised, and historically, cut) is to induce a surgical transection of a bone to allow the results were unpredictable and at times poor. These realignment and a consequent transfer of weight bearing factors, combined with the success of knee arthroplasty from a damaged area to an undamaged area of joint surface. -

Does the Patellofemoral Joint Need Articular Cartilage?—Clinical Relevance
Review Article Page 1 of 6 Does the patellofemoral joint need articular cartilage?—clinical relevance Lars Blønd1,2 1Department of Orthopaedic Surgery, Aleris-Hamlet Parken, Copenhagen, Denmark; 2Department of Orthopaedic Surgery, The Zealand University Hospital, Koege, Denmark Correspondence to: Lars Blønd, MD. Falkevej 6, 2670 Greve Strand, Denmark. Email: [email protected]. Abstract: The patellofemoral joint (PFJ) is enigmatic and we know the pathomorphology for anterior knee pain (AKP) is multifaceted. This paper review alignment and biomechanical factors associated with AKP both in the younger generation with or without cartilage changes and discusses the importance or obscurity of cartilage in the PFJ pathoanatomic changes such as trochlear dysplasia (TD), patella alta, increased femoral anteversion, lateralized tibial tubercle, external tibial torsion and valgus deformity affects the patellofemoral articulation. In order to achieve effective and durable results, it is of importance that any significant deviation in patellofemoral alignment should be corrected by realignment surgery, before considering cartilage procedures in the PFJ Patellofemoral alignment factors in both the frontal plane, the transverse plane and as well as the sagittal plan needs to evaluated thoroughly by not only clinical examination and X-ray, but also by MRI scans or CT scans. Keywords: Patellofemoral; malalignment; cartilage repair; anterior knee pain (AKP); trochlear dysplasia (TD); osteoarthritis Received: 01 January 2018; Accepted: 02 May 2018; Published: 24 May 2018. doi: 10.21037/aoj.2018.05.01 View this article at: http://dx.doi.org/10.21037/aoj.2018.05.01 The patellofemoral joint (PFJ) is enigmatic and we know not established the precise link between pain and cartilage the pathomorphology for anterior knee pain (AKP) is lesions (1). -

Expanded Indications for Guided Growth in Pediatric Extremities
Current Concept Review Expanded Indications for Guided Growth in Pediatric Extremities Teresa Cappello, MD Shriners Hospitals for Children, Chicago, IL Abstract: Guided growth for coronal plane knee deformity has successfully historically been utilized for knee val- gus and knee varus. More recent use of this technique has expanded its indications to correct other lower and upper extremity deformities such as hallux valgus, hindfoot calcaneus, ankle valgus and equinus, rotational abnormalities of the lower extremity, knee flexion, coxa valga, and distal radius deformity. Guiding the growth of the extremity can be successful and is a low morbidity method for correcting deformity and should be considered early in the treatment of these conditions when the child has a minimum of 2 years of growth remaining. Further expansion of the application of this concept in the treatment of pediatric limb deformities should be considered. Key Concepts: • Guiding the growth of pediatric physes can successfully correct a variety of angular and potentially rotational deformities of the extremities. • Guided growth can be performed using a variety of techniques, from permanent partial epiphysiodesis to tem- porary methods utilizing staples, screws, or plate and screw constructs. • Utilizing the potential of growth in the pediatric population, guided growth principals have even been success- fully applied to correct deformities such as knee flexion contractures, hip dysplasia, femoral anteversion, ankle deformities, hallux valgus, and distal radius deformity. Introduction Guiding the growth of pediatric orthopaedic deformities other indications and uses for guided growth that may is represented by the symbol of orthopaedics itself, as not have wide appreciation. the growth of a tree is guided as it is tethered to a post (Figure 1). -

Which Osteotomy for a Valgus Knee?
International Orthopaedics (SICOT) (2010) 34:239–247 DOI 10.1007/s00264-009-0820-3 ORIGINAL PAPER Which osteotomy for a valgus knee? Giancarlo Puddu & Massimo Cipolla & Guglielmo Cerullo & Vittorio Franco & Enrico Giannì Received: 2 April 2009 /Revised: 18 May 2009 /Accepted: 18 May 2009 /Published online: 23 June 2009 # Springer-Verlag 2009 Abstract A valgus knee is a disabling condition that can The young patient with knee OA or with an initial affect patients of all ages. Antivalgus osteotomy of the knee condral pathology presents a challenging treatment dilem- is the treatment of choice to correct the valgus, to eliminate ma to the orthopaedic surgeon. A valgus painful knee is a pain in the young or middle age patient, and to avoid or disabling condition that can affect patients of all ages. Anti- delay a total knee replacement. A distal femoral lateral valgus osteotomies are the treatment of choice to correct the opening wedge procedure appears to be one of the choices valgus deformity and eliminate pain and other functional for medium or large corrections and is particularly easy and problems. In particular, patients with an early arthritis of the precise if compared to the medial femoral closing wedge lateral femoro-tibial compartment or damage of the carti- osteotomy. However, if the deformity is minimal, a tibial lage of the lateral femoral condyle are candidates for anti- medial closing wedge osteotomy can be done with a faster valgus osteotomies. Both the lateral femoral condyle and healing and a short recovery time. the lateral tibial plateau have convex surfaces, the congru- ence of which is maintained thanks to the integrity of the lateral meniscus. -

Patellofemoral SMCA 2014 Handout
Patellofemoral Pain Syndrome / How can a Sesamoid Bone Anterior Knee Pain / Runners’ Knee cause So Many Problems? _ n Most common cause of Patellofemoral Pain and knee pain Patella Instability n Most common symptom presenting to SM n Diagnostic challenge n Treatment controversies n Lack of evidence to support Sarah Kerslake BPHTY Ax and Rx PFPS Patellofemoral Anatomy n Multifactorial Etiology n Considering the PF joint is one of the most n Non-operative treatment is successful highly loaded joints in the human body, the prevalence of AKP is not surprising. n Strong evidence supports treatment with multimodal therapy n Anatomy: n Sesamoid bone in extensor apparatus n Routine clinical Ax of muscle strength in athletes may not detect deficits n Acts as pulley/cam in extensor mechanism n Protects the tibiofemoral joint n More challenging functional tests required n Anchored by Active and Passive elements PFPS Anatomy PFPS Anatomy n Active (Dynamic) restraints n Passive (Static) restraints n Quadriceps muscle n Bony anatomy (Facets <=> Trochlea) n Vastus Lateralis Obliquus/Longus n Quadriceps Fascia + Patellar Tendon n Rectus Femoris + Vastus Intermedius n Lateral Peripatellar Retinaculum n Vastus Medialis Obliquus/Longus n Medial Peripatellar Retinaculum, particularly n Patella Tendon the medial patellofemoral ligament n Iliotibial band n Balance between structures is v. important 1 PFPS Symptoms PFPS Pathology n Symptoms include pain, swelling, n Patellar Tracking weakness, instability, mechanical n Patellar Tendinopathy symptoms & functional